Abstract
The paper examines risk factors associated with child mortality in the scheduled tribe population in India and explains differences in child mortality outcomes between the scheduled tribe and the non-scheduled tribe population. A weighted total of 7,962 deaths of children aged under 5 years occurred within the 5 years preceding the survey in our pooled sample of NFHS 3 and NFHS 4 where scheduled tribe children contribute approximately 59% of the death. A Cox proportional hazard regression is estimated using several predictors. The findings suggest that there is a significant decline in neonatal, infant and under-five mortality among the tribal population in the last 10 years. Cox regression results indicate that timely implementation of ante-natal care, postnatal care and institutional delivery are important factors behind the reduction in neonatal as well as infant mortality in tribal-dominated areas; whereas proper family planning method, lower birth order of the child and maternal education, media exposure along with autonomy of mother are effective in reducing under-five mortality. Further, early initiation of breastfeeding and exclusive breastfeeding can reduce child mortality more effectively. Therefore, policies and programmes on maternal care and family planning, and the creation of awareness at the community level on reproductive maternal and child health will need to be emphasised to reduce child mortality in the tribal population.


Source: Author’s calculations based on NFHS-3 and NFHS-4

Source: Author’s calculations based on NFHS-4

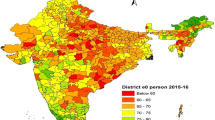
Source: Author’s calculations based on Health Management Information System (HMIS) 2019, Government of India

