Abstract
Background
Weight loss in diabetes prevention programmes has been shown to be associated with participants’ age, socio-economic status, and ethnicity. However, little is known about how these differences relate to attendance and whether such differences can be mediated by other potentially modifiable factors. Differential effectiveness across these factors may exacerbate health inequalities.
Method
Prospective analysis of participant data collected by one provider of the standardised national NHS diabetes prevention programme in England. Mediation analysis was performed via a structural equation model to examine whether the number of attended sessions mediated the associations of age, socio-economic status, and ethnicity with follow-up weight. The group-level factor of number of attended sessions was examined using multiple linear regression as a benchmark; multilevel linear regression using three levels (venue, coach, and group); and fixed effects regression to account for venue-specific and coach-specific characteristics.
Results
The associations of age, socio-economic status, and ethnicity with follow-up weight were all mediated by the number of attended sessions. Group size was associated with attendance in an inverted ‘U’ shape, and the number of days between referral and group start was negatively associated with attendance. Time of day, day of the week, and the number of past groups led by the coach were not associated with attendance.
Conclusion
Most of the differences in weight loss initially attributed to socio-demographic factors are mediated by the attendance of the diabetes prevention programme. Therefore, targeted efforts to improve uptake and adherence to such programmes may help alleviate inequalities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The increasing rate of Type 2 diabetes is a public health concern, putting pressure on health systems globally [1]. Lifestyle programmes aiming to support behavioural change to prevent the onset of Type 2 diabetes have been an effective way to reduce this incidence [2, 3]. Pragmatic diabetes prevention interventions can achieve this, but their effectiveness depends on the degree to which participants adhere to programme guidelines [4, 5]. In England, the prevalence of Type 2 diabetes has been on the rise, with its rate in 2020 being at 4.7% [6]. In 2016, the National Health Service (NHS) established a universal Diabetes Prevention Programme (NHS-DPP) targeting people who have nondiabetic hyperglycaemia. The delivery of the NHS-DPP is conducted by independent providers that deliver the service to according to specific guidelines set by the NHS [7].
Research into the fidelity of design of the NHS-DPP shows that the programme is largely delivered according to the guidelines set out by the Department of Health and Social Care [8, 9]. However, programme delivery of the NHS-DPP varies substantially and this variation has implications for the patient experience, especially in terms of venue quality, scheduling, and group size, which have been proven important factors of participant satisfaction with programme [10]. Substantial variation is also observed in staff training [11]. All these delivery characteristics affect patient experience and therefore potentially affect adherence to the intervention.
Whilst there are established differences in the effectiveness of the NHS-DPP across age, socio-economic status, and ethnicity [12], little is known about what causes such differential responses. There are several possible modifiable factors that may contribute to this, including aspects of the intervention itself such as the size of the group or skills of the person delivering the intervention (implementation-level factors), as well as aspects of the way the individuals respond to the intervention (e.g. degree of attendance and adherence to behavioural recommendations). Implementation and participant behavioural factors may be potentially modifiable and therefore represent an opportunity to reduce or eliminate responses to the NHS-DPP that contribute to inequalities [13].
Adherence to behavioural interventions is an important component of their effectiveness. In the NHS-DPP there are several ways in which participants can be said to adhere to the intervention including attendance and the degree to which they implement the multiple behavioural recommendations for lifestyle change. Although adherence to behavioural recommendations is likely to be most strongly related to outcome, this is difficult to measure. As recommendations may vary across different providers of the NHS-DPP, benchmarking across providers is challenging. Session attendance is a critical measure of participant adherence and previous research has demonstrated it has a significant impact on the effectiveness of behavioural interventions, such as diabetes prevention or weight management programmes [12, 14,15,16]. Higher attendance has been strongly associated with greater weight loss in several trials [17,18,19]. Session attendance can be measured across programmes and therefore it may be a good candidate for benchmarking performance relating to inequality across programmes. Whilst differences in participation across sociodemographic groups in behavioural interventions are well established, little research has explored whether group-level modifiable factors, such as group size, time and place, are associated with differential participation using prospective models [20].
