Abstract
Diffusion-weighted MR Imaging is a rapidly emerging technique, that allows in-vivo mapping processes of the water diffusion in tissues. It has the potential capabilities for clinical application in breast imaging. The aim of this study was to find out the optimal b-value for calculation of ADC value for differential diagnosis of breast lesions. A total of 124 subjects (mean age 46 years) with 141 lesions were included. The protocol consists of axial T2 sequence for lesion localization and measurement and DW sequence with three sets of b-values of 0, 300, 600, and 1000 s/mm2. The mean ADC values of the breast lesions for b-values (0, 300, 600, and 1000) were 1.75 ± 0.18 × 10−3mm2/sec, 1.66 ± 0.12 × 10−3mm2/sec and 1.57 ± 0.15 × 10−3mm2/sec for the benign lesions and 1.26 ± 0.048 × 10−3mm2/sec, 1.14 ± 0.11 × 10−3mm2/sec and 0.93 ± 0.14 × 10−3mm2/sec for malignant lesions respectively. Statistical significant differences were noted on the ADC value of benign and malignant lesions among the three sets of b values (p = 0.001). ADC values of malignant lesion was significantly lower compared to benign lesions. The AUC (0.998) was substantially large for b-value of 0,600 s/mm2 with a threshold ADC cut off value of 1.28 × 10−3mm2/sec with 98.4% sensitivity, 93.2% specificity and 98.5% positive predictive value(PPV). In conclusion, diffusion weighted imaging has the ability for differential diagnosis of breast lesions with the optimal b value of 0,600 s/ mm2. DWI is a reliable tool for characterising breast lesions and may increase the overall specificity of breast MRI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Magnetic Resonance Imaging (MRI) has been a modality of choice for diagnosis and evaluation of breast tumors, especially in high breast density, where lesions were occult on mammogram and sonography. Diffusion-weighted MRI is a rapidly emerging technique, that allows the in-vivo mapping processes of the diffusion of water in the tissues; it can delineate the microstructure of a targeted tissue such as extracellular space, tissue cellularity etc. [1]. It is highly susceptible to the displacement of water molecules at the diffusion scale, which is a three-dimensional process and quantifies the diffusion index, which reflects the apparent mean diffusivity, commonly known as the Apparent Diffusion Coefficient (ADC), which estimate the degree of diffusion along three orthogonal directions [2]. Diffusion Weighted Imaging (DWI) is already an established magnetic resonances diagnostic tool in the field of medicine, but its clinical application for breast lesions evaluation is challenging due to the technical limitations and lack of standardized protocol. Diffusion-Weighted MR uses Echo Planar Imaging (EPI) technique, which yields rapid image acquisition and contrast agent scan can be avoided. The quantitative data analysis provided by this sequence helps in differential diagnosis and evaluation of breast lesions. Hence, this technique has potential competence as an alternative for invasive biopsy procedures. Diffusion weighted MRI techniques have high prospect to enhance the sensitivity and specificity for detecting and diagnosing of benign and malignant breast lesions [3].
The earlier studies have reported that the use of DWI technique for breast imaging shows variation in their sensitivity and specificity, probably due to the variation in technical parameters, such as b-value selection, the strength of the magnetic gradient and also the methods for calculation of ADC value in the region of interest [4, 5]. However, due to lack of standardized approach and guidelines for the application of DWI in screening and detection of breast lesions, the data quality varies widely, though DWI have manifest the prospective capabilities for ameliorating the Positive Predictive Value (PPV) for detecting the breast lesion in MRI. Therefore, further investigation should be conducted in order to standardize the protocol. The main objective of the present study was to determine the optimal b-value for calculation of ADC value for differentiating the benign from malignant breast lesions.
2 Methods
The ethical approval for this prospective study was received from the institutional ethics committee. The study was explained to all the participants and written informed consents were obtained.
2.1 Subjects
The study subjects were females with the age group of 25—60 years (mean age 46 years). A total of 124 subjects with breast lesions of various BIRADS grading (BIRADS 1–5) as detected in ultrasonography and mammography were recruited for breast MRI, with total number of lesions count of 141. The mean diameter of the lesions was 6.42 cm. MRI scan was scheduled between 7 to 15th days of the menstrual cycle for premenopausal subjects. Patients with cystic lesions and silicone implants were excluded from the study.
