Abstract
Purpose
In the present short report, we encompass the radiobiological and dosimetric advantages of particle beam radiotherapy and we illustrate the oncological pathway for patients eligible for hadrontherapy being used at the National Center for Oncological Hadrontherapy (CNAO).
Methods
With a narrative approach, we examined the clinical and practical aspects of hadrontherapy compared to traditional photon beam radiotherapy. We described the need to select patients considering the intrinsic characteristics both of the tumour and the patient. Moreover, we described the decisional oncological tree and the patient pathway by our facility.
Results
Considering the dosimetric and radiobiological characteristics of particle beam radiotherapy, the selection of patients can not be done regardless of the intrinsic tumour and patient hallmarks. In particular, the tumour radioresistance, the patient radiosensitivity and the need to avoid post-actinic toxicities in long-term survivors should guide the clinical indication. The finite range of particles should be considered to avoid treatment uncertainties. Multidisciplinary national and international collaboration is crucial to better manage patients to treat with hadrontherapy and to create robust clinical evidence.
Conclusion
Hadrontherapy, with its distinctive physical and biological advantages, heralds a promising era in the field of precision radiotherapy. Patients’ radiosensitivity, tumour radioresistance, and treatment uncertainties should be considered to enhance the efficacy and to ameliorate the selection of patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Over the past decades, several significant improvements have been made in the radiotherapy (RT) field enhancing precision, effectiveness, and quality of life of cancer patients. The advantages in terms of toxicity reduction of intensity-modulated radiation therapy (IMRT) are now well known [1, 2] However, despite the high conformality of this technique, the organs at risk (OARs) still receive low to moderate radiation doses that may lead to the development of radiation-induced side effects. The introduction of hypofractionation and stereotactic ablative radiotherapy has further brought the clinical community closer to the goal of precisely targeting the tumour with an excellent safety profile, but unfortunately, despite the proven benefits especially in the oligometastatic setting [3,4,5,6], further research is mandatory for the definition of optimal selection criteria, dose-fractionation schedules, and predictive factors. Considering that over 50% of oncological patients need RT during their oncological road and, in light of the improvement of survival thanks to the therapeutic progress, all efforts should be made to increase the quality of life also by reducing the toxicity. In this scenario, the growing interest in the application of new RT technology, such as particle beam RT (also known as hadrontherapy), appears justified by the ballistic and radiobiological proprieties of particles. Indeed, on one hand, the dose distribution of the particles allows maximal dose release at the tumour depth, followed by sharp distal dose fall-off which is responsible for a more effective OAR avoidance. On the other, protons and carbon ions exhibit a distinctive energy deposition curve compared to X-rays, characterized by the Bragg peak at the termination of their path within tissues [7]. In addition, the heightened relative biological effectiveness (RBE) of carbon ions, coupled with their ability to induce clustered DNA damages, provides a distinct biological and immunological advantage [8], increasing the therapeutic window between tumour control probability (TCP) and normal tissue complication probability (NTCP) [9]. These benefits are particularly prominent in the case of radioresistant tumours, radio-induced malignancies, challenging anatomical regions, and recurrent settings. In this scenario, hadrontherapy represents a valuable biology-based strategy potentially leading an optimization of tumour control, while reducing normal tissue injury from radiation damage even modulating the immune system. This approach is fully integrated into the frame of tailored RT and oncological treatments.
To provide a holistic snapshot of the clinical implications of hadrontherapy, herein we will encompass briefly the radiobiological and dosimetric advantages of particle beam RT over photon beam RT (X-RT) and we will design a possible oncological pathway for patients eligible for hadrontherapy based on the clinical practice used in our particle beam institution.
2 Tumour and patient’s hallmarks: a guide for the selection criteria and the clinical indications for particle beam RT
To better select patients eligible for particle beam RT, the multidisciplinary oncological team should take into account the intrinsic tumour and the patient’s specific characteristics.
From the tumour perspective, hadrontherapy (and, among particles, mainly carbon ions) is suitable for overcoming tumour radioresistance [8]. Radioresitant tumours have a low α/β ratio, with a consequent slow proliferation, a large hypoxic fraction [10] and a high amount of cancer stem cells [11, 12]. Taken together, all these hallmarks seem to be insurmountable by conventional RT.