The way NHS-DPPs are implemented may also be related to differential outcomes between groups. Process evaluations of the DPP suggest several candidates for factors that might influence participant experience, engagement, and adherence to the NHS-DPP [21]. The delivery of these behavioural interventions takes place within groups, usually referred by primary care practises. Thus, in addition to individual-level characteristics, there are aggregate factors that affect the uptake and participation to these programmes, such as referring practise characteristics [22] or characteristics of the way the programme is delivered by coaches [10].
This study aims to identify potentially modifiable factors influencing the differential socio-demographic response to the NHS-DPP. Using data from one provider of the NHS-DPP, this study examines whether the number of attended sessions mediates the associations of individual-level characteristics with weight loss. In addition, some group-level factors of the number of attended sessions are examined to provide guidance for future programme design.
Methods
The data used in this study were provided by one of the four commercial providers of the framework 1 of the NHS-DPP, Reed Momenta. This involved extracting anonymised data on the eligible individuals that were referred to participate to the NHS-DPP through this provider. These referred individuals were invited for an initial assessment and then booked into a group led by a coach at a designated venue to follow the 18-session programme over 9 months.
This study design provides different sources of variation in data collection that we exploit to explore group-level factors of attendance. Specifically, each venue hosted multiple groups, some of which started at the same date. Coaches were assigned to multiple groups, some within the same venue, and others at different venues. Whilst the participant allocation to the venue is mostly driven by geographical criteria and is highly endogenous, the participant allocation to the group within the venue is largely based on scheduling and resources relating the venue and the coach.
The outcome variables examined are follow-up weight in kgs (weight at last session attended) and the number of sessions attended. Predictors include participant-level and group-level characteristics. The participant-level predictors used are sex, age in 5-year groups, Index of Multiple Deprivation (IMD) quintile (an area-level measure of relative deprivation calculated for each of the Lower Layer Super Output Areas in England across the following domains: income; employment; health deprivation and disability; education, skills training; crime; barriers to housing and services; and living environment), and self-reported ethnicity. As we are interested in weight change, we also include weight at the first session in the regression. With the inclusion of initial weight, the analysis of follow-up weight is effectively examining weight change. The group-level variables are the following: group size and group size squared (to test for non-linearities) based on the number of participants that started each group; groups per coach based on the number of groups that each coach has delivered up until the current group, starting with the value of one and increasing by one with each subsequent group; number of days between referral and group starting date (in logarithm as this is highly skewed and has no zero values), time of the day, day of the week sessions run, and dummy variables for region and year (to account for regional differences and time differences, respectively).
The analysis in this study is divided in two parts. The first part explores these individual-level factors using a mediation analysis to examine whether the number of attended sessions mediated the associations of the participant-level characteristics with follow-up weight. The second part explores these group-level factors, by examining their relationship with attendance whilst controlling for the individual-level factors and accounting for unobserved heterogeneity at various levels in the implementation.
The mediation analysis is performed on follow-up weight (outcome), sessions (potential mediator), and the individual-level characteristics, calculating total, direct, and indirect effects of the individual-level characteristics. This was done using the Baron and Kenny approach [23], where the shares of the effects that are mediated by sessions can be calculated as the ratio of indirect over total. Figure 1 provides a graph of the mediation analysis strategy along with equations of the models that are estimated to retrieve all three effects. Inference was performed via bootstrap replications, as is standard in mediation analysis [24].
For the analysis of the group-level factors, the current design allows us to account for unobserved heterogeneity at various levels, by accounting for unobserved venue- and coach-specific characteristics. For example, groups in a small church in the city centre might be smaller in size compared to groups in a large modern community centre in a suburban area. By exploiting the fact that we have multiple groups within the same venue, we account for venue-specific characteristics (which may relate to the large geographic and socio-economic disparities) and estimate within-venue effects. Similarly, we account for coach-specific characteristics (sex, age, education, motivation, etc.) and estimate the effect of coach delivery experience (proxied by the number of groups the coach had started before the group’s first day). We present three specifications, using linear regression analysis as a benchmark, multilevel (mixed-effects) linear regression, and a fixed effects estimation (within estimator). All statistical analysis was conducted in Stata [25].
