Abstract
Neural and humoral autonomic mechanisms may be important in the maintenance of blood flow in the masseter muscle (MBF). However, their interactions remain unclear. In this study, we examined interactions between neural and humoral regulation of MBF and investigated the mechanisms mediating these interactions in urethane-anesthetized rats. Stimulation of the adrenal nerve (AN) projecting to the adrenal medulla increased MBF, and this increase was mediated by β-adrenoceptors. Sectioning of the superior cervical sympathetic trunk (CST) significantly inhibited increases in MBF induced by AN stimulation during high activity in the CST, but not during low activity. AN stimulation with clonidine after CST sectioning induced a significant increased in MBF, however phenylephrine had no observable effect. Pretreatment with yohimbine or propranolol significantly inhibited the increase in the MBF. Our results suggest an interaction between β-adrenergic vasodilation evoked by circulating adrenaline and the cervical sympathetic nerves that is mediated by α2-adrenoceptors in the masseter muscle.
Similar content being viewed by others
Introduction
The autonomic nervous system plays an important role in the regulation of the hemodynamics in jaw muscles, with the autonomic vasomotor responses evoked by neural and humoral mechanisms rapidly and markedly changing the blood flow in jaw muscles [1–3]. Parasympathetic vasodilation in jaw muscles, especially in the masseter muscle, is known to be evoked by a trigeminal [2] or a vagal-mediated reflex [4, 5]. However, sympathetic vasoconstriction is under tonic control from the superior cervical sympathetic trunk (CST) [6]. It has also been reported that the release of circulating adrenaline through activation of the sympathoadrenal system is involved in vasodilation in the masseter muscle through a β-adrenergic mechanism [7]. These observations suggest that neural and humoral autonomic mechanisms and their interactions may be important for the maintenance of blood flow in the masseter muscle (MBF) and the activity of the masseter muscle.
Stress and chronic pain associated with jaw muscle dysfunction, such as fibromyalgia, are known to modulate sympathetic nerve activity, inducing changes in the cardiovascular parameters, such as blood pressure and regional blood flow [8–10]. Sympathoexcitation can cause an increase or decrease in MBF [7, 11, 12]. For example, cold-pressor stimulation has been reported to induce an increase in intramuscular blood volume in the human masseter muscle [11], while acute stress, such as noise, air jets, and noxious cutaneous stimuli, has been found to reduce blood flow in the rabbit masseter muscle [12]. The reasons for these differences in the effects of such stimuli are not clear. However, the interaction between cervical sympathetic nerves (neural) and the sympathoadrenal system (humoral) may be involved in the regulation of MBF during sympathoexcitation. Details of the interaction between these mechanisms in the regulation of MBF are not fully understood.
In the study reported here, we explored (1) the effects of electrical stimulation of the peripheral cut end of the adrenal nerve (AN) branch from splanchnic nerve projecting into the adrenal medulla on MBF with either the intact or sectioned CST and (2) the underlying mechanisms mediating these responses in deeply urethane-anesthetized, artificially ventilated, and cervically vagotomized rats (Fig. 1).

Modified from Ishii et al. [7]
Schematic representation of the sites of electrical stimulation and blood flow measurement in rats. a Stimulation site at the peripheral cut end (i) of the adrenal nerve (AN), which is derived from the splanchnic nerve (SPLN). Blood flow was measured at the site of the masseter muscle (ii) and lower lip (iii) using a laser-Doppler flowmeter (LDF). Solid lines: iv Sympathetic preganglionic neurons projecting to the adrenal medulla through the AN, v sympathetic vasoconstrictor fibers to both the masseter muscle and lower lip from the superior cervical ganglion (SCG) of the cervical sympathetic trunk (CST). Dashed lines: vi Parasympathetic vasodilator fibers to the masseter muscle and lower lip from the salivatory nuclei (SN), vii trigeminal sensory inputs to the brainstem. LN Lingual nerve, OG otic ganglion, TG trigeminal ganglion, Vsp trigeminal spinal nucleus, V trigeminal nerve root, IX glossopharyngeal nerve root. b Photograph (left) and illustration (right) of the area indicated by the dashed rectangle in a showing the left AN to the adrenal gland in a supine rat. Arrowheads indicate the approximate site at which nerve was electrically stimulated. Scale bar 2 mm
Methods
Preparation of animals
The experiments were performed on 48 adult male Wistar rats between 9 and 16 weeks of age and weighing between 320 and 450 g each. After induction with inhalation anesthesia (isoflurane), urethane (1 g/kg in 1 ml/100 g body weight) was injected subcutaneously into the backs of the animals. One femoral vein was cannulated to allow drug injection, and one femoral artery was cannulated and connected to a Statham pressure transducer to monitor the systemic arterial blood pressure (SABP) and heart rate (HR). The anesthetized animals were intubated, paralyzed by an intravenous (iv) injection of pancuronium bromide (Mioblock; Organon Teknika, Oss, The Netherlands; 0.6 mg/kg initially, supplemented with 0.4 mg/kg every hour or so after testing the level of anesthesia; see following text), and artificially ventilated via a tracheal cannula with a mixture of 50% air and 50% O2. The ventilator (model