Indeed, hypoxia leads to epithelial-mesenchymal transition inducing circulating tumour cell (CTC) formation, migration and invasiveness and significantly increasing the angiogenesis-related gene expression, facilitating CTC entry into the blood flow [13]. Moreover, hypoxia activates several hypoxia-inducible factors (HIFs) implicated in metabolic, angiogenetic, cell growth and differentiation, survival, and apoptosis pathways [14]. However, it has been proved that, over X-RT and proton beam RT (PBT), carbon ion radiotherapy (CIRT) significantly reduces the ability of tumour cells to invade and migrate [15,16,17], decreases the HIF expression and delays tumour growth [18,19,20]. For these reasons, when the radiation oncologists have to decide the type of radiation to use, they should take into account the oxygen enhancement ratio (OER), that is the ratio of dosages in oxic and hypoxic tissues that can reach up to 3. OER is strongly dependent on the partial pressure of oxygen and on the linear energy transfer (LET), but is barely influenced by the dose [21, 22]. Nakano et al [23] clinically demonstrated that CIRT can overcome hypoxia-induced radioresistance in bulky cervical uterine carcinomas. To the best of our knowledge, this trial is the only clinical experience based on real-world data about the effectiveness of high LET with low OER in hypoxic tumours. Nevertheless, the remarkable clinical outcomes, recently summarized by Pompos et colleagues [24], for CIRT in patients with well-known hypoxic diseases (i.e. pancreatic cancers, sacral chordoma, osteosarcomas, mucosal melanomas, soft tissue sarcomas, liver and prostate malignancies), point to the importance of a lower OER to reduce the impact of intrinsic radioresistance by high LET. However, OER has been proven to be higher in vitro than in vivo [25,26,27], suggesting that hypoxia is not the only factor to be considered in these challenging cases.
In recent years a growing interest in the impact of CIRT on the tumor microenvironment and immune response has emerged. Experiments on human tongue squamous carcinoma (Tca8113 and Cal27) and the glioma cell lines (Ln229 and Ln18) showed the ability of CIRT to upregulate the calreticulin and the programmed cell death ligand 1 (PD-L1) in normoxic conditions as compared to X-RT and PBT [28]. PD-L1 expression increased after CIRT also in cervical adenocarcinoma (HeLa) and human osteosarcoma (U2OS) cell lines [29, 30] and the data was confirmed clinically on specimens obtained by patients treated with CIRT for cervical adenocarcinomas [29]. These pieces of evidence suggested that CIRT mediated the oncological immunogenic cell death. The induction of an abscopal effect after CIRT both in preclinical [31, 32] and also in sporadic clinical experiences supported the hypothesis that CIRT works through the immune system more than X-RT [33, 34]. To create evidence, several trials are now exploring this thesis in large bulky tumours treated partially (PArtial Tumor irradiation targeting HYpoxic segment -PATHY-) [35] or in metastatic radioresistant settings in combination with immunotherapy [36]. Notably, the physics of particles justifies their immunogenic effects. Indeed, a significantly high amount of naïve T-lymphocytes and memory T-cells, which are necessary to initiate and maintain a tumour-specific immune response, are spared by the lowered integral dose of CIRT compared to XRT or PBT [33]. Among hadrons, protons have a similar biological effectiveness of X-RT except for a little area closest to the edge of their range, where there is an increased LET that causes an increase of RBE [37], supporting the need to prefer CIRT for the tumours that exhibit radioresistant hallmarks.
Beyond the immunological advantages, its characteristic dose deposition makes CIRT suitable for tumours located in challenging anatomical localization and close to high radiosensitive normal tissues. This is true also for PBT where the maximum deposition of the energy is at the end of the particle range, within Bragg’s peak. Hence, both PBT and CIRT offer unparalleled target conformality with a significantly reduced integral dose to normal tissues compared to the most modern X-RT with a consequent lower risk of post-actinc adverse events. This is particularly worthwhile in all those scenarios where the tumours are unresectable and/or recurrent but the radiation oncologists must respect strict anatomical constraints, such as in malignancies located in the skull base [38, 39] or near the spinal cord [40] as well as recurrent in the head-and-neck region [41,42,43] or in the pelvic area [44,45,46,47].
Shifting to a “patient-tailored” perspective, the age, the comorbidities, the previous treatment (including RT but also chemotherapy regimens) as well as the genetic background are crucial aspects to consider in the decision-making flowchart.
Data from the most updated survey on the current practice among European PBT centres showed how adult patients are submitted to protons if the main objective is toxicity risk decrease or, more rarely, dose escalation. In addition, both younger and geriatric patients can benefit from PBT, the former due to longer life expectancy, and the latter due to increased vulnerability [48]. In children and really young populations, all efforts should be made to reduce the risk of the more dramatic adverse event: the radio-induction of secondary malignancies. Literature data demonstrated that PBT is associated with a significantly lower risk of second cancer compared to X-RT, a result that cannot be ignored in long-surviving cancer patients [49,50,51]. Furthermore, we should remember that the most frequent cause of death in long-term survivors from a mediastinal X-RT for Hodgkin lymphoma is the cardiovascular disease provoked by the combination of cardiotoxic chemotherapies and unnecessary doses to the heart and its substructures, highlighting the need to better select patients to enrol for PBT [52]. No less important, in a tailored strategy that considers the patient’s quality of life, we should consider the possibility of hadrontherapy to preserve fertility in children and young patients [53, 54].
Unforeseen toxicities might occur in patients with individual radiation sensitivity (iRS) based on their genetic background. NTCP models and a variety of tests to enhance toxicity prediction, such as iRS tests, might be useful in selecting high-risk patients to be treated with hadrontherapy, considering the potential advantages of particles in reducing unexpected toxicities also in this challenging group [55].