2.2 MRI Techniques
MRI scan was performed using Philips Achieve 1.5 Tesla MRI (Philips, Netherland). Bilateral MRI breast scan was conducted, where the contralateral side was taken for evaluation of the normal fibro-glandular breast tissue. The diseased side was evaluated for the detection of breast lesions. The examination protocol consists of conventional pulse sequences -Axial T2W [6] (TE/TR: 120/3500 ms, slice thickness: 1 mm, matrix: 340 × 512, NSA: 2) for lesion localization and lesion size measurement and DW sequence (TE/TR: 95/8200 ms, flip angle: 90°, slice thickness: 3 mm, matrix: 192 × 192, signal averages: 4) with three combinations of b-values (b = 0, 300, 600, and 1000 s/ mm2). The acquired diffusion series were registered prior to creating the corresponding ADC maps for each b values.
2.3 Image analysis
T2 FS sequence was used for lesion localization, and lesion size was measured at its maximal dimension in cm. The diffusion-weighted series for all the b-values combination were post-processed in the extended workstation.
For calculating the ADC values, the necrotic tissues identified in the morphological images of T2 FS weighted sequence were avoided [7]. ADC values were calculated using an ADC mapping. For a lesion measuring of 1–2 cm, three ROIs were calculated, 2.1 cm and above, six ROIs were individually placed basically for each pixel. The calculated ADC values of the ROIs for each lesion were averaged and tabulated. The margins of the lesions were avoided during ADC measurements in order to curtail the effect of partial volume averaging. For normal fibro glandular tissues, six ROIs were considered and calculated. Two radiologists with more than 10 years of experience in MR Breast Imaging retrospectively interpreted and analyzed the obtained DW images; however, they were blinded from the histopathological reports.
2.4 Statistical analysis
The data were statistically analyzed using Statistical Package for the Social Sciences (SPSS) v16.0. Descriptive statistic was used to calculate the mean ADC values. Analysis of variance (ANOVA) statistic was used to determine the statistical difference in the ADC values for benign lesions, malignant lesions and fibro glandular tissues for all sets of b-values where p-value of 0.05 was set as a level of significance. Receiver Operating Characteristic (ROC) curve analysis was used to determine the cut off ADC values between malignant and benign breast lesions and area under the curve (AUC) was used to determine optimal b-value for the calculation of ADC values. Further, the diagnostic accuracy of multiple b-value for determining the cut off ADC values was analyzed in terms of sensitivity, specificity and positive predictive value (PPV). Youden index (J) were also calculated to evaluate the diagnostic levels for investigation and differential diagnosis of a disease.
3 Results
The total samples for the present study were collected from 62 breasts with 62 benign lesions, 62 breasts with 73 malignant lesions and 62 fibro-glandular tissues. The mean ADCs of the breast lesions and fibro glandular tissues for all the set of b values (300, 600, and 1000) are tabulated in Table 1.
The mean ADCs of the breast tissues for all the set of b values (0, 300, 600, and 1000) was 1.75 ± 0.18 × 10−3mm2/sec, 1.66 ± 0.12 × 10−3mm2/sec and 1.57 ± 0.0.15 × 10−3mm2/sec for benign lesions and 1.26 ± 0.048 × 10−3mm2/sec, 1.14 ± 0.11 × 10−3mm2/sec and 0.93 ± 0.14 × 10−3mm2/sec for malignant lesions respectively. The ADC value for the fibro glandular tissues in all the sets of b value was 2.14 ± 0.25 × 10−3mm2/sec, 2.04 ± 0.29 × 10−3mm2/sec and 1.90 ± 0.26 × 10−3mm2/sec respectively. The ADC value difference for benign and malignant lesions was statistically significant among the three sets of b values (p = 0.001).
The mean ADC values for benign, malignant and fibro glandular tissues showed lower ADC values with the increase in the b-values, that is, the b-value of 0,300 showed higher ADC values whereas the b-value of 0,1000 showed lower ADC values and the difference noted were statistically significant (p < 0.001). Also, note that ADC value for malignant is significantly lower than the ADC for benign lesion and fibro glandular tissues.