SN-480-7; Shinano, Tokyo, Japan) was set to deliver a tidal volume of 8.5–10 cm3/kg at a rate of 20–23 breaths/min, and the end-tidal concentration of CO2 was determined by means of an infrared analyzer (Capnomac Ultima; Datex, Helsinki, Finland), as reported previously [2]. Continuous ventilation in this manner has been shown to maintain an end-tidal concentration of CO2 of 40–45 mmHg. The changes in the end-tidal CO2 following treatment (from 45 to 35 mmHg) were not responsible for the blood flow changes measured by the method used in this study(data not shown). Rectal temperature was maintained at 37–38 °C with the use of a heating pad. Before the injection of additional pancuronium bromide, the depth of anesthesia was determined as adequate by the absence of any flexion response to a noxious stimulus, such as pinching the digit for approximately 2 s. The criterion for the maintenance of an adequate depth of anesthesia following paralysis was defined as the absence of a reflexive elevation of SABP in response to the noxious stimulus. When the depth of anesthesia was considered to be inadequate, additional urethane (intermittent doses of 100 mg/kg, iv) was administered. At the end of the experiment, all rats were killed by an overdose (approximately 100 mg, iv) of pentobarbital sodium. Experimental protocols were reviewed and approved by the Animal Ethics and Research Committee of the University and were conducted in accordance with the Regulations for the Care and Use of Laboratory Animals of the Health Sciences University of Hokkaido (No. 021). All the animals were cared for in accordance with the recommendations in the current National Research Council guide.
Measurement of the blood flow and cardiovascular parameters
Changes in the blood flow of the bilateral MBF (n = 10) and lower lip blood flow (LBF) (n = 10) were monitored using a laser-Doppler flowmeter (Fig. 1) (LDF; model FLO-C1; Omegawave, Tokyo, Japan), as described elsewhere [2, 5–7, 13, 14]. The probes were placed against the masseter muscle after making incisions in the cheek and lower lip without exerting pressure on the tissue. The masseter muscle was ascertained by the naked eye. The LDF values obtained in this way represent the blood flow in the superficial vessels of the tissue [15, 16]. The analog output of the equipment did not provide absolute values, but showed relative changes in blood flow [in arbitrary units (a.u.)] (for technical details and an evaluation of the LDF method, see Stern et al. [17]). The SABP was recorded from a femoral catheter via a Statham pressure transducer. All data were collected online with a LabScribe2 data-acquisition system (iWorx Systems, Washington, NH). The HR and systolic, diastolic, and mean SABP were calculated from the SABP signals (n = 7). Vascular conductance (VC) was calculated using the following equation:
Changes in the averaged VC were assessed by measuring the maximum value in the responses.
Electrical stimulation of the AN
The peripheral cut end of the AN (Fig. 1), which regulates catecholamine secretion from the adrenal medulla [18–20], was stimulated electrically using a bipolar silver electrode attached to an electrical stimulator (model SEN-7103; Nihon Kohden, Tokyo, Japan). For this purpose, a midline abdominal incision was made, and the gut was carefully moved aside and covered with sterile gauze moistened with sterile saline (0.9% NaCl). With the use of a cotton swab, a major branch of the AN to the adrenal gland on the left side was cleaned of fat and exposed. Electrical stimulation of the AN was delivered for periods of 20 s with supramaximal voltage (10 V) at 20 Hz using 2-ms pulse durations [7] with either intact or sectioning of the CST in the neck (n = 10). In all experiments, the cervical vagi were cut bilaterally at the neck before stimulation, which ruled out the involvement of the visceral inputs through the cervical and abdominal vagus nerves.
Pharmacological agents
All drugs were dissolved in sterile saline. The agonist drugs were clonidine hydrochloride (n = 6; 2–10 μg/ml; Wako, Osaka, Japan) and phenylephrine hydrochloride (n = 6; 2–10 μg/ml; KOWA, Tokyo, Japan). The following pharmacological interventions were performed: (1) β-adrenergic blockade using propranolol hydrochloride (n = 6–10; 1 mg/ml; AstraZeneca, Osaka, Japan); (2) α2-adrenergic blockade using yohimbine hydrochloride (n = 6; 0.5 mg/ml; Sigma-Aldrich, St. Louis, MO). These drugs were perfused intravenously for 10 min at a flow rate of 0.1 ml/min using a syringe pump (Model ‘22’ Multisyringe; HARVARD, Holliston, MA). The adrenaline (n = 5; 100 ng/kg; DAIICHI SANKYO, Tokyo, Japan) was administered by bolus injections in volumes of 0.01–0.1 ml. The administration of a similar volume of saline had no measurable effect on the cardiovascular parameters (data not shown). The responses evoked by stimulation of the AN after the administration of various drugs were determined at least 5–10 min after the injection when changes in the blood flow and SABP had reached a steady state. The magnitude of the response after the administration of various drugs was compared with the control response recorded before the administration. The effectiveness of the blockade using yohimbine was assessed by the absence of a vasoconstrictor response to clonidine (10 μg/ml) (Fig. 5a). The effectiveness of the blockade using propranolol was assessed by the absence of a vasodilator response to isoproterenol hydrochloride (100 ng/kg; KOWA) (data not shown). The dose of adrenaline chosen for our study was 100 ng/kg, as this dose has been shown to produce a significant increase in MBF [7].