Results
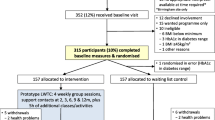
Between June 2016 and December 2019, 61,066 eligible individuals were referred to Reed-Momenta to participate in the NHS-DPP. Of those, 40,359 (66%) attended an initial assessment and 20,655 (34%) attended at least one session (i.e. started the programme). Those with missing information on weight were excluded, resulting to an analytical sample of 15,902 individuals. These were referred from 1314 General Practitioner (GP) practises, with 2055 groups delivered in 330 venues (mainly in London, North-West, and South-East) from a total of 147 coaches. The flowchart in Fig. 2 shows the number of participants that remain or dropout at each stage of the recruitment process and those included in the analytical sample.
Each venue hosted an average of six groups. Conditional on starting on the same day, the average number of groups was two per venue, whereas conditioning on starting the same month, the average was 2.5 per venue. Each venue had an average of three coaches. Each coach instructed, on average, in about six venues and to 13 groups, with each group having an initial size of about 11 participants. Table 1 presents descriptive statistics for all variables used in the analysis.
The results of the mediation analysis of follow-up weight and sessions attended are presented in Table 2. In the total-effects analysis, there are strong significant associations of follow-up weight with age, IMD quintile, and ethnicity, but not with sex. Participants of older age, higher IMD, Asian, other mixed, and missing ethnicity, have a greater weight loss. All these predictors are associated with more sessions attended, except for ethnicity. In the direct-effects model which includes the individual predictors and sessions, none of these predictors remains significant and their magnitudes are close to zero. Moreover, every session attended is associated with a weight loss of 0.281 kg (p < 0.001). Initial weight remains a strong predictor in both total- and direct-effects models.
Indirect effects (and proportion mediated) are calculated for those categories which have a statistically significant total effect, as otherwise there is no effect in the first place (except for initial weight which is included only as a control). The large indirect effects reveal that for age, IMD, and ethnicity, their associations with follow-up weight are mediated via sessions attended, in most cases at about 70%. This is also confirmed in a fully interacted model of attended sessions and the three individual-level predictors (Fig. 3).
Examining the associations with group-level variables, all models indicate strong associations with group size and days between referral and programme start dates (Table 3). The benchmark model also shows a positive association with groups-per-coach, the 3 pm time slot, and Saturday. These associations are not present in the two models that account for unobserved heterogeneity. The positive sign of the linear term and negative sign of the quadratic term of group size reveal a relationship with the number of sessions attended that has an inverted ‘U’ shape, where the maximum is reached at between 15 and 18 participants. The logarithm of the number of days between referral and programme start has a strong negative relationship, suggesting that an increase in days by 100% (doubling the time between referral and start) is associated with a decrease of 0.3 sessions attended (p < 0.001). The groups-per-coach has no relationship with sessions attended, and the same is true for time of the day and day of the week.
Discussion
This study aimed to identify potentially modifiable characteristics of the implementation or participant response to an NHS-DPP relating to differential effects between social and demographic groups. Greater attendance to the programme was associated with a lower follow-up weight during the programme, indicating a dose–response relationship. A decrease in follow-up weight of 0.28 kg per session attended was found in the current study. This is similar to a larger evaluation of the NHS-DPP that found a 0.32 kg weight loss per session [12], and other commercial weight management programmes, with the attendance-weight loss relationship holding for both for referred and self-referred programmes [15, 16, 19]. Whilst this relationship is evident, the mechanism via which this happens remains unclear. Attendance might be related to programme adherence or other behavioural components, which may differ between people [16]. Indeed, a systematic review of weight loss interventions failed to reach conclusion towards a consistent set of factors that predict dropout [26]. This may be because such psychological and behavioural determinants are usually largely unobserved and confound the analysis.
Age was an important predictor of attendance, with older participants attending far more sessions. Other studies have shown a similar pattern of attendance with age [19, 22, 27, 28]. The relationship with ethnicity and deprivation is more mixed in the literature, with some studies finding evidence of differences, whilst others do not [13, 19, 29], but this may depend on the type of measurement, especially in terms of measuring deprivation. A study that also used the IMD in Scotland found a similar pattern of decreasing attendance with increasing deprivation [22]. In line with other studies [19, 22], there was no difference in attendance between men and women.
The present finding of an association between individual characteristics and the number of sessions attended are in line with the results of a study which sampled data from all NHS-DPP providers that looked at predictors of initial attendance and of completion [12]. Lower attendance rates were found for younger participants, those from the most deprived quintiles, and for Asian and mixed ethnic groups, but not for sex.
