Abstract
Background
Although physical activity (PA) has been shown to be beneficial in older adults with osteoarthritis (OA), most show low levels of PA. This study evaluated if self-efficacy, attitude, social norm, and coping styles predicted change in PA in older adults with OA in the knee and/or hip.
Methods
Prospective study following 105 participants in a self-management intervention with baseline, post-test (6 weeks), and follow-up (6 months). Univariate associations and multivariate regression with self-reported change in PA as the dependent variable were measured. Potential predictors in the model: demographic, illness-related, and behavioral variables (attitude, self-efficacy, social norm, and intention), coping style, and pain coping.
Results
Forty-eight percent of participants reported increased PA at 6 weeks and 37% at 6 months which corresponded with registered PA levels. At 6 weeks, use of the pain coping style “resting,” intention, and participation in the intervention was univariately and multivariately, positively associated with more self-reported change, whereas being single and less use of the pain coping style “distraction” predicted less change. Higher pain severity only predicted less change multivariately. At 6 months, univariate associations for age, general coping style “seeking support,” and participation in the intervention were found; higher age was associated multivariately with less self-reported change.
Conclusion
At short term, self-reported change of PA was predicted by the behavioral factors intention and several pain coping styles. Together with other predictors of self-reported change (pain severity, higher age, being single), these could be addressed in future interventions for enhancing PA in older adults with OA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoarthritis (OA) is the most common form of arthritis, with knee and hip joints affected most. OA leads to pain, tenderness, swelling, and decreased function of weight-bearing joints which in turn could lead to disability [1].
As there is no direct cure for OA, the prevention and management of its consequences are important. One of the most widely known and recommended non-pharmacological methods for the effective management of OA is physical activity (PA) [2]. Any movement of your body requiring energy is considered physical activity. Exercise (a subcategory of PA as it is usually structured and planned PA) helps regain muscular condition, balance, and joint stability [3] which improves physical functioning and general well-being and reduces pain [4]. Regular daily PA has preventive and therapeutic effects [5], while avoidance of activity predicts an increase of limitations in patients with knee OA [6]. Walking has also been found to be equally effective in managing knee OA as has home-based quadriceps exercise training [7]. In knee OA, obesity is one of the modifiable risk factors that also can be targeted by PA, preferably combined with dietary interventions [8].
Despite these positive findings, older adults with OA show low levels of maintaining exercise and low compliance with PA guidelines [9]. Greater adherence to recommended exercise programs predicts long-term benefits [7, 10]. More insight into which factors determine PA behavior in older adults with OA can contribute to more effective intervention strategies to increase quality of life and prevent dependency in older adults [11]. Several studies have found that socio-demographic (e.g., lower age, male gender, and higher education), health (e.g., normal weight, no physical limitations, pain, or fatigue), and healthcare factors (i.e., having been advised by a health professional that PA benefits osteoarthritis) are associated with increased levels of PA [12,13,14].
Individual behavioral aspects such as self-efficacy (an individual’s belief in his or her capacity to execute behaviors), attitude, and pain-coping strategies are all considered possible determinants of PA behavior and thereby on the impact of OA on physical performance and disability [15,16,17,18,19].
More insight into how these factors interact with each other and predict actual PA behavioral change in older adults with chronic conditions is needed. The answer still remains a gap in knowledge and could be of importance for designing future more effective interventions. A longer version of this manuscript has been published in the PhD dissertation of the first author [20].
Methods
Study Design
Data of 105 participants of an earlier randomized controlled trial (RCT) of a self-management program for patients with OA of the knee and or hip were used [21]. Potential participants were recruited through advertisements in a local newspaper. Inclusion criteria were OA of the hip and/or knee diagnosed by radiographic and clinical criteria, age between 55 and 75 years, and not being on a waiting list for joint replacement.