Reverse transcription-PCR analysis
The urethane-anesthetized rats were killed by cervical dislocation, and the masseter muscles and lower lips were excised and used for subsequent analyses (n = 5). The tissue was homogenized in 50 mg/ml of TRIzol/mRNA reagent (Gibco BRL, Grand Island, NY), and the total RNA was extracted as described in the protocol provided by the manufacturer. Total RNA (1 μg) from the tissue was used for the reverse transcription (RT)-PCR analyses in a final volume of 50 μl. The PCR amplifications were performed using specific primers for α-adrenoceptor isoforms (α1A, α2A, α2B, and α2C) as described in Table 1 [21]. The size of the expected fragments for each isoform was: α1A, 479 (range: 154–632) bp; α2A, 265 (1116–1380) bp; α2B, 396 (1481–1876) bp; α2C, 567 (2031–2597) bp. The RT-PCR was conducted using a one-step RT-PCR kit (Qiagen, Holden, Germany). Template RNA in each tube was reverse transcribed at 50 °C for 30 min, subjected to initial PCR activation at 95 °C for 15 min, and then subjected to PCR cycling (35-step cycle) consisting of denaturation at 94 °C for 1 min, annealing at 58 °C for 1 min, and extension at 72 °C for 1 min. A 10-μl portion of the amplified product was resolved on 2.0% agarose gels (NuSeive 3:1; FMC Products, Rockland, ME) containing 0.01% GelRed™ (Biotium, Fremont, CA), and the DNA was visualized by LED transillumination (Wako, Osaka, Japan). The gel images were captured by a digital camera, recorded on a Macintosh computer, and quantified using ImageJ 1.46r software. The products were normalized with that of the housekeeping gene, glyceraldehyde-3-phosphate dehydrogenase (GAPDH, 452 bp) from the same template and shown as a ratio [22].
Statistical analysis
All numerical data are presented as the mean ± the standard error of the mean. The statistical significance of the observed changes was assessed using the paired Student’s t test or analysis of variance (ANOVA) followed by a post hoc test [Fisher’s protected least significant difference (PLSD) test] and a contrast test. Differences were considered to be significant at P < 0.05. Data were analyzed using a Macintosh computer with StatView 5.0 (SAS Institute Inc., Cary, NC) and SuperANOVA (ABACUS Concepts, Berkeley, CA).
Results
Effects of electrical stimulation of the peripheral cut end of the AN on the hemodynamics in the masseter muscle and lower lip, and the SABP before and after sectioning of the CST
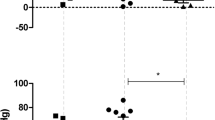
Figure 2 shows the effects of electrical stimulation of the left AN on the MBF on both sides, the LBF on the left side, the VC at each of the measuring sites, and SABP before and after sectioning of the left CST. Similar basal levels for MBF and LBF were recorded before the CST was sectioned (Fig. 2a, b). Before CST sectioning, AN stimulation resulted in significant increases in the MBF on both sides, but not in the LBF, and in a slight decrease in SABP (Figs. 2a, 3). Sectioning of the left CST resulted in a significant and a continuous increase in the basal level of the left MBF, but it had no effect on the right MBF (Figs. 2a, 3). The increased level of the MBF is comparable with the spontaneous activity in the CST fibers innervating the masseter vasculature as electrical stimulation of the peripheral cut end of the CST restored the basal level of the MBF to pre-sectioned values, as also demonstrated previously [6]. The increases in the basal level of the MBF were caused by either high or low spontaneous activity (5:2) in the CST (Fig. 2). The increases in MBF evoked by AN stimulation during high spontaneous activity in the CST were not observed at 5 min after ipsilateral CST sectioning, and AN stimulation decreased the MBF at 30 min after CST sectioning (Figs. 2a, 3). The increased in MBF during low spontaneous activity in the CST were evoked by AN stimulation regardless of the presence or absence of sympathetic innervation (Figs. 2b, 3). Changes in VC in the masseter muscle evoked by AN stimulation showed a negative correlation (r = −0.83) with changes in the baseline after CST sectioning (Fig. 2c). During the period of high spontaneous activity in the CST, there were significant differences in the left masseter muscle VC before and after the AN stimulation alone or CST sectioning (P < 0.001), but not after AN stimulation with CST sectioning (Fig. 3). On the right side, there were significant differences in the masseter muscle VC following AN stimulation regardless of the presence or absence of CST sectioning (P < 0.001) (Fig. 3). There was no significant difference between the increase of masseter muscle VC evoked by AN stimulation on the left and right side before CST sectioning (Fig. 3). The increase in the masseter muscle VC evoked by AN stimulation after CST sectioning in the right masseter muscle was significantly larger than that in the left masseter muscle (P < 0.001) (Fig. 3). The increases in the MBF and masseter muscle VC evoked by AN stimulation were inhibited significantly by the intravenous administration of propranolol (Fig. 3). The animals exhibited normal systolic and diastolic pressures, mean SABP, and HR during rest. The HR remained unchanged during all of the different treatments (Table 2). There were significant differences in the SABP before and after AN stimulation (P < 0.01) (Table 2). The HR at 10 min after the administration of propranolol was 305 ± 9 beats/min. The HR was significantly lower after the administration of propranolol than before its administration (P < 0.01). The mean SABP after the administration of propranolol was 117.8 ± 4.6 mmHg. There was no statistically significant difference in the mean SABP before and after propranolol administration.