This study found that attendance was associated with group size following an inverted ‘U’ shape, with maximum attendance for participants in groups with around 15–18 people. This is consistent with previous work showing group size is an important determinant of participant’s experience. In a qualitative evaluation of the NHS-DPP, participants in groups of 10–15 people reported more positive responses, compared to participants in groups of more than 15 people [11]. Another study on paediatric weight management interventions found that engagement was lower for participants in groups with more than 20 members, compared to groups with less than 20 members [30]. The results of the present study provide empirical support to suggest the maximum group size for optimising attendance and intervention effectiveness should be between the recommendations of 15 people by the National Institute for Clinical Excellence (NICE) [31] and 20 people by the NHS [7]. It is not known why larger group sizes may contribute to inequalities. One possibility is that coaches in larger groups may not have enough time to identify and deal with the specific needs of individuals from lower socioeconomic status and non-white ethnicities, resulting in lower engagement and premature dropout. Further research is needed on this issue.
Heterogeneity in coaches is another potential source of variation in adherence among groups. There are several sources of heterogeneity between coaches, such as professional status, delivery style, and experience. In this study, we used coach experience as one potential source of heterogeneity as previous systematic reviews on the effectiveness of the diabetes prevention programme in the USA, showed no differences when intervention delivered by clinically trained professionals or lay educators [32], and data on delivery style was not available. In the current study, the positive association in the benchmark model did not remain in neither of the main models. That is that although there are differences between coaches with high number of groups and coaches with low number of groups, within-coach, in other words, accounting for unobserved heterogeneity in coaches’ characteristics, groups-per-coach had no association with attendance. This result can be translated that there is no learning curve (nor fatigue) during the duration of the programme. The lack of information on coaches’ backgrounds, including prior experience between this programme, limits the interpretations of the analysis into just that. It is worth noting that, at the time, coaches had only limited mentoring, quality assurance and management support.
The timing of the sessions is also an important component in the delivery of such programmes. Indeed, research which aggregated data across four NHS-DPP providers showed that the providers with the lowest completion rates were the ones with more scheduling issues [10]. Results from the benchmark model suggest a possible decrease in attendance at 3 pm, which coincides with schools’ closure time, and a possible increase in attendance on Saturdays, possibly as this is part of the weekend. Interestingly, these differences vanish in the main models. Overall, the null effects of time of the day and day of the week in this study can be interpreted in two ways. Either scheduling does not matter for attendance, or participants self-selected (or session organisers selected) into the most appropriate schedule, thus minimising the disturbance in the daily or weekly routine. The negative association of the number of days between referral and programme start is indicative of the importance of timing, as delays might negatively affect individuals’ motivation which is an important determinant of participation [33].
The present study is unique in its focus on understanding potentially modifiable factors influencing the differential effectiveness of the NHS-DPP. Using appropriate methods to account for unobserved heterogeneity due to venue- and coach-specific characteristics, a set of clear policy suggestions are made, that are easy to implement by providers of similar programmes. We did not implement multiple imputations in the analysis, as the independent variables have no missing data (except ethnicity for which a separate category was created and included). Thus, we do not expect the incomplete cases to have any beneficial contribution. Indeed, previous analysis of this data found no differences in the sign and magnitude between complete-case and multiple imputations [12]. However, this study has a number of limitations. First, it uses data only from one of the four programme providers, which was slightly different in that it offered 18 sessions, whilst the others offered 13 in total. Second, participants self-select themselves to the sessions they attend, so the dose–response relationship and the mediation analysis results may be driven by factors associated with this selection, such as own motivation. Third, attendance reflects only the total number of sessions attended. Additional information on the exact sessions that each participant attended could reveal patterns of attendance, especially since weight loss from session to session is an important factor of subsequent dropout [34]. Fourth, the lack of HbA1c information, as low values of HbA1c measurement during the programme is another potential predictor of dropout [35]. The provider aimed to measure HbA1c at substantially less frequent intervals than weight, thus ruling out any analysis of the association between HbA1c change and sessions. This can be problematic, as some individuals who have prediabetes might have weight in the healthy range, but still, a target of modest weight loss would still result in clinically significant outcomes (36). Fifth, other coach characteristics, such as prior experience may be important factors that affect attendance. Sixth, despite accounting for venue-specific characteristics, the lack of randomisation in group allocation, may still hinder estimation of the relationships between the group-level characteristics examined in this study.