Source: Author’s calculations based on Health Management Information System (HMIS) 2019, Government of India
Similar content being viewed by others
Notes
Report on the Advisory Committee on the Revision of the list of Scheduled tribes and scheduled caste, 1965 https://ruralindiaonline.org/en/library/resource/the-report-of-the-advisory-committee-on-the-revision-of-the-lists-of-scheduled-castes-and-scheduled-tribes/
National Family and Health Survey in India is similar to Demographic and Health Surveys in other countries. The Multistage sampling framework is used to create a representative sample from all India. It provides information on households’ standard of living, child mortality, health care services, reproductive health and nutrition status of women and child at national and state level.
Due to huge cultural diversity, other North Eastern States except Assam are not included in the study.
The media exposure of women is defined on the basis of three broad indicators, i.e., access and frequency of listening to the radio, watching television and reading newspapers or magazines. Based on frequency of access, to these sources, high media exposure is defined as exposure to any of the three sources every day, while low media exposure is based on rare or no access to media. Those that are not in the category of high or low media exposure are classified as having medium exposure.
The NFHS 4 questionnaire asked about three areas of women's autonomy in decision making. These are, own health care, making household purchases and visits to her family or friends. Each question had six responses: (1) respondent alone; (2) respondent and husband/partner; (3) respondent and other person; (4) husband/partner alone; (5) someone else and (6) others. To create a binary variable for the analysis, we grouped the first two responses under the head having own autonomy. The remaining four responses were categorised as the woman having no say in the decision or low autonomy. Therefore, if a woman can take her own decision in all three domains then she has higher autonomy. In all other cases her autonomy is low.
Timely ANC visit and care helps the mother to connect with formal health system, usage of skill attendant at birth and promote knowledge related to child care like breastfeeding, early post natal care, and optimal family planning.
References
Anderson, I., Robson, B., Connolly, M., Al-Yaman, F., Bjertness, E., King, A., Tynan, M., Madden, R., Bang, A., Coimbra, C. E., Jr., & Pesantes, M. A. (2016). Indigenous and tribal peoples’ health (the lancet-lowitja institute global collaboration): A population study. Lancet, 388, 131–157.
Andriano, L., & Monden, C. W. S. (2019). The causal effect of maternal education on child mortality: Evidence from a quasi-experiment in Malawi and Uganda. Demography, 56, 1765–1790.
Basu, A.K., Byambasuren, T., Chau, N.H. and Khanna, N. (2020). Cooking Fuel Choice, Indoor Air Quality and Child Mortality in India. IZA DP No. 13295.
Baqui, A. H., Ahmed, S., El Arifeen, S., Darmstadt, G. L., Rosecrans, A. M., Ishtiaq, M., Rahman, S. R., Nazma, B., Arif B. A. M., Habbiur, R. S., Emma, K. W., Peter, J. W., Mathuram, S., & Robert, E. B. (2009). Effect of timing of first postnatal care home visit on neonatal mortality In Bangladesh: A observational cohort study. British Medical Journal, 339, b282.
Bora, J. K., Raushan, R., & Lutz, W. (2019). The persistence influence of caste on under five mortality: Factors that explain the caste based gap in high focused Indian states. PLoS ONE, 14(8), e0211086.
Bora, J. K., & Saikia, N. (2018). Neonatal and under-five mortality rate in Indian districts with reference to sustainable development goal 3: An analysis of the national family health survey Of India (NFHS): 2015–16. PLoS ONE, 13(7), e0201125.
Bhatia, M., Dwivedi, L. K., Ranjan, M., Dixit, P., & Putcha, V. (2019). Trends, patterns and predictive factors of infant and child mortality in well-performing and underperforming states of India: A secondary analysis using national family health surveys. British Medical Journal Open, 9, e023875. https://doi.org/10.1136/bmjopen-2018-023875
Borooah, V. K. (2005). Caste, inequality, and poverty in India. Review of Development Economic, 9(3), 399–414.
Cox, D. R. (1972). Regression models and life tables. Journal of Royal Statistical Society, 34, 187–220.
Das, M.B., Kapoor, S., Nikitin, D. (2010). A Closure Look At Child Mortality Among Adivasi In India. Policy Research working paper; no. WPS 5231. Washington, DC: World Bank http://documents.worldbank.org/curated/en/955711468044086021/pdf/WPS5231.pdf
Dommaraju, P., Agadjanian, V., & Yabiku, S. (2008). The pervasive and persistent influence of caste on child mortality in India. Population Research Policy Review, 27(4), 477–495.
Fatema, K., & Lariscy, J. (2021). Mass media exposure and maternal healthcare utilization in South Asia. SSM-Population Health, 11(2020), 100614.
Ghimire, P. R., Agho, K. E., Ezeh, O. K., Renzaho, A., Dibley, M., & Raynes-Greenow, C. (2019). Under-five mortality and associated factors: Evidence from the nepal demographic and health survey (2001–2016). International Journal of Environmental Research and Public Health, 16(7), 1241. https://doi.org/10.3390/ijerph16071241
Government of India (2018). Tribal health in India: Bridging the Gap And A RoadMap for The Future. Ministry of Health and Family Welfare, Government of India and Ministry of Tribal Affairs, Government of India.
Houweling, T. A. J., & Kunst, A. E. (2010). Socio-economic inequalities in childhood mortality in low- and middle-income countries: A review of the international evidence. British Medical Bulletin, 93(1), 7–26.
Jain, N., Singh, A., & Pathak, P. (2013). Infant and child mortality in India: Trends in inequalities across economic groups. Journal of Population Research, 30, 347–365.
Kuntla, S., Goli, S., & Jain, K. (2014). Explaining sex differentials in child mortality in India: Trends and determinants. International Journal of Population Research, 1–7. https://doi.org/10.1155/2014/649741
Liu, L., Oza, S., Hogan, D., Perin, J., Rudan, I., Lawn, J. E., Cousens, S., Mathers, C., & Black, R. E. (2015). Global, regional, and national causes of child mortality in 2000–13, with projections to inform post-2015 priorities: An updated systematic analysis. Lancet, 385, 430–440.
Mohanty, S. K. (2011). Multidimensional poverty and child survival in India. PLoS ONE, 6(10), e26857.
Narain, J. P. (2019). Health of tribal populations in India: How long can we afford to neglect? The Indian Journal of Medical Research, 149(3), 313–316. https://doi.org/10.4103/ijmr.IJMR_2079_18
Pamuk, E. R., Fuchs, R., & Lutz, W. (2011). Comparing relative effects of education and economic resources on infant mortality in developing countries. Population Development Review, 37(4), 637–664.
Panagariya, A., & More, V. (2014). Poverty by social, religious and economic groups in india and its largest states: 1993-1994 to 2011-2012. Indian Growth and Development Review, 7(2), 202–230.
Po, J. Y., & Subramanian, S. V. (2011). Mortality burden and economic status in India. PLoS ONE, 6(2), e16844.
Ram, B., Singh, A., & Yadav, A. (2017). The persistent caste divide in India’s infant mortality : a study of dalits (ex untouchables), adivasis(indigenous peoples), other backward classes, and forward castes. Canadian Studies in Population, 43(3–4), 249–263.
Ranjan, M., Dwivedi, L. K., & Mishra, R. (2017). Infant mortality differentials among the tribal and non tribal populations of central and eastern India. International Journal of Population Studies, 2(2), 26–43.
Saikia, N., Singh, A., Jasillionis, D., & Ram, F. (2013). Explaining the rural-urban gap in infant mortality In India. Demographic Research, 29, 473–506.
Subramanian, S. V., Smith, G. D., & Subramanian, M. (2006). Indigenous health and socio economic status In India. PLoS Medical, 3(10), e421.
UN Interagency Group of Child Mortality Estimation (2019). Levels And Trends Of Child Mortality, UNICEF New York, 2019.
UNICEF (2017). Levels And Trends In Child Mortality Report (2017). UN Inter-agency Group for Child Mortality Estimation.
Van de Poel, E., & Speybroeck, N. (2009). Decomposing malnutrition inequalities between scheduled castes and tribes and the remaining indian population. Ethnicity and Health., 14(3), 271–287. https://doi.org/10.1080/13557850802609931
Vishwakarma, M., Shekhar, C., Dutta, M., & Yadav, A. (2019). Gaps in infant and child mortality among social groups and linkages with institutional delivery and child immunization using census and national family health survey (2015–16). Journal of Public Health: Theory to Practice, 28, 293–303.
Whitworth, A., & Stephenson, R. (2012). Birth spacing, sibling rivalry and child mortality in India. Social Science Medicine., 55(12), 2107–2119.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
See Tables
7,
8,
9,
10,
11.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dutta, S. Risk factors for child survival among tribal dominated states in India: a pooled cross sectional analysis. J Pop Research 39, 391–416 (2022). https://doi.org/10.1007/s12546-022-09288-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12546-022-09288-2