Relationships between cervical sympathetic nerves and the sympathoadrenal system in the regulation of cardiovascular parameters in the rat. a Typical examples of the effects of electrical stimulation of the peripheral cut end of the left AN (at black horizontal bars) before and after (5–30 min) sectioning of the left CST (at arrow) on the blood flow in the masseter muscle (MBF) on both sides, lower lip (LBF) on the left side, vascular conductance (VC) of the measurement sites and systemic arterial blood pressure (SABP) during high spontaneous activity in the CST. Increases in the VC were assessed by measuring the height of peak (†) during the response. b Typical examples of the effects of the left AN stimulation before and after sectioning of the left CST on the left MBF and VC in the masseter muscle during low spontaneous activity in the CST. Electrical stimulation of the AN was delivered for 20 s with a supramaximal voltage (10 V) at 20 Hz using 2-ms pulses. Changes in blood flows (a.u. arbitrary units) and VC (a.u./mmHg) in the masseter muscle and lower lip and SABP were measured simultaneously. c Plot of changes in the VC evoked by AN stimulation vs. changes in the baseline VC after CST sectioning (*) in the masseter muscle. The white traces in a and b indicate the mean VC at the measuring sites
Inhibition by CST sectioning on the increases in the MBF evoked by activation of the sympathoadrenal system during high spontaneous activity in the CST. The mean ± standard error of the mean (SEM) of the changes (black bars) in the MBF on both sides, left LBF (top), and VC of each measuring site (bottom) evoked by electrical stimulation of the left AN (20 s, 10 V, 20 Hz, 2-ms pulses) alone (AN stim.), left CST sectioning (CSTs), and AN stimulation in combination with CST sectioning (CSTs + AN stim.) or propranolol (1 mg/ml; (AN stim. + Pro) (n = 10 in each group) are shown. Statistical significance of the differences from base value before AN stimulation was determined by analysis of variance (ANOVA) followed by a post hoc test [Fisher’s protected least significant difference (PLSD) test]. *P < 0.001 vs. base value. A significant difference between data sets (P < 0.05, P < 0.001) or non-significant difference (NS) is indicated above the appropriate square bracket (ANOVA followed by a contrast test)
Effects of exogenously applied adrenaline on the hemodynamics of the masseter muscle and SABP before and after CST sectioning during high spontaneous activity in the CST
Figure 4a shows the effects of the intravenous administration of adrenaline on the MBF and VC in the left masseter muscle and SABP before and after left CST sectioning. Before CST sectioning, adrenaline administration resulted in significant increases in the MBF, accompanied by a slight decrease in SABP (Fig. 4). The MBF increases evoked by adrenaline administration were significantly lower at 5 min after CST sectioning, and adrenaline administration produced a decrease in the MBF that persisted until 30 min after CST sectioning (Fig. 4). There were significant differences in the masseter muscle VC before and after adrenaline administration alone (P < 0.05), but its administration after CST sectioning had no significant effect on hemodynamics in the masseter muscle (Fig. 4b). The HR remained unchanged by the administration of adrenaline (425 ± 17 beats/min). Adrenaline administration caused slight decreases in the mean SABP (93.9 ± 5.7 mmHg), but there was no significant difference in the mean SABP before and after adrenaline administration.