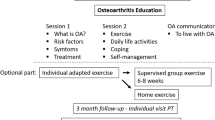
The intervention program consisted of 6 weekly sessions of 2 h health education by a peer and physical exercises taught by a physical therapist (for details, see Textbox 1). Data were collected by questionnaires, interviews, and physical examination at baseline, at 6 weeks, and at 6-months follow-up. A more detailed study design is described elsewhere [21]. The study protocol was approved by the TNO Medical Ethics Committee. All the participants gave informed consent to the study and human rights were respected.
In order to study factors that determine PA behavior, participants from the earlier RCT were analyzed as one group, controlling for participation in the intervention.
Data Collection
To measure changes in PA behavior (the outcome variable), participants were asked: “Has OA caused you to exerciseFootnote 2 more or less over the past 6 weeks/6 months?” Answers were given on a 5-point Likert scale ranging from “much more” to “much less” PA behavior and was dichotomized into more PA at 6 weeks versus the same amount or less PA (model 1), and more PA in the past 6 months versus the same level or less PA (model 2). In two participants, answers on PA behavior outcomes were missing, leaving 103 participants included in the analysis.
To additionally assess PA levels for comparison, the Voorrips questionnaire was conducted by an interviewer at baseline and at 6 months [22]. The reliability (0.89) and validity (0.78) of the questionnaire are good. Respondents were asked to report habitual physical activities over the past (half) year. Questions cover three areas: household activities (mean score of 10 items ranging from “very active” to “inactive”), sport activities (type of activity, intensity, hours per week, and months per year, for a maximum of two activities), and leisure time activities (type of activity, intensity, hours per week and months per year, for six activities maximum). Sport and leisure activity scores were calculated by an equation multiplying the intensity, hours per week and period of the year. The PA levels are reported with mean and SD of continuous data. If tertiles were used this resulted in a total PA score according to which participants were finally classified as having a high, medium, or low level of PA.
The baseline variables age, sex, marital status, education, income, and work status (paid or voluntary work) were identified as demographic variables. There were five categories of marital status: married living together, not married living together, divorced, widowed, and single. Education was divided into three categories following the Dutch educational system: primary education (0–8 years), secondary education (9–16 years), and college/university (17 years and older). Income was classified into categories low, middle, and high income levels in euros (< €908; €908–€1360; > €1360). All participants were white European people.
Duration of joint complaints was assessed by asking “how many years ago did your first OA complaints arise?” Answer categories were < 1 year, 1–3 years, 3–10 years, 10–20 years,” and > 20 years ago. Self-reported joint complaints (right or left hip, right or left knee) were noted by participants if present.
Body mass index (BMI) was calculated as length and weight expressed as kilograms per square meter. Participants were classified as normal weight (BMI < 25), overweight (BMI 25–30), and obese (BMI ≥ 30). Comorbidity, including use of medication, was assessed during the interview by reading out a list of 25 chronic conditions to the participants and asking them if they had any of these disorders and, if so, what sort of medication they took for it. Pain severity, pain tolerance, and fatigue over the previous month were measured on a 10-cm VAS scale ranging from 0 to 100. A higher score indicates more pain/fatigue. Disability was evaluated using the Sickness Impact Profile (SIP) subscale physical functioning which comprises self-reported statements on ability to carry out activities in the area of household management, body care, and movement and mobility. Scores are summarized and presented as a percentage of maximum dysfunction, ranging from 0 to 100%. The higher the score, the higher the level of disability [23].
Behavioral variables were based on the theoretical model of attitude, social norm, and self-efficacy (ASE) of de Vries [24]. The ASE model illustrates how factors contribute to intention to display a desired behavior. Attitude comprised two constructs: the expectations of consequences of certain behavior (e.g., beliefs) and the value given to those expectations (e.g., evaluations). Regarding beliefs, the participant was given a list of six activities and asked “how much benefit do you think the following activities will have on your functioning in general?” The answering scales were “a lot of benefit,” “a little benefit,” and “no benefit.” The same six questions were asked on evaluations; “how important do you feel these benefits are to the following activities” with answering scales “important,” “a little bit important,” and “not important.” Where one item was missing, participants (n = 21) were given the statistical mean value. If more than one item was missing per construct, cases were excluded from analysis (n = 19). A sum score of attitude to PA was calculated by multiplying the beliefs and evaluations of each question per respondent, followed by adding up the scores of the six questions [25]. A higher score indicated a more positive attitude.