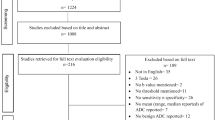
According to the ROC (Fig. 1) the area under the curve (AUC) for b-value of 0,300 s/mm2 was 0.986, for b-value of 0,600 s/mm2 was 0.998 and for b-value of 0,1000 s/mm2 was 0.993. The AUC was substantially large when the b-value was 0,600 s/mm2, indicating that it was the optimal b-value for differentiating the benign and malignant breast lesions. The ADC values were also analyzed at different cut-off points to determine the prime threshold point as well as the diagnostic power of each b value.
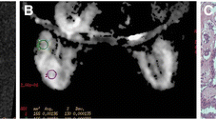
A 39-year-old female was diagnosed with a solid breast lesion on left side of the breast. MRI scan was performed with T2 FS and DWI sequences with three sets of b value (300,600 and 1000 s/mm2). According to the mammography the lesion was reported to be BIRADS III. In the histopathological result the lesion was reported as Infiltrating Ductal Carcinoma (Malignant lesions). (a) Axial T2 FS sequence of the bilateral breast shows an oval shaped tumor measuring 3.31 cm in the left breast. (b, c and d) The diffusion weighted images with multiple b value of 300,600 and 1000 s/mm2 demonstrated ADC values of the malignant lesions as 1.34, 1.28 and 1.22 × 10−3mm2/sec, for fibro glandular tissue the ADC value were 2.63, 2.21,1.97 × 10−3mm2/sec respectively. The ADC value decreases with an increase in b value. The ADC maps reflect the densely packed tumor cells pattern, which inhibits effective motion of water molecules and restricts diffusion
For b value of 0,300 s/mm2, the ADC cut off threshold value is 1.34 × 10−3mm2/sec which yielded 95.3% sensitivity, 93.2% specificity, and 95.8% PPV. Whereas, for b value of 0,600 s/mm2, the ADC cut off threshold value is 1.28 × 10−3mm2/sec with 98.4% sensitivity, 93.2% specificity, and 98.5% PPV and for b value of 0,1000 s/mm2, the ADC cut off threshold value is 1.17 × 10−3mm2/sec with 96.9% sensitivity, 95% specificity, and 98% PPV.
Evaluating the diagnostic performances levels has become a main method in the investigation and differential diagnosis of a disease. Hence, Youden index captures (both sensitivity and specificity) the performance of a diagnostic test. The Youden index (J) for the three b values 300,600, and 1000 s/mm2 were 0.89, 0.92,0.92 respectively. Therefore, the Youden index (J) for b value of 0, 600 and 0,1000 s/mm2 indicate that there was an almost perfect test for differentiating benign from malignant breast lesions (Table 2). Therefore, the optimal b-value in DWI for differential diagnosis of benign and malignant breast tissues in 1.5 T MRI was 0, 600 with a cut off threshold value of 1.28 × 10−3mm2/sec and AUC of 0.998 with 98.4% sensitivity, 93.2% of specificity and 98.5% of Positive Predictive Value, indicating the high diagnostic performance of the quantitative analysis of Diffusion Weighted MR Imaging in differential diagnosis of benign and malignant breast lesions.
4 Discussion
With the advancement in medical technology, besides Ultrasonography and Mammography, MRI is a globally accepted diagnostic technique for the evaluation of the breast tissues and abnormalities. DWI has a dormant capability in the approach to access the structural characteristics of the tissues and also to characterize breast lesions. To improve the sensitivity and specificity for the detection of breast cancer at an early stage, several diverse techniques have endeavored. In this present study, we evaluated the sensitivity of multiple b values for differential diagnosis of breast cancer tissues, as a means to improve the clinical diagnosis and treatment. Differential diagnosis of breast lesion with DWI, can be quantified with ADC values, which was assessed in ADC mapping by the signal attenuation due to the restricted movement of the water molecules in the tissues with high cellular density [8, 9]. In the present study, we found that the optimal b value for differentiating breast lesion between benign and malignant breast lesions is 0,600 s/mm2 with the mean ADC of 1.66 ± 0.12 × 10−3mm2/sec for benign lesions, 1.14 ± 0.11 × 10−3mm2/sec for malignant lesions, and 2.04 ± 0.29 × 10−3mm2/sec for fibro-glandular tissues with 98.4% and 93.2% sensitivity and specificity respectively. We also noted remarkably lower ADC value for malignant lesions as compared to the benign lesions in the three sets of b values, but the b value of 0,600 s/mm2 has higher AUC and high sensitivity and specificity.