Effects of exogenously applied adrenaline on the hemodynamics of the masseter muscle and on SABP during high spontaneous activity in the CST. a Typical examples are shown of the effect of intravenous administration of adrenaline (arrowheads, 100 ng/kg) on changes in the MBF and VC in the masseter muscle on the left side, and SABP before and after (5–30 min) the left CST sectioning (at arrow). The white traces indicate the mean VC for each record. b Mean ± SEM of changes (black bars) in the left MBF (top) and masseter muscle VC (bottom) evoked by adrenaline administration alone (Adrenaline) and 5 min after adrenaline administration in combination with CST sectioning (Adrenaline + CSTs) (n = 5 in each group). Statistical significance of the differences from basal values before adrenaline administration were determined by ANOVA followed by a post hoc test (Fisher’s PLSD). *P < 0.05 vs. basal value. Significant differences between data sets (P < 0.05, P < 0.01) are indicated above the appropriate square bracket (ANOVA followed by a contrast test)
Effects of activation of α-adrenoceptors on hemodynamics in the masseter muscle evoked by AN stimulation and SABP after CST sectioning during high spontaneous activity in the CST
Figure 5 shows the effects of the intravenous administration of clonidine alone and in combination with yohimbine or propranolol and phenylephrine on the changes in MBF and VC in the left masseter muscle evoked by stimulation of the left AN, as well as changes in the SABP after left CST sectioning. The basal level of the MBF after administration of either clonidine (P < 0.01) or phenylephrine (P < 0.05) at 10 μg/ml, but not 2 μg/ml, was significantly smaller than that before their administration. The administration of clonidine negated the inhibitory effects of CST sectioning on MBF increases evoked by AN stimulation at 10 min after clonidine injection in a dose-dependent manner (2–10 μg/ml), whereas the administration of phenylephrine did not influence the inhibition (Fig. 5a, b). Increases in MBF evoked by AN stimulation in combination with clonidine (10 μg/ml) after CST sectioning were not observed at 10 min after pretreatment with yohimbine or propranolol, and the response in the MBF returned to near the initial value at 30 min after their administration (Fig. 5a). There was a significant difference in the increases in the masseter muscle VC evoked by AN stimulation before and after 10 μg/ml of clonidine administration (P < 0.001) (Fig. 5c). Yohimbine or propranolol pretreatment significantly reduced the increase in the masseter muscle VC (P < 0.001) (Fig. 5c). The HR at 10 min after administration of 2 and 10 μg/ml clonidine was 424 ± 21 and 343 ± 5 beats/min, respectively, while that after administration of 2 and 10 μg/ml phenylephrine was 407 ± 7 and 407 ± 8 beats/min, respectively. The mean SABP after administration of 2 and 10 μg/ml clonidine was 88.7 ± 2.5 and 74.6 ± 3.9 mmHg, respectively, while that after the administration of 2 and 10 μg/ml phenylephrine was 127.7 ± 10.9 and 123.5 ± 4.9 mmHg, respectively. There were statistically significant differences in both the HR (P < 0.01) and mean SABP (P < 0.05) before and after the administration of clonidine at 10 μg/ml.
Effects of activation of α-adrenoceptors on changes in the hemodynamics of the masseter muscle and on SABP evoked by AN stimulation after CST sectioning during high spontaneous activity in the CST. a, b Typical examples of changes in the MBF and VC in the left masseter muscle and SABP evoked by left AN stimulation (AN stim.; 20 s, 10 V, 20 Hz, 2-ms) (at black horizontal bars) at 10 min after left CST sectioning (Control CSTs), in combination with intravenous administration for 10 min (0.1 ml/min) of α2-adrenoceptor agonist clonidine (2–10 μg/ml), clonidine (10 μg/ml) and yohimbine (0.5 mg/ml) or propranolol (1 mg/ml) applied together, and 30 min after the injection (a), and in combination with administration of α1-adrenoceptor agonist phenylephrine (2–10 μg/ml) (b). The white trace shows the mean VC for the various data. c Mean data ± SEM of the changes (black bars) in the left MBF (top) and masseter muscle VC (bottom) evoked by AN stimulation at 10 min after CST sectioning for the various treatments (n = 6 in each group). Presence (+) or absence (−) of treatment is indicated under the bars. Statistical significance of the differences from the control before the drug injections determined by ANOVA, followed by a post hoc test (Fisher’s PLSD). *P < 0.001 vs. control. Significant differences between sets of data (P < 0.05, P < 0.001) are indicated above the appropriate square bracket (ANOVA followed by a contrast test)
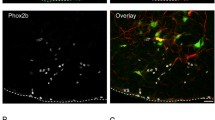
Expression of α-adrenoceptor isoforms in the masseter muscle
An RT-PCR was performed to determine which α-adrenoceptor isoforms were expressed in the masseter muscle and lower lip. As shown in Fig. 6, the four isoforms (α1A, α2A, α2B, and α2C) were observed at 479, 265, 396, and 567 bp, respectively, as expected (Fig. 6a). The cDNA products of the housekeeping gene GAPDH (452 bp) were expressed in all of the tissue samples. The sequence analyses of these PCR products verified the identity of the various isoforms (data not shown). The relative volumes of their isoforms were significantly higher in the masseter muscle than in lower lip (P < 0.05), with the exception of the α2B isoform (Fig. 6b).