Figure. 1 Synthesized the hadrontherapy’s indications in relation to tumour and patient characteristics.
3 Managing the particle range uncertainties in challenging anatomical situations
The dosimetric advantage of hadrontherapy is due to its finite range. However, this edge might be potentially penalizing and related to a high risk of uncertainties due to dose computation, delivery, patient positioning, simulation imaging (i.e. uncertainty in the Hounsfield Unit to water equivalent path length calibration curve), intra- and interfraction anatomy variations (i.e.: breathing pattern, organ motion and filling status) as well as possible density variations found by the particles during their path to the target [56]. To overcome these limits several techniques were implemented.
Concerning organ motion management, different strategies are currently carried out in hadrontherapy facilities [57, 58]. Unfortunately, the adaptive RT with carbon ions is still unrealistic worldwide because of the current quality of in-room imaging, the long time necessary for plan optimization, and the unavailability of an online dose evaluation/replanning on intra-treatment cone-beam computed tomography (CBCT). At CNAO, the approach consists of a robust optimization on four-dimensional imaging simulation, an off-line adaptive approach along with a gated-dose delivery, rescanning and compression of the abdomen [59,60,61,62,63].
Moreover, the presence of high Z materials (such as metal prostheses and devices) creates additional uncertainties due to the significant perturbation effect on simulation imaging and distortion of dose distribution, leading to a compromised tumour coverage and a suboptimal OAR sparing. If a metallic device can not be avoided, a multidisciplinary discussion with the surgeons is mandatory to choose the correct metal type to use [64]. In addition, considering the substantial impact of organ filling status along with the variation of the anatomical interface, in a safe hadrontherapy dose distribution, a possible solution is to create space between challenging OARs, such as the intestinal tract, and the target. In this context, silicon [65], omentum [66], Gore-Tex [67, 68], hydrogel [69] as well as polyglycolic acid [70] were tested and proved to be safe and technically feasible. In addition, our group described a clinical-oriented approach able to translate the currently available radiobiological model in order to reduce the dissimilarity of CIRT plans [71].
4 Following the hadrontherapy clinical patient’s pathway
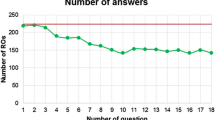
A hadrontherapy center can be incorporated within an oncological center or operate as an independent outpatient facility, with or without the availability of X-ray accelerators. The indications for hadrontherapy can widely vary from one country to another, according to national policies. In the same way, the methods by which patients are referred from oncological centers to hadrontherapy hubs differ worldwide, according also to the established and recognized networks at the regional or national level. Patients often live far from the particle beam center and, for this reason, we must provide them at least logistical support. Figure 2 explains the decisional tree used at our Institution to evaluate any potential indications for hadrontherapy. It should be noted that, in most cases, patients are referred to CNAO by a multidisciplinary team (located mainly in tertiary centres followed by the oncological unit of academic hubs or general hospitals). The multidisciplinary discussions of the cases, also through a virtual national tumour board, are of crucial importance in the correct selection of patients and in the management of rare tumours, that are commonly centralised at our Institution [72]. In our experience, another channel to evaluate patients is a direct contact between the specialists of the referring centre and CNAO, while barely a “self-patient referral”. Each case is evaluated considering both the national indications and the possibility of being included in ongoing and recruiting trials [73].
In particular, currently, for the following 10 indications, the Italian National Health System reimburses PBT and CIRT equally, without distinguishing between the two modalities:
-
1.
chordomas and chondrosarcomas (of the skull base and the spine);
-
2.
meningiomas in challenging intracranial sites;
-
3.
brain stem and spinal cord tumours;
-
4.
adenoid cystic carcinomas of the salivary glands;
-
5.
orbit tumours, including eye melanoma;
-
6.
extremity radioresistant sarcomas;
-
7.
soft tissue and bone sarcomas (head and neck, paraspinal, pelvic, retroperitoneal);
-
8.
recurrent tumours (re-irradiation);
-
9.
patients with genetic or immunological disorders related to higher radiosensitivity;
-
10.
paediatric solid tumours.
Moreover, we activated prospective trials to evaluate possible new indications for particles (i.e. gynaecological tumors, head and neck malignancies) [72]. In this scenario, considering the preclinical pieces of evidence about the immunogenic effect of hadrontherapy, especially when associated with immune-checkpoint inhibitors, we are exploring the feasibility and clinical activity of combining CIRT and immunotherapy in clinical settings [36].
When a patient is considered potentially eligible for hadrontherapy, we offer assistance for logistic issues and we collaborate with spoke hospitals for supportive care and/or , when indicated, for the administration of systemic therapies ( Fig. 3).