This study examined the relationship between attendance, follow-up weight, and individual-level characteristics. Most of the socio-demographic differences in weight loss are mediated by attendance to the programme. Examining further the predictors of attendance, the analysis revealed an inverted ‘U’ shape relationship between group size and attendance, with maximum attendance observed for groups of 15–18 people. Another important predictor identified was the number of days lapsed between referral and programme group start, indicating a decline of the ‘referral effect’ and the subsequent motivation to adhere to the programme. In contrast, neither scheduling (measured by time of the day and day of the week) nor programme familiarity of the instructor (measured by the number of past programme groups coached for each instructor) were associated with attendance.
This study adds to the existing literature on DPP by highlighting the importance of considering potentially modifiable influences on sociodemographic variation in response to such programmes. It demonstrates the importance of attendance as a potentially modifiable determinant of outcome. More research is needed to understand the modifiable drivers of attendance and retention, including specifically why groups who derive the least benefit from the DPP are more likely to attend fewer sessions. It points to the importance of efforts to maximise the implementation of existing DPPs to address health inequalities, in conjunction with efforts to create bespoke pathways for those groups that are much less engaged.
References
Saeedi P, Petersohn I, Salpea P, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas. Diabetes Res Clin Pract. 2019;157: 107843.
Tuomilehto J, Lindström J, Eriksson JG, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. 2001;344(18):1343–50.
Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6):393–403.
Dunkley AJ, Bodicoat DH, Greaves CJ, et al. Diabetes prevention in the real world: effectiveness of pragmatic lifestyle interventions for the prevention of type 2 diabetes and of the impact of adherence to guideline recommendations: a systematic review and meta-analysis. Diabet Care. 2014;37(4):922–33.
Galaviz KI, Weber MB, Straus A, Haw JS, Narayan KV, Ali MK. Global diabetes prevention interventions: a systematic review and network meta-analysis of the real-world impact on incidence, weight, and glucose. Diabet Care. 2018;41(7):1526–34.
Barron E, Bakhai C, Kar P, et al. Associations of type 1 and type 2 diabetes with COVID-19-related mortality in England: a whole-population study. Lancet Diabetes Endocrinol. 2020;8(10):813–22.
England NHS (2016) Service specification no. 1: Provision of behavioural interventions for people with non-diabetic hyperglycaemia. https://www.england.nhs.uk/wp-content/uploads/2016/08/dpp-service-spec-aug16.pdf
Hawkes R, Cameron E, Bower P, French DP. Does the design of the NHS diabetes prevention Programme intervention have fidelity to the programme specification? A document analysis. Diabet Med. 2020;37(8):1357–66.
French DP, Hawkes RE, Bower P, Cameron E. Is the NHS diabetes prevention programme intervention delivered as planned? An observational study of fidelity of intervention delivery. Ann Behav Med. 2021;55(11):1104–15.
Hawkes RE, Cameron E, Cotterill S, Bower P, French DP. The NHS diabetes prevention programme: an observational study of service delivery and patient experience. BMC Health Serv Res. 2020;20(1):1–12.
Hawkes RE, Cameron E, Miles LM, French DP. The fidelity of training in behaviour change techniques to intervention design in a National Diabetes Prevention Programme. Int J Behav Med. 2021;28(6):671–82.
Valabhji J, Barron E, Bradley D, et al. Early outcomes from the English National health service diabetes prevention programme. Diabetes Care. 2020;43(1):152–60.
Graham J, Tudor K, Jebb S, et al. The equity impact of brief opportunistic interventions to promote weight loss in primary care: secondary analysis of the BWeL randomised trial. BMC Med. 2019;17(1):1–9.
Wadden TA, Foster GD, Wang J, et al. Clinical correlates of short-and long-term weight loss. Am J Clin Nutr. 1992;56(1):271S-S274.
Stubbs R, Brogelli D, Pallister C, Whybrow S, Avery A, Lavin J. Attendance and weight outcomes in 4754 adults referred over 6 months to a primary care/commercial weight management partnership scheme. Clinical Obesity. 2012;2(1–2):6–14.