Identification of mRNA expression of α-adrenoceptor isoforms α1A, α2A, α2B, and α2C in the masseter muscle and lower lip using reverse transcription-PCR. a Typical examples of the amplified PCR fragments were consistent with the length predicted by the subunit primers. All PCR products were compared with a 100-base DNA ladder (Φ). G Glyceraldehyde-3-phosphate dehydrogenase (GAPDH). b Gene expression of the α-adrenoceptor isoforms in the masseter muscle (black bars) and lower lip (white bars) normalized with GAPDH from the same template and shown as a ratio (mean ± SEM). Statistical significance of the differences between the masseter muscle and lower lip was determined by ANOVA, followed by a post hoc test (Fisher’s PLSD). *P < 0.05, **P < 0.01 vs. masseter muscle
Discussion
Our results show that electrical stimulation of the peripheral cut end of the AN, which induces activation of the sympathoadrenal system, significantly increased the MBF bilaterally in cervically vagotomized rats, while there were no significant increases induced by AN stimulation in the LBF (Figs. 2, 3). The increases in the MBF evoked by AN stimulation were almost completely reversed by the intravenous administration of propranolol (Fig. 3) and not dependent on changes in SABP (Fig. 2). Further, there were no significant differences in the HR before and after AN stimulation (Table 2). These results suggest that the MBF increase elicited by the AN stimulation is not a passive result of any evoked SABP or HR changes and that this increase should be considered to be ‘β-adrenergic vasodilation’. These findings are consistent with the observation that the AN stimulation-induced MBF increase in rats is mediated entirely through the β2-adrenoceptors in the masseter muscle [7].
Sectioning of the CST ipsilaterally increased the basal level of MBF, and it significantly inhibited MBF increases induced by AN stimulation during high spontaneous activity in the CST, but not during low activity (Figs. 2, 3). The changes in the MBF evoked by AN stimulation after CST sectioning were similar to those evoked by the intravenous administration of adrenaline (Fig. 4). These results indicate that interactions between the β-adrenergic vasodilation and cervical sympathetic nerves are involved in the maintenance of MBF during high spontaneous activity in the CST. The results of our previous study indicate that AN stimulation elicits MBF increases in cervically sympathectomized rats [7]. The precise reasons for differences in MBF responses are not clear, but anesthesia does influence the mean resting levels of the sympathetic outflow, and differences in MBF responses may be due to differences in the activity of cervical sympathetic nerves depending on the level of anesthesia [23, 24]. Other conditions in our study, such as dose of anesthesia, respiration rate, and SABP levels, are unlikely to account for the discrepancy of MBF response evoked by AN stimulation between our present and previous study [7] because the experimental conditions in both studies are similar.
During high spontaneous activity in the CST, AN stimulation after CST sectioning in combination with the intravenous administration of the α2-adrenoceptor agonist clonidine induced a significant increase in the MBF, which was largely suppressed by pretreatment with yohimbine or propranolol (Fig. 5a, c). The administration of the α1-adrenoceptor agonist phenylephrine had no effect on the AN stimulation-induced MBF responses after the CST sectioning, while it restored the basal level of the MBF to the pre-sectioned values (Fig. 5b, c). These results suggest that the interaction between the cervical sympathetic nerves (neural) and the sympathoadrenal system (humoral) in the regulation of MBF during high spontaneous activity in the CST is closely related to the α2- rather than the α1-adrenoceptors via the cervical sympathetic nerves. The α2-adrenoceptors are located on sympathetic nerve terminals innervating vascular smooth muscle cells, and they mediate a negative modulation of release of noradrenaline [25, 26]. However, in several blood vessels, post-junctional α2-adrenoceptors contribute to the vasoconstriction caused by noradrenaline [25, 27]. The identity of the α2-adrenoceptors involved in β-adrenergic vasodilation in the masseter muscle has not been established conclusively; however, the post-junctional α2-adrenoceptor must be involved in the response because clonidine administration decreased the MBF consistently in the present study (Fig. 5a). This conclusion is supported by the findings that the three major α2-adrenoceptor isoforms (α2A, α2B, and α2C) were expressed in the masseter muscle (Fig. 6). The α2-adrenoceptors are coupled predominantly to the inhibitory GTP-binding protein (Gi) which inhibits the activity of adenylyl cyclase [25, 28], while β2-adrenoceptors lead to activation of adenylyl cyclase via the stimulatory GTP-binding protein (Gs) [25, 29]. Activation of the β2-adrenoceptor has been reported to depend on the basal adenylyl cyclase activity [29, 30], suggesting that adenylyl cyclase-based cross-talk between these receptors may be related to the modulation of β-adrenergic vasodilation in the masseter muscle (Fig. 7).