5 Conclusions
Hadrontherapy, with its distinctive physical and biological advantages, heralds a promising era in the field of precision RT. To enhance the efficacy and ameliorate the selection of patients, deeper reflections on patients’ radiosensitivity and tumour radioresistance, as well as treatment uncertainties, should be considered. A strong, creative, collaborative national and international networking between experts in hadrontherapy and rare tumours might lead to creating solid data, clinical evidence, consensus and desirably guidelines.
Data availability
No new data are included in the present paper.
References
Nutting CM, Morden JP, Harrington KJ, Urbano TG, Bhide SA, Clark C, et al. Parotid-sparing intensity modulated versus conventional radiotherapy in head and neck cancer (PARSPORT): a phase 3 multicentre randomised controlled trial. Lancet Oncol. 2011;12:127–36. https://doi.org/10.1016/S1470-2045(10)70290-4.
Peng G, Wang T, Yang K-Y, Zhang S, Zhang T, Li Q, et al. A prospective, randomized study comparing outcomes and toxicities of intensity-modulated radiotherapy vs. conventional two-dimensional radiotherapy for the treatment of nasopharyngeal carcinoma. Radiother Oncol J Eur Soc Ther Radiol Oncol. 2012;104:286–93. https://doi.org/10.1016/j.radonc.2012.08.013.
Gomez DR, Tang C, Zhang J, Blumenschein GRJ, Hernandez M, Lee JJ, et al. Local consolidative therapy Vs. maintenance Therapy or Observation for patients with Oligometastatic Non-small-cell Lung Cancer: long-term results of a multi-institutional, phase II, Randomized Study. J Clin Oncol off J Am Soc Clin Oncol. 2019;37:1558–65. https://doi.org/10.1200/JCO.19.00201.
Palma DA, Olson R, Harrow S, Gaede S, Louie AV, Haasbeek C, et al. Stereotactic ablative radiotherapy for the Comprehensive Treatment of Oligometastatic Cancers: long-term results of the SABR-COMET phase II randomized trial. J Clin Oncol off J Am Soc Clin Oncol. 2020;38:2830–8. https://doi.org/10.1200/JCO.20.00818.
Macchia G, Lazzari R, Colombo N, Laliscia C, Capelli G, D’Agostino GR, et al. A large, Multicenter, Retrospective Study on Efficacy and Safety of Stereotactic Body Radiotherapy (SBRT) in Oligometastatic Ovarian Cancer (MITO RT1 Study): a collaboration of MITO, AIRO GYN, and MaNGO groups. Oncologist. 2020;25:e311–20. https://doi.org/10.1634/theoncologist.2019-0309.
Macchia G, Pezzulla D, Campitelli M, Laliscia C, Fodor A, Bonome P, et al. Efficacy and safety of stereotactic body Radiation Therapy in Oligometastatic Uterine Cancer (MITO-RT2/RAD): a large, real-world study in Collaboration with Italian Association of Radiation Oncology, Multicenter Italian trials in Ovarian Cancer, and Mari. Int J Radiat Oncol Biol Phys. 2023;117:321–32. https://doi.org/10.1016/j.ijrobp.2023.04.025.
Beddok A, Vela A, Calugaru V, Tessonnier T, Kubes J, Dutheil P, et al. Proton therapy for head and neck squamous cell carcinomas: a review of the physical and clinical challenges. Radiother Oncol J Eur Soc Ther Radiol Oncol. 2020;147:30–9. https://doi.org/10.1016/j.radonc.2020.03.006.
Tinganelli W, Durante M. Carbon Ion Radiobiology. Cancers (Basel). 2020;12. https://doi.org/10.3390/cancers12103022.
Lin SH, Willers H, Krishnan S, Sarkaria JN, Baumann M, Lawrence TS. Moving beyond the Standard of Care: accelerate testing of Radiation-Drug combinations. Int J Radiat Oncol Biol Phys. 2021;111:1131–9. https://doi.org/10.1016/j.ijrobp.2021.08.018.
Sokol O, Durante M. Carbon ions for hypoxic tumors: are we making the most of them? Cancers (Basel). 2023;15. https://doi.org/10.3390/cancers15184494.
Galeaz C, Totis C, Bisio A, Radiation Resistance. A matter of transcription factors. Front Oncol. 2021;11:662840. https://doi.org/10.3389/fonc.2021.662840.
Olivares-Urbano MA, Griñán-Lisón C, Marchal JA, Núñez MI. CSC Radioresistance: a therapeutic challenge to improve Radiotherapy Effectiveness in Cancer. Cells 2020;9. https://doi.org/10.3390/cells9071651.
Tinganelli W, Durante M. Tumor Hypoxia and circulating Tumor cells. Int J Mol Sci. 2020;21. https://doi.org/10.3390/ijms21249592.
Choudhry H, Harris AL. Advances in Hypoxia-Inducible factor Biology. Cell Metab. 2018;27:281–98. https://doi.org/10.1016/j.cmet.2017.10.005.
