Abstract
Background
Left ventricular non-compaction (LVNC) cardiomyopathy in adults has primarily been studied with a phenotypic expression of low ejection fraction (EF) and dilated cardiomyopathy; however, data on LVNC with preserved EF is scarce. The present study aimed to evaluate cardiac geometry and mechanics in LVNC patients with preserved EF.
Methods
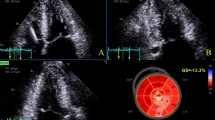
A retrospective cohort study of patients diagnosed with LVNC and a preserved EF between 2008 and 2019 was performed. LVNC was defined according to the presence of established transthoracic 2D echocardiographic (TTE) criteria as follows: (1) prominent LV trabeculations with deep recesses; (2) bi-layered myocardial appearance; and, (3) systolic non-compacted:compacted ratio≥ 2. Subjects were matched 1:1 to controls without LVNC referred for routine TTE. Geometric, functional and mechanics parameters were analyzed in the two cohorts using 2D and speckle-tracking TTE.
Results
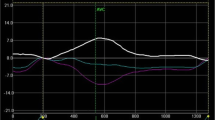
Seventeen patients with LVNC and preserved EF were identified. Compared with controls, patients with LVNC had similar LV systolic function and chamber dimensions, but a larger mass and relative wall thickness, and more abnormal LV geometry (76% vs. 18%, p = 0.002), LA remodeling, and pulmonary hypertension. Global longitudinal strain was significantly decreased (-15.4 ± 3.2 vs. -18.9 ± 2.8%, p = < 0.01) and the prevalence of rigid body rotation was significantly increased (57% vs. 14%, p = 0.05) in the LVNC population. The peak twist values were comparable in both cohorts.
Conclusions
Impaired LV geometry and longitudinal mechanics, as well as increased myocardial stiffness as expressed by rigid body rotation, characterize LVNC with preserved EF when compared with controls.

Similar content being viewed by others
References
Maron BJ, Towbin JA, Thiene G, et al. Contemporary definitions and classification of the cardiomyopathies. Circulation. 2006;113:1807–16.
Varnava AM. Isolated left ventricular non-compaction: A distinct cardiomyopathy? Heart. 2001;86:599–600.
Oechslin E, Jenni R. Left ventricular non-compaction revisited: A distinct phenotype with genetic heterogeneity? Eur Heart J. 2011;32:1446–56.
Wessels A, Sedmera D. Developmental anatomy of the heart: A tale of mice and man. Physiol Genom. 2004;15:165–76.
Towbin JA, Jefferies JL. Cardiomyopathies due to left ventricular noncompaction, mitochondrial and storage diseases, and inborn errors of metabolism. Circ Res. 2017;121:838–54.
Lofiego C, Biagini E, Pasquale F, et al. Wide spectrum of presentation and variable outcomes of isolated left ventricular non-compaction. Heart. 2007;93:65–71.
van Waning JI, Caliskan K, Hoedemaekers YM, et al. Genetics, clinical features, and long-term outcome of noncompaction cardiomyopathy. J Am Coll Cardiol. 2018;71:711–22.
Li S, Zhang C, Liu N, et al. Genotype-positive status is associated with poor prognoses in patients with left ventricular noncompaction cardiomyopathy. J Am Heart Assoc. 2018;7: e009910.
Gati S, Papadakis M, Papamichael ND, et al. Reversible de novo left ventricular trabeculations in pregnant women: Implications for the diagnosis of left ventricular noncompaction in low-risk populations. Circulation. 2014;130:475–83.
Arbustini E, Favalli V, Narula N, Serio A, Grasso M. Left ventricular noncompaction: a distinct genetic cardiomyopathy? J Am Coll Cardiol. 2016;68:949–66.
Anderson RH, Jensen B, Mohun TJ, et al. Key questions relating to left ventricular noncompaction cardiomyopathy: is the emperor still wearing any clothes? Can J Cardiol. 2017;33:747–57.
Gati S, Chandra N, Bennett RL, et al. Increased left ventricular trabeculation in highly trained athletes: Do we need more stringent criteria for the diagnosis of left ventricular non-compaction in athletes? Heart. 2013;99:401–8.