Proposed schema for modulating effects of sympathetic systems in the blood flow in rat masseter muscle. Noradrenaline (NA) released by cervical sympathetic nerve (cSN) may induce modulation of β-adrenergic vasodilation mediated by circulating adrenaline (AD) through the post-junctional α2-adrenoceptor (α2AR) in the blood vessels in the masseter muscle. α1AR α1-Adrenoceptor, βAR β-adrenoceptor
The β-adrenergic vasodilation is generally accepted to be involved in the modulation of hemodynamics in skeletal muscles during sympathoexcitation [31–34], suggesting an important role in the maintenance of the blood flow and activity of muscles. In the masseter muscle, sympathoexcitation with cold-pressor stimulation induces an increase in intramuscular blood volume in the human masseter muscle, and this increase is reduced significantly by propranolol treatment [11, 35]. These observations suggest that β-adrenergic vasodilation is involved in MBF increases during sympathoexcitation. The functional implications of α2-adrenoceptors in the masseter muscle are unclear. However, α2-adrenoceptors have been shown to be relatively more prevalent on distal terminal arterioles and affected by local metabolic influences, while larger arteriole constriction has been found to be mediated predominantly by α1-adrenoceptors and to be less affected by local tissue factors [36–38]. These observations suggest that an interaction between β-adrenergic vasodilation evoked by circulating adrenaline and cervical sympathetic nerves mediated by α2-adrenoceptors would be important for facilitating blood flow and oxygen delivery in the masseter muscle during its exercise.
In summary, our results indicate that cervical sympathetic nerves are involved in β-adrenergic vasodilation in the masseter muscle evoked by circulating adrenaline released from the adrenal medulla during high spontaneous activity in the CST. They thereby suggest that the activation of α2- rather than α1-adrenoceptors via cervical sympathetic nerves contributes to the observed vasodilation in the masseter muscle. Further studies of the precise mechanisms for the interaction between α- and β-adrenoceptors and their molecular properties involved in the hemodynamics of the jaw muscles should provide a better understanding of the physiological role of neural and humoral regulations of the blood flow in the orofacial area.
Change history
20 April 2018
The article Interactions between β-adrenergic vasodilation and cervical sympathetic nerves are mediated by α2-adrenoceptors in the rat masseter muscle, written by Hisayoshi Ishii and Toshiya Sato, was originally published Online First without open access.
References
Ishii H, Niioka T, Izumi H (2007) Parasympathetic vasodilator fibers in masseter muscle. J Oral Biosci 49:163–172
Ishii H, Niioka T, Sudo E, Izumi H (2005) Evidence for parasympathetic vasodilator fibres in the rat masseter muscle. J Physiol 569:617–629
Sudo E, Ishii H, Niioka T, Hirai T, Izumi H (2009) Parasympathetic vasodilator fibers in rat digastric muscle. Brain Res 1302:125–131
Ishii H, Niioka T, Izumi H (2011) Parasympathetic reflex vasodilatation in the masseter muscle compensates for carotid hypoperfusion during the vagus-mediated depressor response. Brain Res 1370:145–153
Ishii H, Niioka T, Izumi H (2010) Vagal visceral inputs to the nucleus of the solitary tract: involvement in a parasympathetic reflex vasodilator pathway in the rat masseter muscle. Brain Res 1312:41–53
Ishii H, Niioka T, Watanabe H, Izumi H (2007) Inhibitory effects of excess sympathetic activity on parasympathetic vasodilation in the rat masseter muscle. Am J Physiol Regul Integr Comp Physiol 293:R729–R736
Ishii H, Niioka T, Izumi H (2009) Circulating adrenaline released by sympathoadrenal activation elicits acute vasodilatation in the rat masseter muscle. Arch Oral Biol 54:486–494
Delcanho RE, Kim YJ, Clark GT (1996) Haemodynamic changes induced by submaximal isometric contraction in painful and non-painful human masseter using near-infra-red spectroscopy. Arch Oral Biol 41:585–596
Kulshreshtha P, Deepak KK (2013) Autonomic nervous system profile in fibromyalgia patients and its modulation by exercise: a mini review. Clin Physiol Funct Imaging 33:83–91
Maekawa K, Clark GT, Kuboki T (2002) Intramuscular hypoperfusion, adrenergic receptors, and chronic muscle pain. J Pain 3:251–260
Maekawa K, Kuboki T, Clark GT, Shinoda M, Yamashita A (1998) Cold pressor stimulus temperature and resting masseter muscle haemodynamics in normal humans. Arch Oral Biol 43:849–859
Roatta S, Mohammed M, Passatore M (2009) Acute stress reduces blood flow in the orofacial area, in conscious rabbits. Arch Oral Biol 54:380–388
Ishii H, Izumi H (2012) GABAB receptors in the NTS mediate the inhibitory effect of trigeminal nociceptive inputs on parasympathetic reflex vasodilation in the rat masseter muscle. Am J Physiol Regul Integr Comp Physiol 302:R776–R784