In the present study we noted, the ADC value for benign, malignant and fibro-glandular tissues was lower in 0, 1000 than 0, 600 s/mm2 (Table 2) as compared to 0,300 s/mm2 which indicate that the ADC values decreases with increasing b values (Fig. 2). This was probably owing to the elimination of the effect of perfusion circulation. Similarly, in a study conducted by Kaiji Inoue [9] and also the previous studies [7, 10, 11] have reported that the ADC value was also influenced by perfusion if small b value was applied. In the tissues, the microscopic motion includes water diffusion and blood microcirculation within the capillary network, therefore the ADC value is highly affected by both diffusion and perfusion. In malignant breast tumor, due to the extent of micro vessels, the ADC value can be vigorously influenced by perfusion if small b value was applied.
The result of the present study is similar to the previous study conducted by Jung Pak et al. [11] who urges the use of b-values lower than 750 s/mm2 for detecting breast tumors. According to Guangwei et al. [12] recommendation, b value greater than 500 should be used for breast MRI so that the ADC measurement will be insensitive to perfusion and hence the ADC mapping value would be within an ace to the true diffusion coefficient.
Similarly, we noted in the previous studies [8, 13,14,15,16,17,18,19] they have reported detection and evaluation of breast lesions in DWI with multiple b value ranging from 250 -1500 s/mm2 and with variable ADC cut off value. Studies that used low b value ranging from 250- 800 s/mm2 have reported slightly higher ADC values for both benign and malignant lesion as compared to studies that used b values of 1000–1500 s/mm2. Qinghua Min et al. [8] reported that the optimal b-value for breast lesion differentiation is 800 s/mm2 with a threshold of 1.23 × 10−3mm2/sec. Guangwei et al. [12] reported with b value of 600 s/mm2 the cut off threshold for differentiating benign from malignant breast lesion is 1.44 × 10−3mm2/sec. Reiko Woodhams et al. [20] in the year 2005 reported, the ADC value to be 2.05 ± 0.27 × 10−3mm2/sec for fibro-glandular tissue, 1.12 ± 0.24 × 10−3mm2/sec for malignant lesions, 1.09 ± 0.23 × 10−3mm2/sec for IDC, and 1.42 ± 0.42 × 10−3mm2/sec for NIDC with b values of 0,750 s/mm2. Whereas Wei Zhang et al. [14] reported the ADC value of Malignant lesion to be 1.010 ± 0.234 × 10−3mm2/sec and Benign lesion to be 1.648 ± 0.392 × 10−3mm2/sec for the b value of 0, 800 s/mm2. Lalitha Palle N et al. [19] in their study reported the range of ADC value for benign and malignant lesions to be 1.3 to 1.5 × 10−3mm2/sec and 0.85 to 1.1 × 10−3mm2/sec respectively with the sensitivity of 97.22% and a specificity of 100% for the b-values of 0,500 and 1000 s/mm2. Similarly, in the study conducted by Uma Sharma et al. [21] they reported the ADC of malignant lesions to be 1.02 ± 0.17 × 10−3mm2/sec, benign lesions to be 1.57 ± 0.26 × 10−3mm2/sec and normal breast tissues to be 1.78 ± 0.13 × 10−3mm2/sec with the sensitivity of 92.5% and specificity of 91.1% for the b values of 0,500,1000 s/mm2. In a study conducted by Pratiksha Yadav et al. [18] with the b value of 800 s/mm2 the reported ADCs for benign and malignant lesions was 1.905 ± 0.59 × 10−3mm2/sec, and 1.014 ± 0.47 × 10−3mm2/sec respectively.