Charalampopoulou A, Barcellini A, Frittitta GE, Fulgini G, Ivaldi GB, Magro G et al. In Vitro effects of Photon Beam and Carbon Ion Radiotherapy on the Perineural Invasion of Two Cell Lines of Neurotropic Tumours. Life 2023;13. https://doi.org/10.3390/life13030794.
Facoetti A, Di Gioia C, Pasi F, Di Liberto R, Corbella F, Nano R, et al. Morphological analysis of amoeboid-mesenchymal transition plasticity after low and high LET Radiation on migrating and invading pancreatic Cancer cells. Anticancer Res. 2018;38:4585–91. https://doi.org/10.21873/anticanres.12763.
Charalampopoulou A, Barcellini A, Ciocca M, Di Liberto R, Pasi F, Pullia MG, et al. Factors released by low and high-LET irradiated fibroblasts modulate migration and invasiveness of pancreatic cancer cells. Front Oncol. 2022;12:1003494. https://doi.org/10.3389/fonc.2022.1003494.
Subtil FSB, Wilhelm J, Bill V, Westholt N, Rudolph S, Fischer J, et al. Carbon ion radiotherapy of human lung cancer attenuates HIF-1 signaling and acts with considerably enhanced therapeutic efficiency. FASEB J off Publ Fed Am Soc Exp Biol. 2014;28:1412–21. https://doi.org/10.1096/fj.13-242230.
Valable S, Gérault AN, Lambert G, Leblond MM, Anfray C, Toutain J, et al. Impact of Hypoxia on Carbon Ion Therapy in Glioblastoma cells: modulation by LET and Hypoxia-Dependent genes. Cancers (Basel). 2020;12. https://doi.org/10.3390/cancers12082019.
Wozny A-S, Lauret A, Battiston-Montagne P, Guy J-B, Beuve M, Cunha M, et al. Differential pattern of HIF-1α expression in HNSCC cancer stem cells after carbon ion or photon irradiation: one molecular explanation of the oxygen effect. Br J Cancer. 2017;116:1340–9. https://doi.org/10.1038/bjc.2017.100.
Furusawa Y, Fukutsu K, Aoki M, Itsukaichi H, Eguchi-Kasai K, Ohara H, et al. Inactivation of aerobic and hypoxic cells from three different cell lines by accelerated (3)He-, (12)C- and (20)Ne-ion beams. Radiat Res. 2000;154:485–96. https://doi.org/10.1667/0033-7587(2000)154[0485:ioaahc]2.0.co;2.
Wenzl T, Wilkens JJ. Theoretical analysis of the dose dependence of the oxygen enhancement ratio and its relevance for clinical applications. Radiat Oncol. 2011;6:171. https://doi.org/10.1186/1748-717X-6-171.
Nakano T, Suzuki Y, Ohno T, Kato S, Suzuki M, Morita S, et al. Carbon Beam therapy overcomes the radiation resistance of uterine cervical cancer originating from hypoxia. Clin Cancer Res off J Am Assoc Cancer Res. 2006;12:2185–90. https://doi.org/10.1158/1078-0432.CCR-05-1907.
Pompos A, Foote RL, Koong AC, Le QT, Mohan R, Paganetti H, et al. National Effort to Re-establish Heavy Ion Cancer Therapy in the United States. Front Oncol. 2022;12:880712. https://doi.org/10.3389/fonc.2022.880712.
Glowa C, Karger CP, Brons S, Zhao D, Mason RP, Huber PE, et al. Carbon ion radiotherapy decreases the impact of tumor heterogeneity on radiation response in experimental prostate tumors. Cancer Lett. 2016;378:97–103. https://doi.org/10.1016/j.canlet.2016.05.013.
Glowa C, Peschke P, Brons S, Neels OC, Kopka K, Debus J, et al. Carbon ion radiotherapy: impact of tumor differentiation on local control in experimental prostate carcinomas. Radiat Oncol. 2017;12:174. https://doi.org/10.1186/s13014-017-0914-9.
Glowa C, Peschke P, Brons S, Debus J, Karger CP. Intrinsic and extrinsic tumor characteristics are of minor relevance for the efficacy of split-dose carbon ion irradiation in three experimental prostate tumors. Radiother Oncol J Eur Soc Ther Radiol Oncol. 2019;133:120–4. https://doi.org/10.1016/j.radonc.2018.12.017.
Huang Y, Huang Q, Zhao J, Dong Y, Zhang L, Fang X, et al. The impacts of different types of Radiation on the CRT and PDL1 expression in Tumor cells under Normoxia and Hypoxia. Front Oncol. 2020;10:1610. https://doi.org/10.3389/fonc.2020.01610.
Iijima M, Okonogi N, Nakajima NI, Morokoshi Y, Kanda H, Yamada T, et al. Significance of PD-L1 expression in carbon-ion radiotherapy for uterine cervical adeno/adenosquamous carcinoma. J Gynecol Oncol. 2020;31:e19. https://doi.org/10.3802/jgo.2020.31.e19.