Ishii H, Niioka T, Izumi H (2009) Difference between male and female rats in cholinergic activity of parasympathetic vasodilatation in the masseter muscle. Arch Oral Biol 54:533–542
Ishii H, Sato T, Izumi H (2014) Parasympathetic reflex vasodilation in the cerebral hemodynamics of rats. J Comp Physiol B 184:385–399
Niioka T, Ishii H, Izumi H (2009) Regional differences in blood flow variation in rat masseter muscle. Arch Oral Biol 54:1022–1028
Stern MD, Lappe DL, Bowen PD, Chimosky JE, Holloway GA Jr, Keiser HR, Bowman RL (1977) Continuous measurement of tissue blood flow by laser-Doppler spectroscopy. Am J Physiol 232:H441–H448
Kumakura K, Sato A, Suzuki H (1988) Direct recording of total catecholamine secretion from the adrenal gland in response to splanchnic nerve stimulation in rats. J Neurosci Methods 24:39–43
Okuma Y, Yokotani K, Osumi Y (1995) Centrally applied bombesin increases nerve activity of both sympathetic and adrenal branch of the splanchnic nerves. Jpn J Pharmacol 68:227–230
Vollmer RR, Balcita-Pedicino JJ, Debnam AJ, Edwards DJ (2000) Adrenal medullary catecholamine secretion patterns in rats evoked by reflex and direct neural stimulation. Clin Exp Hypertens 22:705–715
Wilborn TW, Sun D, Schafer JA (1998) Expression of multiple α-adrenoceptor isoforms in rat CCD. Am J Physiol 275:F111–F118
Ishii H, Oota I, Arakawa T, Takuma T (2002) Differential gene expression of vascular endothelial growth factor isoforms and their receptors in the development of the rat masseter muscle. Arch Oral Biol 47:505–510
Dorward PK, Riedel W, Burke SL, Gipps J, Korner PI (1985) The renal sympathetic baroreflex in the rabbit. Arterial and cardiac baroreceptor influences, resetting, and effect of anesthesia. Circ Res 57:618–633
Shimokawa A, Kunitake T, Takasaki M, Kannan H (1998) Differential effects of anesthetics on sympathetic nerve activity and arterial baroreceptor reflex in chronically instrumented rats. J Auton Nerv Syst 72:46–54
Guimaraes S, Moura D (2001) Vascular adrenoceptors: an update. Pharmacol Rev 53:319–356
Langer SZ (1997) 25 years since the discovery of presynaptic receptors: present knowledge and future perspectives. Trends Pharmacol Sci 18:95–99
Flavahan NA, Cooke JP, Shepherd JT, Vanhoutte PM (1987) Human postjunctional alpha-1 and alpha-2 adrenoceptors: differential distribution in arteries of the limbs. J Pharmacol Exp Ther 241:361–365
Ziolkowski N, Grover AK (2010) Functional linkage as a direction for studies in oxidative stress: α-adrenergic receptors. Can J Physiol Pharmacol 88:220–232
McGraw DW, Liggett SB (2005) Molecular mechanisms of β2-adrenergic receptor function and regulation. Proc Am Thorac Soc 2:292–296 (discussion 311–292)
Billington CK, Ojo OO, Penn RB, Ito S (2013) cAMP regulation of airway smooth muscle function. Pulm Pharmacol Ther 26:112–120
Berecek KH, Brody MJ (1982) Evidence for a neurotransmitter role for epinephrine derived from the adrenal medulla. Am J Physiol 242:H593–H601
Herd JA (1991) Cardiovascular response to stress. Physiol Rev 71:305–330
Yardley CP, Hilton SM (1987) Vasodilatation in hind-limb skeletal muscle evoked as part of the defence reaction in the rat. J Auton Nerv Syst 19:127–136
Vianna LC, Silva BM, Nobrega AC (2014) Sex differences in blood pressure responses to mental stress are abolished after a single bout of exercise: underlying hemodynamic mechanisms. J Physiol Sci 64:213–219
Maekawa K, Kuboki T, Miyawaki T, Shimada M, Yamashita A, Clark GT (1999) Effect of intravenous infusion of a β-adrenergic blocking agent on the haemodynamic changes in human masseter muscle induced by cold-pressor stimulation. Arch Oral Biol 44:475–483
McGillivray-Anderson KM, Faber JE (1990) Effects of acidosis on contraction of microvascular smooth muscle by α1- and α2-adrenoceptors: implications for neural and metabolic regulation. Circ Res 66:1643–1657
Ohyanagi M, Faber JE, Nishigaki K (1991) Differential activation of α1- and α2-adrenoceptors on microvascular smooth muscle during sympathetic nerve stimulation. Circ Res 68:232–244
Dinenno FA, Joyner MJ (2006) α-Adrenergic control of skeletal muscle circulation at rest and during exercise in aging humans. Microcirculation 13:329–341
Acknowledgements
This study was supported, in part, by MEXT KAKENHI (No. 25462896) to H. Ishii.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest, financial or otherwise, regarding this article.
Additional information
The original version of this article was revised due to a retrospective open access order.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Ishii, H., Sato, T. Interactions between β-adrenergic vasodilation and cervical sympathetic nerves are mediated by α2-adrenoceptors in the rat masseter muscle. J Physiol Sci 67, 699–709 (2017). https://doi.org/10.1007/s12576-016-0499-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12576-016-0499-3