Several studies conducted previously used b value of 1000 s/mm2, but the reported mean ADC values and threshold cut off value for the differential diagnosis of benign and malignant lesions were varying. C Marini et al. [5] used b values of 0, 1000 s/mm2 and reported the mean ADCs for benign and malignant lesions to be 1.48 ± 0.37 × 10−3mm2/sec and 0.95 ± 0.18 × 10−3mm2/sec respectively. Similarly, Mi Jung Pak et al. [11] conducted a study using b values of 0,1000 s/mm2 and reported ADCs for invasive ductal carcinoma to be 0.89 0.18 × 10−3mm2/sec mm2, DCIS to be 1.17 ± 0.18 × 10−3mm2/sec, benign lesions to be 1.41 ± 0.56 × 10−3mm2/sec and the normal fibro glandular tissue to be 1.51 ± 0.29 × 10−3mm2/sec. Likewise, Ebru Yılmaz et al. [17] reported the ADC values for benign were 1.584 × 10−3mm2/sec and malignant lesions were 0.884 × 10−3mm2/sec with 88% sensitivity and 87% specificity using b-value of 0,1000 s/mm2. CWS Wan et al. [15] also reported the mean ADCs for benign and malignant lesions using the b Value of 1000 s/mm2. Their study reported the mean ADC for malignant and benign lesions to be 0.89 ± 0.29 × 10−3mm2/sec and 1.27 ± 0.42 × 10−3mm2/sec respectively with the sensitivity of 85.9% and specificity of 77%. Whereas, Kaiji Inoue et al. [9] reported with multiple b value of 0, 250, 500, 750, 1000 s/mm2 and mean ADC threshold ADC + 1.65 × SD, for benign lesions (1.50 ± 0.38 × 10−3mm2/sec) and malignant lesions (0.98 ± 0.19 × 10−3mm2/sec), with 94.5% sensitivity, 80% specificity. In a study conducted by Miho et al. [22] they used higher b value of 0, 1500 s/mm2 and reported the ADC value to be 0.90 ± 0.18 × 10−3mm2/sec for malignant lesions, and 1.21 ± 0.29 × 10−3mm2/sec for benign lesions with a threshold value of 1.11 × 10−3mm2/sec and 93.2%, 55.6%, 73.3% of sensitivity, specificity, positive predictive value (PPV) respectively. Similarly, in a study conducted by Reiko Woodham et al. [7] used a b values of 0, 1500 s/mm2 and reported the ADC value of 0.9 ± 0.2 × 10−3mm2/sec and 1.3 ± 0.3 × 10−3mm2/sec for malignant and benign lesions respectively.
Therefore, we noted in all the previous studies the b value ranges from 250 up to 1500 s/mm2 with varying values of ADCs for both benign and malignant breast lesions and therefore the threshold cut off value for differential diagnosis were also not constant. However, accordant with the earlier studies, the present study revealed that the ADC value was significantly lower for malignant lesions as compared to benign lesions. It was also reported that the tissues microstructure such as necrosis or marked fibrosis, highly influenced the ADC value because water diffusion was restricted in severe fibrosis. Therefore, the ADC value of fibrous adenomas or invasive ductal carcinomas with prominent fibrosis may be decreased, and the ADCs of invasive ductal carcinomas with central necrosis may be increased [10]. We also noted that the precise positioning of the ROIs in the lesions were highly crucial for ADC measurement. Therefore, we avoided all regions suspected of necrosis. We also noted that prolonged DWI acquisition scanning times might be essential in order to increase the signal-to-noise ratio (SNR) and maneuver a decrease in slice thickness, hence in the current study we performed the scan with 1 mm thickness. According to the present results, we noted that the ADC values manifest less variability and were more specific since we excluded lesions < 1 cm in size, to avoid partial volume artifacts and also low b value (< 1000 mm/sec2) was used to minimize the perfusion circulation effect.
Among the other factors that may affect the ADC values, the higher strength of the magnetic field such as 3 T may have higher sensitivity and specificity, though the present study and other studies cited in this article were done on a 1.5 T. However, we expect that these issues will be improved with advances in imaging instruments and software.
Diffusion-weighted MRI is a promising technique that can be incorporated into standard clinical breast MRI protocols and increase the PPV for MRI breast assessment. Another advantage of DWI is this technique can be easily added to the screening protocol, especially of younger women with denser breasts. In several cases where contrast-enhanced imaging is contraindicated, DWI is a preferable method than T1- and T2-weighted imaging for detecting breast tumors. Therefore, in order to acquire accurate, cut off threshold value for breast tumor characterizations, standardized of b value in DWI should be recognized.