Zhou H, Tu C, Yang P, Li J, Kepp O, Li H, et al. Carbon ion radiotherapy triggers immunogenic cell death and sensitizes melanoma to anti-PD-1 therapy in mice. Oncoimmunology. 2022;11:2057892. https://doi.org/10.1080/2162402X.2022.2057892.
Helm A, Tinganelli W, Simoniello P, Kurosawa F, Fournier C, Shimokawa T, et al. Reduction of lung metastases in a mouse osteosarcoma model treated with Carbon ions and Immune Checkpoint inhibitors. Int J Radiat Oncol Biol Phys. 2021;109:594–602. https://doi.org/10.1016/j.ijrobp.2020.09.041.
Shimokawa T, Ma L, Ando K, Sato K, Imai T. The future of combining Carbon-Ion Radiotherapy with Immunotherapy: evidence and progress in mouse models. Int J Part Ther. 2016;3:61–70. https://doi.org/10.14338/IJPT-15-00023.1.
Durante M, Brenner DJ, Formenti SC. Does Heavy Ion Therapy Work through the Immune System? Int J Radiat Oncol Biol Phys. 2016;96:934–6. https://doi.org/10.1016/j.ijrobp.2016.08.037.
Durante M, Formenti S. Harnessing radiation to improve immunotherapy: better with particles? Br J Radiol. 2020;93:20190224. https://doi.org/10.1259/bjr.20190224.
Tubin S, Yan W, Mourad WF, Fossati P, Khan MK. The future of radiation-induced abscopal response: beyond conventional radiotherapy approaches. Future Oncol. 2020;16:1137–51. https://doi.org/10.2217/fon-2020-0063.
Cavalieri S, Vitolo V, Barcellini A, Ronchi S, Facoetti A, Campo C, et al. Immune checkpoint inhibitors and Carbon iON radiotherapy in solid cancers with stable disease (ICONIC). Future Oncol. 2023;19:193–203. https://doi.org/10.2217/fon-2022-0503.
Paganetti H. Relative biological effectiveness (RBE) values for proton beam therapy. Variations as a function of biological endpoint, dose, and linear energy transfer. Phys Med Biol. 2014;59:R419–72. https://doi.org/10.1088/0031-9155/59/22/R419.
Riva G, Cavallo I, Gandini S, Ingargiola R, Pecorilla M, Imparato S, et al. Particle Radiotherapy for Skull Base Chondrosarcoma: a clinical series from Italian National Center for Oncological Hadrontherapy. Cancers (Basel). 2021;13. https://doi.org/10.3390/cancers13174423.
Mizoe J-E, Hasegawa A, Takagi R, Bessho H, Onda T, Tsujii H. Carbon ion radiotherapy for skull base chordoma. Skull Base. 2009;19:219–24. https://doi.org/10.1055/s-0028-1114295.
Cuccia F, Fiore MR, Barcellini A, Iannalfi A, Vischioni B, Ronchi S, et al. Outcome and Toxicity of Carbon Ion Radiotherapy for Axial Bone and Soft tissue sarcomas. Anticancer Res. 2020;40. https://doi.org/10.21873/anticanres.14260.
Vischioni B, Dhanireddy B, Severo C, Bonora M, Ronchi S, Vitolo V, et al. Reirradiation of salivary gland tumors with carbon ion radiotherapy at CNAO. Radiother Oncol. 2020;145. https://doi.org/10.1016/j.radonc.2020.01.004.
Held T, Windisch P, Akbaba S, Lang K, El Shafie R, Bernhardt D, et al. Carbon Ion Reirradiation for Recurrent Head and Neck Cancer: a single-institutional experience. Int J Radiat Oncol Biol Phys. 2019;105:803–11. https://doi.org/10.1016/j.ijrobp.2019.07.021.
Bhattacharyya T, Koto M, Windisch P, Ikawa H, Hagiwara Y, Tsuji H, et al. Emerging role of Carbon Ion Radiotherapy in Reirradiation of Recurrent Head and Neck cancers: what have we achieved so far? Front Oncol. 2022;12:888446. https://doi.org/10.3389/fonc.2022.888446.
Yamada S, Takiyama H, Isozaki Y, Shinoto M, Ebner DK, Koto M, et al. Carbon Ion Radiotherapy for locally recurrent rectal Cancer of patients with prior pelvic irradiation. Ann Surg Oncol. 2022;29:99–106. https://doi.org/10.1245/s10434-021-10876-4.
Barcellini A, Vitolo V, Cobianchi L, Peloso A, Vanoli A, Mirandola A, et al. Re-irradiation with Carbon Ion Radiotherapy for pelvic rectal Cancer recurrences in patients previously irradiated to the Pelvis. Vivo (Brooklyn). 2020;34:1547–53. https://doi.org/10.21873/invivo.11944.