Elliott P, Andersson B, Arbustini E, et al. Classification of the cardiomyopathies: A position statement from the european society of cardiology working group on myocardial and pericardial diseases. Eur Heart J. 2008;29:270–6.
Biering-Sørensen T, Biering-Sørensen SR, Olsen FJ, et al. Global longitudinal strain by echocardiography predicts long-term risk of cardiovascular morbidity and mortality in a low-risk general population: The Copenhagen City Heart Study. Circ Cardiovasc Imag. 2017;10:1–11.
Opdahl A, Helle-Valle T, Skulstad H, Smiseth OA. Strain, strain rate, torsion, and twist: echocardiographic evaluation. Curr Cardiol Rep. 2015;17:1–14.
Stokke TM, Hasselberg NE, Smedsrud MK, et al. Geometry as a confounder when assessing ventricular systolic function: comparison between ejection fraction and strain. J Am Coll Cardiol. 2017;70:942–54.
Bellavia D, Michelena HI, Martinez M, et al. Speckle myocardial imaging modalities for early detection of myocardial impairment in isolated left ventricular non-compaction. Heart. 2010;96:440–7.
Arenas IA, Mihos CG, DeFaria YD, Yucel E, Elmahdy HM, Santana O. Echocardiographic and clinical markers of left ventricular ejection fraction and moderate or greater systolic dysfunction in left ventricular noncompaction cardiomyopathy. Echocardiography. 2018;35:941–8.
van Dalen BM, Caliskan K, Soliman OII, et al. Left ventricular solid body rotation in non-compaction cardiomyopathy: A potential new objective and quantitative functional diagnostic criterion? Eur J Heart Fail. 2008;10:1088–93.
Peters F, Khandheria BK, Libhaber E, et al. Left ventricular twist in left ventricular noncompaction. Eur Heart J Cardiovasc Imag. 2014;15:48–55.
Jenni R. Echocardiographic and pathoanatomical characteristics of isolated left ventricular non-compaction: a step towards classification as a distinct cardiomyopathy. Heart. 2001;86:666–71.
Lang RM, Badano LP, Victor MA, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: An update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015;28:1–39.
Steckelberg RC, Tseng AS, Nishimura R, Ommen S, Sorajja P. Derivation of mean pulmonary artery pressure from noninvasive parameters. J Am Soc Echocardiogr. 2013;26:464–8.
Simonneau G, Montani D, Celermajer DS, et al. Haemodynamic definitions and updated clinical classification of pulmonary hypertension. Eur Respir J. 2019;53:1801913.
Arunamata A, Stringer J, Balasubramanian S, et al. Cardiac segmental strain analysis in pediatric left ventricular noncompaction cardiomyopathy. J Am Soc Echocardiogr. 2019;32:763–73.
Badano LP, Muraru D. Twist mechanics of the left ventricle. Circ Cardiovasc Imag. 2019;12: e009085.
Omar AMS, Vallabhajosyula S, Sengupta PP. Left ventricular twist and torsion. Circ Cardiovasc Imag 2015;8:1–10.
van Dalen BM, Caliskan K, Soliman OI, et al. Diagnostic value of rigid body rotation in noncompaction cardiomyopathy. J Am Soc Echocardiogr. 2011;24:548–55.
Drazner MH, Dries DL, Peshock RM, et al. Left ventricular hypertrophy is more prevalent in blacks than whites in the general population: The Dallas heart study. Hypertension. 2005;46:124–9.
Nawaytou HM, Montero AE, Yubbu P, et al. A preliminary study of left ventricular rotational mechanics in children with noncompaction cardiomyopathy: do they influence ventricular function? J Am Soc Echocardiogr. 2018;31:951–61.
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Guigui, S.A., Horvath, S.A., Arenas, I.A. et al. Cardiac geometry, function and mechanics in left ventricular non-compaction cardiomyopathy with preserved ejection fraction. J Echocardiogr 20, 144–150 (2022). https://doi.org/10.1007/s12574-021-00560-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12574-021-00560-7