According to the recommendation of Mi Junk Park et al. [11] the ADC value of breast lesions should be juxtaposed to fibro glandular tissue because the ADC value was variable with different gradient factors. In the present study we compared the ADC value of the lesions with the fibro- glandular tissues, for the three set of b value (300,600 and 1000 s/mm2) and the results shows that there was a significant difference (p < 0.05) between the ADC value of benign, malignant and fibro-glandular tissues but the b value of 0,600 s/mm2 has the highest sensitivity and specificity for differential diagnosis.
We recommend to include DWI sequence in the breast MR protocol, for good reciprocity with histology finding. The b value and also the ADC threshold value for differential diagnosis of breast lesions should be standardized through large studies conducted at multiple centers. The results of the study can be translated into routine practice by using the following steps. In order to detect and perform differential diagnosis of the lesion a T2 weighted fat suppressed sequence should be obtained for accurate lesion localization and size measurement, followed by DWI sequence with the b-value of 0,600 s/mm2. Thereafter, ADC should be calculated using ADC mapping with a minimum selection of 3 ROIs, in which the ADC calculation should be done pixel by pixel. Differential diagnosis of the lesion can be obtained by using the ADC cut off value of 1.28 X 10–3 mm2/sec. ADC value below the cut off is considered as malignant lesion and ADC value above cut off is considered to be benign lesion.
5 Conclusion
Diffusion-weighted sequence constitutes a potential resource for both qualitative and quantitative evaluation of breast pathology. It manifests potential capabilities for improving the positive predictive value for the detection of breast cancer. DWI sequence can be implemented as a screening tool for high-risk population because of its short scan time and high sensitivity. According to our study, the optimal b value for differential diagnosis of breast lesion using ADC value for benign, malignant and fibro-glandular tissue was 0, 600 s/mm2. We conclude that the ADC value increases the diagnostic sensitivity and specificity of Diffusion-Weighted sequence, which is an effective tool for treatment and management in clinical setting.
Availability of data and material
Not Applicable.
Code availability
Not Applicable.
Change history
19 February 2022
Springer Nature’s version of this paper was updated to present the funding note.
References
Koh DM, Collins DJ. Diffusion-weighted MRI in the body: Applications and challenges in oncology. Am J Roentgenol. 2007;188(6):1622–35.
Pereira FPA, Martins G, Carvalhaes de Oliveira R de V. Diffusion magnetic resonance imaging of the breast. Magn Reson Imaging Clin N Am [Internet]. 2011;19(1):95–110. Available from: https://doi.org/10.1016/j.mric.2010.09.001
Hetta W. Role of diffusion weighted images combined with breast MRI in improving the detection and differentiation of breast lesions. Egypt J Radiol Nucl Med [Internet]. 2015;46(1):259–70. Available from: https://doi.org/10.1016/j.ejrnm.2014.10.009
Partridge SC, Demartini WB, Kurland BF, Eby PR, White SW, Lehman CD. Differential Diagnosis of Mammographically and Clinically Occult Breast Lesions on Diffusion- Weighted MRI. 2010;570:562–70.
Marini C, Iacconi C, Giannelli M, Cilotti A, Moretti M, Bartolozzi C. Quantitative diffusion-weighted MR imaging in the differential diagnosis of breast lesion. Eur Radiol. 2007;17(10):2646–55.
Bickelhaupt S, Laun F, Lederer W, Daniel H, Stieber A, Delorme S, et al. Diffusion-Weighted MR Mammography ( DWI-MRM ) – Potential in the Clarification of Suspicious Lesions Detected by X-Ray Mammography. 2016;(65):70–4.
Woodhams R, Kakita S, Hata H, Iwabuchi K, Umeoka S, Mountford CE, et al. Diffusion-weighted imaging of mucinous carcinoma of the breast: Evaluation of apparent diffusion coefficient and signal intensity in correlation with histologic findings. Am J Roentgenol. 2009;193(1):260–6.
Min Q, Shao K, Zhai L, Liu W, Zhu C, Yuan L, et al. Differential diagnosis of benign and malignant breast masses using diffusion-weighted magnetic resonance imaging. World J Surg Oncol [Internet]. 2015;13:32. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=4328303&tool=pmcentrez&rendertype=abstract
Inoue K, Kozawa E, Mizukoshi W. Usefulness of diffusion-weighted imaging of breast tumors : quantitative and visual assessment. 2011;429–36.