Shiba S, Okonogi N, Kato S, Wakatsuki M, Kobayashi D, Kiyohara H, et al. Clinical impact of re-irradiation with Carbon-ion Radiotherapy for Lymph Node Recurrence of Gynecological Cancers. Anticancer Res. 2017;37:5577–83. https://doi.org/10.21873/anticanres.11991.
Barcellini A, Vitolo V, Mastella E, Mirandola A, Valvo F. Letter to the editor concerning re-irradiation in gynaecological cancers, present experiences and future hopes. J Radiat Oncol. 2019;8:355–6. https://doi.org/10.1007/s13566-019-00396-w.
Tambas M, van der Laan HP, Steenbakkers RJHM, Doyen J, Timmermann B, Orlandi E, et al. Current practice in proton therapy delivery in adult cancer patients across Europe. Radiother Oncol J Eur Soc Ther Radiol Oncol. 2022;167:7–13. https://doi.org/10.1016/j.radonc.2021.12.004.
Xiang M, Chang DT, Pollom EL. Second cancer risk after primary cancer treatment with three-dimensional conformal, intensity-modulated, or proton beam radiation therapy. Cancer. 2020;126:3560–8. https://doi.org/10.1002/cncr.32938.
Facoetti A, Barcellini A, Valvo F, Pullia M. The role of particle therapy in the risk of radio-induced second tumors: a review of the literature. Anticancer Res. 2019;39. https://doi.org/10.21873/anticanres.13641.
König L, Haering P, Lang C, Splinter M, von Nettelbladt B, Weykamp F, et al. Secondary malignancy risk following Proton vs. X-ray treatment of Mediastinal Malignant Lymphoma: a comparative modeling study of thoracic organ-specific Cancer risk. Front Oncol. 2020;10:989. https://doi.org/10.3389/fonc.2020.00989.
Loap P, Orlandi E, De Marzi L, Vitolo V, Barcellini A, Iannalfi A, et al. Cardiotoxicity model-based patient selection for Hodgkin lymphoma proton therapy. Acta Oncol. 2022;61:979–86. https://doi.org/10.1080/0284186X.2022.2084639.
Barcellini A, Cassani C, Orlandi E, Nappi RE, Broglia F, Delmonte MP et al. Is motherhood still possible after pelvic carbon ion radiotherapy? A promising combined fertility-preservation approach. Tumori 2024:3008916231218794. https://doi.org/10.1177/03008916231218794.
Rosenbrock J, Baues C, Vasquez-Torres A, Clivio A, Fogliata A, Borchmann P, et al. Volumetric modulated arc therapy versus intensity-modulated proton therapy in the irradiation of infra diaphragmatic Hodgkin Lymphoma in female patients. Acta Oncol. 2022;61:81–8. https://doi.org/10.1080/0284186X.2021.1986230.
Pereira S, Orlandi E, Deneuve S, Barcellini A, Chalaszczyk A, Behm-Ansmant I, et al. The normal, the Radiosensitive, and the ataxic in the era of Precision Radiotherapy: a narrative review. Cancers (Basel). 2022;14. https://doi.org/10.3390/cancers14246252.
Paganetti H. Range uncertainties in proton therapy and the role of Monte Carlo simulations. Phys Med Biol. 2012;57:R99–117. https://doi.org/10.1088/0031-9155/57/11/R99.
Li H, Dong L, Bert C, Chang J, Flampouri S, Jee K-W, et al. AAPM Task Group Report 290: respiratory motion management for particle therapy. Med Phys. 2022;49:e50–81. https://doi.org/10.1002/mp.15470.
Mori S, Knopf A-C, Umegaki K. Motion management in particle therapy. Med Phys. 2018;45:e994–1010. https://doi.org/10.1002/mp.12679.
Ciocca M, Mirandola A, Molinelli S, Russo S, Mastella E, Vai A, et al. Commissioning of the 4-D treatment delivery system for organ motion management in synchrotron-based scanning ion beams. Phys Med PM Int J Devoted Appl Phys Med Biol off J Ital Assoc Biomed Phys. 2016;32:1667–71. https://doi.org/10.1016/j.ejmp.2016.11.107.
Mastella E, Mirandola A, Russo S, Vai A, Magro G, Molinelli S, et al. High-dose hypofractionated pencil beam scanning carbon ion radiotherapy for lung tumors: dosimetric impact of different spot sizes and robustness to interfractional uncertainties. Phys Medica PM an int J devoted to Appl Phys to Med Biol Off. J Ital Assoc Biomed Phys. 2021;85:79–86. https://doi.org/10.1016/j.ejmp.2021.05.004.
Mastella E, Molinelli S, Pella A, Vai A, Maestri D, Vitolo V, et al. 4D strategies for lung tumors treated with hypofractionated scanning proton beam therapy: dosimetric impact and robustness to interplay effects. Radiother Oncol J Eur Soc Ther Radiol Oncol. 2020;146:213–20. https://doi.org/10.1016/j.radonc.2020.02.025.