Social norm was operationalized as the perceived opinion of important others (e.g., normative beliefs) and the personal value given to these opinions (e.g., motivation to comply). Normative beliefs were assessed by asking “how do you think your near environment would react if you were to undertake more PA?” with answers “positive, negative or neutral.” The motivation to comply was measured by asking “how important is the opinion of your near environment” on a 5-point answer scale “very important” to “not important.” A social norm score was calculated by multiplying the normative beliefs of each participant with their motivation to comply [25]. A higher score indicates a more positive social norm.
Self-efficacy is one’s belief in being able to carry out a certain behavior. Self-efficacy was measured by asking “do you believe you will succeed in exercising more?” on a 10-cm VAS scale, with a higher score indicating “no, I will not succeed.” This scale was developed by Lorig and Holman [26] to measure perceived self-efficacy in patients with rheumatic disease.
Finally, intention was measured by asking “do you intend to engage in more PA?” Answers “definitely yes,” “probably yes,” “probably no,” and “definitely no” were dichotomized into 1 = yes and 0 = no.
Coping styles in general were assessed at baseline by the short version of the Utrecht Coping List (UCL) which views coping as a personality trait and measures how people deal with health and illness in general. Seventeen items were evaluated by respondents by reporting the frequency of responding to a given problem on a four-point scale from “never” to “very often.” Items were divided into four categories: active problem solving (5 items, such as “seeking ways to solve the problem”), seeking support (5 items, e.g., “asking someone for help”), avoidance (5 items, e.g., “doing other things to avoid thinking about the problem”), and a religious response (2 items, “praying” and “thinking the situation is inevitable because it comes from a higher power”). A higher score indicated more use of the coping style. The short version of the UCL has been found to be valid and reliable [27].
The Pain Coping Inventory (PCI) is a Dutch pain-specific coping instrument developed by Kraaimaat and van Schevikhoven [28]. The PCI assesses how people deal with pain. A four-point answering scale was used to identify how often a certain behavior is carried out (“never” to “very often”). The 35 items were categorized into six pain coping scales: worrying about pain (“I think the pain will get worse”), distraction by engaging in pleasant activities (e.g., “I seek distraction by diverting my attention to reading, music, watching television, or something similar”), resting (e.g., “I restrict myself to simple activities”), pain transformation (e.g., “I imagine the pain to be less severe than it really is”), retreating (e.g., “I ensure I will not be disturbed by intrusive noise”), and reducing demands (e.g., “I make sure I do not get anxious”). A higher score indicated more use of a pain coping style.
Participation in the intervention program and baseline PA (continuous score as calculated by the Voorrips questionnaire) were included as confounders.
Analysis
Descriptive statistics of all participants on baseline characteristics were calculated. Results for self-reported change in PA behavior and PA levels at 6 months are compared to see if participants’ reports correspond.
To study which factors predicted self-reported change in PA behavior at 6 weeks and at 6 months, univariate comparisons were made between possible predictors and the two models using chi-square tests for categorical variables and t tests for continuous variables. All participants were categorized as either carrying out less or the same PA or more PA. In the first step of the (explorative) analysis, all study variables were entered. These variables have been chosen based on the short literature review described in the introduction. Univariate associations of p < 0.20 (see Table 3 in the “Results” section) were required for entry into the multivariate model with the exception of pain severity which was added to the multivariate model due to its great impact on patients suffering from OA [29, 30].