Kinoshita T, Yashiro N, Ihara N, Funatu H, Fukuma E, Narita M. Diffusion-weighted half-fourier single-shot turbo spin echo imaging in breast tumors: Differentiation of invasive ductal carcinoma from fibroadenoma. J Comput Assist Tomogr. 2002;26(6):1042–6.
Mi JP, Eun SC, Bong JK, Yon KI, Jun HB. The role of diffusion-weighted imaging and the apparent diffusion coefficient (ADC) values for breast tumors. Korean J Radiol. 2007;8(5):390–6.
Jin G, An N, Jacobs MA, Li K. The Role of Parallel Diffusion-Weighted Imaging and Apparent Diffusion Coefficient (ADC) Map Values for Evaluating Breast Lesions. Preliminary Results Acad Radiol. 2010;17(4):456–63.
Abowarda MH, Hasan DI, Elteeh OA. Predictive value of ADC mapping in discriminating probably benign and suspicious breast lesions. Egypt J Radiol Nucl Med [Internet]. 2015;46(2):545–51. Available from: https://doi.org/10.1016/j.ejrnm.2015.02.004
Zhang W, Jin GQ, Liu JJ, Su DK, Luo N Bin, Xie D, et al. Diagnostic performance of ADCs in different rois for breast lesions. Int J Clin Exp Med. 2015;8(8):12096–104.
Wan CWS, Lee CY, Lui CY, Fong CY, Lau KCH. Apparent diffusion coefficient in differentiation between malignant and benign breast masses: Does size matter? Clin Radiol [Internet]. 2016;71(2):170–7. Available from: https://doi.org/10.1016/j.crad.2015.11.006
Sharma U, Sah RG, Agarwal K, Parshad R, Seenu V, Mathur SR, et al. Potential of diffusion-weighted imaging in the characterization of malignant, benign, and healthy breast tissues and molecular subtypes of breast cancer. Front Oncol. 2016;6(MAY):1–11.
Yılmaz E, Sarı O, Yılmaz A, Ucar N, Aslan A, Inan I, et al. Diffusion-Weighted Imaging for the Discrimination of Benign and Malignant Breast Masses; Utility of ADC and Relative ADC. J Belg Soc Radiol 2018;102.
Yadav P, Chauhan S. Effectivity of combined diffusion-weighted imaging and contrast-enhanced {MRI} in malignant and benign breast lesions. Polish J Radiol [Internet]. 2018;83:82–93. Available from: https://doi.org/10.5114/2Fpjr.2018.74363
Palle L, Reddy B. Role of diffusion MRI in characterizing benign and malignant breast lesions. Indian J Radiol Imaging [Internet]. 2009;19(4):287. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=2797740&tool=pmcentrez&rendertype=abstract
Woodhams R, Matsunaga K, Iwabuchi K, Kan S, Hata H, Kuranami M, et al. Diffusion-Weighted Imaging of Malignant Breast Tumors. J Comput Assist Tomogr. 2005;29(5):644–9.
Sharma U. Potential of Diffusion-Weighted imaging in the characterization of Malignant. Benign, and healthy Breast Tissues and Molecular subtypes of Breast cancer. 2016;6(May):1–11.
Ochi M, Kuroiwa T, Sunami S, Murakami J, Miyahara S, Nagaie T, et al. Diffusion-weighted imaging (b value = 1500 s/mm2) is useful to decrease false-positive breast cancer cases due to fibrocystic changes. Breast Cancer. 2013;20(2):137–44.
Acknowledgements
We would like to acknowledge the guidance of Dr. Anurag Ayachit and (Late) Dr. Smiti Sripathi during the planning and development of this research work. Their encouragement and constructive suggestions were very much appreciated.
Funding
Open access funding provided by Manipal Academy of Higher Education, Manipal.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Mrs. Winniecia Dkhar, Dr. Rajagopal Kadavigere and Dr. Samir Paruthikunnan Mustaffa. The first draft of the manuscript was written by Mrs. Winniecia Dkhar and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
Approval was obtained from the Institutional ethics committee, Kasturba Hospital. The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Conflicts of interest
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Dkhar, W., Kadavigere, R. & Mustaffa, S.P. Quantitative Evaluation for Differential Diagnosis of Breast Lesions in Diffusion-Weighted MR Imaging. Health Technol. 11, 1269–1275 (2021). https://doi.org/10.1007/s12553-021-00604-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12553-021-00604-z