Meschini G, Vai A, Barcellini A, Fontana G, Molinelli S, Mastella E, et al. Time-resolved MRI for off-line treatment robustness evaluation in carbon-ion radiotherapy of pancreatic cancer. Med Phys. 2022;49:2386–95. https://doi.org/10.1002/mp.15510.
Molinelli S, Vai A, Russo S, Loap P, Meschini G, Paganelli C, et al. The role of multiple anatomical scenarios in plan optimization for carbon ion radiotherapy of pancreatic cancer. Radiother Oncol J Eur Soc Ther Radiol Oncol. 2022;176:1–8. https://doi.org/10.1016/j.radonc.2022.09.005.
Mastella E, Molinelli S, Magro G, Mirandola A, Russo S, Vai A, et al. Dosimetric characterization of carbon fiber stabilization devices for post-operative particle therapy. Phys Med PM Int J Devoted Appl Phys Med Biol off J Ital Assoc Biomed Phys. 2017;44:18–25. https://doi.org/10.1016/j.ejmp.2017.11.008.
Cobianchi L, Peloso A, Vischioni B, Panizza D, Fiore MR, Fossati P, et al. Surgical spacer placement prior carbon ion radiotherapy (CIRT): an effective feasible strategy to improve the treatment for sacral chordoma. World J Surg Oncol. 2016;14:1–9.
Barcellini A, Mirandola A, Fiore MR, Orlandi E, Cobianchi L. Omentum flap as a spacer before carbon ion radiotherapy for gynecological recurrences. A technical note. Cancer Radiother J La Soc Fr Radiother Oncol. 2022;26:599–603. https://doi.org/10.1016/j.canrad.2021.12.009.
Nagai S, Nagayoshi K, Mizuuchi Y, Fujita H, Ohuchida K, Ohtsuka T, et al. Laparoscopic spacer placement for recurrent sacral chordoma before carbon ion radiotherapy: a case report. Asian J Endosc Surg. 2020;13:582–5. https://doi.org/10.1111/ases.12792.
Lee D, Komatsu S, Terashima K, Toyama H, Matsuo Y, Takahashi D, et al. Surgical spacer placement for proton radiotherapy in locally advanced pancreatic body and tail cancers: initial clinical results. Radiat Oncol. 2021;16:3. https://doi.org/10.1186/s13014-020-01731-z.
Narukawa T, Aibe N, Tsujimoto M, Shiraishi T, Kimoto T, Suzuki G, et al. Increasing rectum-prostate distance using a hydrogel spacer to reduce radiation exposure during proton beam therapy for prostate cancer. Sci Rep. 2023;13:18319. https://doi.org/10.1038/s41598-023-45557-7.
Komatsu S, Wang T, Terashima K, Demizu Y, Anzai M, Suga M, et al. Innovative combination treatment to Expand the indications of particle therapy: Spacer Placement surgery using Bio-absorbable Polyglycolic Acid Spacer. J Am Coll Surg. 2024;238:119–28. https://doi.org/10.1097/XCS.0000000000000873.
Molinelli S, Magro G, Mairani A, Matsufuji N, Kanematsu N, Inaniwa T, et al. Dose prescription in carbon ion radiotherapy: how to compare two different RBE-weighted dose calculation systems. Radiother Oncol J Eur Soc Ther Radiol Oncol. 2016;120:307–12. https://doi.org/10.1016/j.radonc.2016.05.031.
Orlandi E, Barcellini A, Vischioni B, Fiore MR, Vitolo V, Iannalfi A, et al. The role of Carbon Ion Therapy in the changing Oncology Landscape-A Narrative Review of the literature and the Decade of Carbon Ion experience at the Italian National Center for Oncological Hadrontherapy. Cancers (Basel). 2023;15. https://doi.org/10.3390/cancers15205068.
Ahern V, Adeberg S, Fossati P, Garrett R, Hoppe B, Mahajan A, et al. An international approach to estimating the indications and number of eligible patients for carbon ion radiation therapy (CIRT) in Australia. Radiother Oncol J Eur Soc Ther Radiol Oncol. 2023;187:109816. https://doi.org/10.1016/j.radonc.2023.109816.
Funding
The authors declare that they have no funding and no financial support.
Open access funding provided by Università degli Studi di Pavia within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Contributions
Conceptualisation: E.O and A.B.; writing-original draft preparation: E.O and A.B.; writing-review and editing: S.L; A.M.C; S.R; A.C; L.P.C; M.R.; M.B.
Corresponding author
Ethics declarations
Institutional review board statement
Not applicable.
Informed consent statement
Not applicable.
Conflict of interest
Authors declare no conflict of interest with regard to the current article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Orlandi, E., Lillo, S., Camarda, A.M. et al. The clinical roadmap in a dual-beam hadrontherapy centre: tumour-based and patient-tailored selection criteria, management of range uncertainties and oncological patient pathway. Health Technol. (2024). https://doi.org/10.1007/s12553-024-00865-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12553-024-00865-4