Abstract
This study investigated the effects of Lacticaseibacillus paracasei K56 (L. paracasei K56) on body weight, body composition, and glycolipid metabolism in mice with high-fat diet-induced obesity and explored the underlying mechanisms. Male C57BL/6J mice were fed a high-fat diet for 8 weeks to induce obesity; then, the obese mice were gavaged with or without L. paracasei K56 for 10 weeks. The body weight, body composition, fat mass, blood lipid, blood glucose, and hormones of the mice were evaluated. Moreover, the fatty acid synthesis (FAS) and peroxisome proliferator-activated receptor γ (PPAR-γ) expressions in the liver were detected via Western blotting. 16S rRNA gene sequencing was adopted to determine the gut microbiota alterations. The high-fat diet successfully induced obesity, as indicated by the abnormal increase in body weight, visceral fat, fat mass, blood lipids, fasting blood glucose, and insulin-resistance. Moreover, the FAS expression in the liver was significantly increased, whereas the PPAR-γ expression was significantly decreased. The relative abundance of Proteobacteria, Actinobacteria and Patescibacteria was also significantly increased, and that of Verrucomicrobia was significantly decreased. However, these indicators of mice supplemented with L. paracasei K56 were significantly opposite to those of obese mice. The Ruminococcuaceae_UCG-013, Akkermansia, Prevotellaceae_UCG-001, Muribaculum, and Lachnospiraceae_NK4A136 groups were significantly negatively correlated with body weight, blood lipids, and blood glucose-related indicators, whereas Coriobacteriaceae_UCG-002, Enterorhabdus, Raoultibacter, Acinetobacter, Romboutsia, Leuconostoc, and Erysipelatoclostridium were significantly positively correlated with these indicators. L. paracasei K56 might be a promising probiotic strain that could effectively slow down the body weight gain, reduce fat accumulation, alleviate insulin-resistance, and restore pancreatic β-cell function in obese mice by regulating the gut microbiota.







Similar content being viewed by others
Data Availability
All data included in this study are available upon request by contact with the corresponding author. Raw reads of 16S rRNA sequencing data is submitted to Sequence Read Archive (SRA) under the BioProject ID PRJNA722791 in NCBI.
References
GBD 2015 Obesity Collaborators (2017) Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med 377(1):13–27. https://doi.org/10.1056/NEJMoa1614362
Blüher M (2019) Obesity: global epidemiology and pathogenesis. Nat Rev Endocrinol 15(5):288–298. https://doi.org/10.1038/s41574-019-0176-8
Rothschild D, Weissbrod O, Barkan E et al (2018) Environment dominates over host genetics in shaping human gut microbiota. Nature 555(7695):210–215. https://doi.org/10.1038/nature25973
Gomes AC, Hoffmann C, Mota JF (2018) The human gut microbiota: metabolism and perspective in obesity. Gut Microbes 9(4):308–325. https://doi.org/10.1080/19490976.2018.1465157
Green M, Arora K, Prakash S (2020) Microbial medicine: prebiotic and probiotic functional foods to target obesity and metabolic syndrome. Int J Mol Sci 21(8). https://doi.org/10.3390/ijms21082890
Castaneda-Marquez AC, Diaz-Benitez C, Bahena-Roman M et al (2020) Lactobacillus paracasei as a protective factor of obesity induced by an unhealthy diet in children. Obes Res Clin Pract 14(3):271–278. https://doi.org/10.1016/j.orcp.2020.04.005
Cheng MC, Tsai TY, Pan TM (2015) Anti-obesity activity of the water extract of Lactobacillus paracasei subsp. paracasei NTU 101 fermented soy milk products. Food Funct 6(11):3522–3530. https://doi.org/10.1039/c5fo00531k
Tanida M, Shen J, Maeda K et al (2008) High-fat diet-induced obesity is attenuated by probiotic strain Lactobacillus paracasei ST11 (NCC2461) in rats. Obes Res Clin Pract 2(3):159–169. https://doi.org/10.1016/j.orcp.2008.04.003
Cui XW, Shi YY, Gao SY et al (2019) Effects of Lactobacillus reuteri DSM 17938 in preterm infants: a double-blinded randomized controlled study. Ital J Pediatr 45(1):140. https://doi.org/10.1186/s13052-019-0716-9
Lai HH, Chiu CH, Kong MS et al (2019) Probiotic Lactobacillus casei: effective for managing childhood diarrhea by altering gut microbiota and attenuating fecal inflammatory markers. Nutrients 11(5):1150. https://doi.org/10.3390/nu11051150
Cheng RY, Guo JW, Pu FF et al (2019) Loading ceftriaxone, vancomycin, and Bifidobacteria bifidum TMC3115 to neonatal mice could differently and consequently affect intestinal microbiota and immunity in adulthood. Sci Rep 9(1):3254. https://doi.org/10.1038/s41598-018-35737-1
Meng L, Duan S, Situ W et al (2020) Probiotic edible composition useful in preparing food for promoting digestive function, comprises Bifidobacterium lactis BL-99, Lactobacillus paracasei K56 and Lactobacillus paracasei ET-2. In.: Inner Mongolia Yili Ind Group Co Ltd. Patent Number: CN110903995-A
Min QQ, Sun T, Xu JY et al (2021) Differential modulation of the metabolic effects of diet-induced obesity by probiotic Lactobacillus Paracasei K56 and prebiotic alpha-galactooligosaccharides. Curr Top Nutraceutical Res 19(1):21–28. https://doi.org/10.37290/ctnr2641-452X.19:21-28