Stubbs RJ, Morris L, Pallister C, Horgan G, Lavin JH (2015) Weight outcomes audit in 1.3 million adults during their first 3 months’ attendance in a commercial weight management programme. BMC Public Health 15(1):1–13
Acharya SD, Elci OU, Sereika SM, et al. Adherence to a behavioral weight loss treatment program enhances weight loss and improvements in biomarkers. Patient Prefer Adherence. 2009;3:151.
Bartfield JK, Stevens VJ, Jerome GJ, et al. Behavioral transitions and weight change patterns within the PREMIER trial. Obesity. 2011;19(8):1609–15.
Piernas C, MacLean F, Aveyard P, et al. Greater attendance at a community weight loss programme over the first 12 weeks predicts weight loss at 2 years. Obes Facts. 2020;13(4):349–60.
Birch JM, Jones RA, Mueller J et al (2022) A systematic review of inequalities in the uptake of, adherence to, and effectiveness of behavioral weight management interventions in adults. Obes Rev. e13438
Begum S, Povey R, Ellis N, Gidlow C, Chadwick P (2022) Influences of decisions to attend a national diabetes prevention programme from people living in a socioeconomically deprived area. Diab Med e14804
Blane DN, McLoone P, Morrison D, Macdonald S, O’Donnell CA. Patient and practice characteristics predicting attendance and completion at a specialist weight management service in the UK: a cross-sectional study. BMJ Open. 2017;7(11): e018286.
Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173.
Imai K, Keele L, Tingley D. A general approach to causal mediation analysis. Psychol Methods. 2010;15(4):309.
StataCorp (2017) Stata statistical software: Release 15. College Station, TX: StataCorp.
Moroshko I, Brennan L, O’Brien P. Predictors of dropout in weight loss interventions: a systematic review of the literature. Obes Rev. 2011;12(11):912–34.
Wadden TA, West DS, Neiberg RH, et al. One-year weight losses in the Look AHEAD study: factors associated with success. Obesity. 2009;17(4):713–22.
Fabricatore AN, Wadden TA, Moore RH, Butryn ML, Heymsfield SB, Nguyen AM. Predictors of attrition and weight loss success: results from a randomized controlled trial. Behav Res Ther. 2009;47(8):685–91.
Chao D, Farmer DF, Sevick MA, Espeland MA, Vitolins M, Naughton MJ. The value of session attendance in a weight-loss intervention. Am J Health Behav. 2000;24(6):413–21.
Nobles J, Griffiths C, Pringle A, Gately P. Design programmes to maximise participant engagement: a predictive study of programme and participant characteristics associated with engagement in paediatric weight management. Int J Behav Nutr Phys Act. 2016;13(1):1–10.
National Institute for Health Care Excellence (2017) Type 2 diabetes: prevention in people at high risk. London: National Institute for Health and Care Excellence (NICE)
Ali MK, Echouffo-Tcheugui JB, Williamson DF. How effective were lifestyle interventions in real-world settings that were modeled on the Diabetes Prevention Program? Health Aff. 2012;31(1):67–75.
Webber KH, Tate DF, Ward DS, Bowling JM. Motivation and its relationship to adherence to self-monitoring and weight loss in a 16-week Internet behavioral weight loss intervention. J Nutr Educ Behav. 2010;42(3):161–7.
Yackobovitch-Gavan M, Steinberg D, Endevelt R, Benyamini Y. Factors associated with dropout in a group weight-loss programme: a longitudinal investigation. J Hum Nutr Diet. 2015;28:33–40.
Barron E, Misra S, English E, et al. Experience of point-of-care HbA1c testing in the English National Health Service Diabetes Prevention Programme: an observational study. BMJ Open Diabetes Res Care. 2020;8(2): e001703.
Taylor R, Holman RR. Normal weight individuals who develop type 2 diabetes: the personal fat threshold. Clin Sci. 2015;128(7):405–10.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Poupakis, S., Kolotourou, M., MacMillan, H.J. et al. Attendance, Weight Loss, and Participation in a Behavioural Diabetes Prevention Programme. Int.J. Behav. Med. 30, 904–913 (2023). https://doi.org/10.1007/s12529-022-10146-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12529-022-10146-x