Jayashree B, Bibin YS, Prabhu D et al (2014) Increased circulatory levels of lipopolysaccharide (LPS) and zonulin signify novel biomarkers of proinflammation in patients with type 2 diabetes. Mol Cell Biochem 388(1–2):203–210. https://doi.org/10.1007/s11010-013-1911-4
Mulders RJ, de Git KCG, Schele E et al (2018) Microbiota in obesity: interactions with enteroendocrine, immune and central nervous systems. Obes Rev 19(4):435–451. https://doi.org/10.1111/obr.12661
Zhao D, Zhu H, Gao F et al (2020) Antidiabetic effects of selenium-enriched Bifidobacterium longum DD98 in type 2 diabetes model of mice. Food Funct 11(7):6528–6541. https://doi.org/10.1039/d0fo00180e
Turnbaugh PJ, Ley RE, Mahowald MA et al (2006) An obesity-associated gut microbiome with increased capacity for energy harvest. Nature 444(7122):1027–1031. https://doi.org/10.1038/nature05414
Ranganathan G, Unal R, Pokrovskaya I et al (2006) The lipogenic enzymes DGAT1, FAS, and LPL in adipose tissue: effects of obesity, insulin resistance, and TZD treatment. J Lipid Res 47(11):2444–2450. https://doi.org/10.1194/jlr.M600248-JLR200
Janani C, Ranjitha Kumari BD (2015) PPAR gamma gene–a review. Diabetes Metab Syndr 9(1):46–50. https://doi.org/10.1016/j.dsx.2014.09.015
Chang CJ, Lin CS, Lu CC et al (2015) Ganoderma lucidum reduces obesity in mice by modulating the composition of the gut microbiota. Nat Commun 6:7489. https://doi.org/10.1038/ncomms8489
Zhang T, Li QQ, Cheng L et al (2019) Akkermansia muciniphila is a promising probiotic. Microb Biotechnol 12(6):1109–1125. https://doi.org/10.1111/1751-7915.13410
Massier L, Chakaroun R, Tabei S et al (2020) Adipose tissue derived bacteria are associated with inflammation in obesity and type 2 diabetes. Gut 69(10):1796–1806. https://doi.org/10.1136/gutjnl-2019-320118
Amorim AM, Nascimento JD (2017) Acinetobacter: an underrated foodborne pathogen?. J Infect Dev Countr 11(2):111–114. https://doi.org/10.3855/jidc.8418
Zhou HX, Tai JJ, Xu HY et al (2019) Xanthoceraside could ameliorate Alzheimer’s disease symptoms of rats by affecting the gut microbiota composition and modulating the endogenous metabolite levels. Front Pharmacol 10:1035. https://doi.org/10.3389/fphar.2019.01035
Mu HN, Zhou Q, Yang RY et al (2020) Naringin attenuates high fat diet induced non-alcoholic fatty liver disease and gut bacterial dysbiosis in mice. Front Microbiol 11:585066. https://doi.org/10.3389/fmicb.2020.585066
Lee CJ, Sears CL, Maruthur N (2020) Gut microbiome and its role in obesity and insulin resistance. Ann Ny Acad Sci 1461(1):37–52. https://doi.org/10.1111/nyas.14107
Milosevic I, Vujovic A, Barac A et al (2019) Gut-liver axis, gut microbiota, and its modulation in the management of liver diseases: a review of the literature. Int J Mol Sci 20(2). https://doi.org/10.3390/ijms20020395
Zhou JC, Zhang XW (2019) Akkermansia muciniphila: a promising target for the therapy of metabolic syndrome and related diseases. Chin J Nat Medicines 17:835–841. https://doi.org/10.1016/S1875-5364(19)30101-3
Song XF, Zhong L, Lyu N et al (2019) Inulin can alleviate metabolism disorders in ob/ob mice by partially restoring leptin-related pathways mediated by gut microbiota. Genom Proteom Bioinf 17(1):64–75. https://doi.org/10.1016/j.gpb.2019.03.001
Koh A, De Vadder F, Kovatcheva-Datchary P et al (2016) From dietary fiber to host physiology: short-chain fatty acids as key bacterial metabolites. Cell 165(6):1332–1345. https://doi.org/10.1016/j.cell.2016.05.041
Sinha SR, Haileselassie Y, Nguyen LP et al (2020) Dysbiosis-induced secondary bile acid deficiency promotes intestinal inflammation. Cell Host Microbe 27(4):659-670.e655. https://doi.org/10.1016/j.chom.2020.01.021
Liang HJ, Jiang FL, Cheng RY et al (2021) A high-fat diet and high-fat and high-cholesterol diet may affect glucose and lipid metabolism differentially through gut microbiota in mice. Exp Anim 70(1):73–83. https://doi.org/10.1538/expanim.20-0094
Vallim TQD, Tarling EJ, Edwards PA (2013) Pleiotropic roles of bile acids in metabolism. Cell Metab 17(5):657–669. https://doi.org/10.1016/j.cmet.2013.03.013
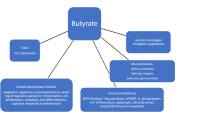
He B, Moreau R (2019) Lipid-regulating properties of butyric acid and 4-phenylbutyric acid: molecular mechanisms and therapeutic applications. Pharmacol Res 144:116–131. https://doi.org/10.1016/j.phrs.2019.04.002
Acknowledgements
The authors would like to thank GENE DENOVO for providing assistance in bioinformatic analysis. We appreciated the Enago (http://www.enago.jp) for the English language review.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Miao, Z., Zheng, H., Liu, WH. et al. Lacticaseibacillus paracasei K56 Attenuates High-Fat Diet-Induced Obesity by Modulating the Gut Microbiota in Mice. Probiotics & Antimicro. Prot. 15, 844–855 (2023). https://doi.org/10.1007/s12602-022-09911-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12602-022-09911-x