In the second step of the analysis, multivariate stepwise backward logistic regression analyses were first conducted between independent predictors and more PA behavior at 6 weeks (model 1) and at 6 months (model 2). Predictors were tested in five blocks of variables (Fig. 1); demographic variables were tested in block 1, followed by illness-related variables in block 2, behavior variables in block 3, pain coping styles and coping styles in general in block 4, and confounders in block 5. Confounders were entered into the last step of the model to reduce its effects on other variables. Intention was entered as an extra step after attitude to prevent obscuring the multivariate model, as the ASE model shows that attitude influences intention.
In analyzing the two models, changes in ß, p values, and Nagelkerke R2 were calculated. Hosmer and Lemeshow’s goodness-of-fit tests were conducted to assess if non-significant chi-square goodness-of-fit value was present. Correlations between predictors were assessed to test for multicollinearity. Correlations higher than 0.50 were excluded to ensure stable regression analyses. Finally, missing analyses were conducted using chi-square tests and t tests to assess if excluded participants were similar to valid participants on demographic variables age, sex, marital status, education, income, and illness-related variable body mass index.
To check whether the results for self-reported change could be replicated for PA levels as measured with the Voorrips questionnaire at 6 months, possible predictors of these were tested with the same procedure. P values less than 0.05 were considered statistically significant. Statistical analyses were performed using SPSS.
Results
Baseline characteristics of the total study population (n = 105; Table 1) showed that most participants were women, married and living together, and overweight or obese and had completed secondary or higher education. Around one-third were engaged in paid work or voluntary work. Of participants reporting other chronic diseases, OA of the hands, severe back complaints, and high blood pressure were most frequently reported. Almost all participants reported complaints in knee and/or hip joints, with 30% reporting complaints in three or four joints. Knee complaints were twice more prevalent than hip complaints. Radiological OA (ROA) of the knee was two to three times more prevalent than hip ROA. Disability in the domain of physical functioning was low, with participants indicating only 6% maximum dysfunction.
Around 48% of respondents reported they had become more physically active after 6 weeks compared with baseline, 45% remained stable, and 8% reported less PA (Table 2). At follow-up, 6 months later, 38% reported that they had increased their PA behavior on comparison with baseline. A large proportion of all participants who reported more PA at 6 weeks also reported more PA at 6 months (n = 28, 58%) or maintained the level (n = 19, 40%). A few participants were doing less at 6 months than at 6 weeks (n = 11). To assess the correspondence between self-reported change in PA behavior and self-reported PA levels using the Voorrips questionnaire, Table 2 shows the mean change in PA level per change group at 6 months. Although only the “more” group reported a rise in PA levels, compared to a minor decline for the “same” and “less” group, there was no statistically significant difference in mean change between the three groups (F = 2.6; p = 0.078).
Univariate associations between baseline characteristics and PA behavior are presented in Table 3.
Predictors of Change in PA at 6 Weeks
The following variables were entered into the multivariate analysis based on associations with more PA behavior measured at 6 weeks: marital status, BMI, intention, general coping style “active problem solving,” pain coping styles, “pain transformation,” “distraction,” “retreating,” and “resting,” intervention status, baseline PA levels, and pain severity.
In the last step of the multivariate regression analysis (Table 4), intention, use of the pain coping style “resting,” and participation in the intervention were positively associated with more PA behavior whereas being single, having more severe pain, and making less use of the pain coping style “distraction” contributed to lower levels of PA behavior. Intention was the best predictor of change in PA behavior, followed closely by being single. The predictors explained 59% of the variance of more PA behavior. Demographic variables explained most of the variance together with intention and pain coping styles. No significant chi-square goodness-of-fit values were detected, and no multicollinearity was present. Missing analysis showed there were no significant differences between missing and valid subjects on demographic variables and BMI.
Predictors of Change in PA at 6 Months
Variables univariately associated with change in PA behavior at 6 months that were selected for multivariate analysis were sex, income, paid and voluntary work, age, BMI, comorbidity, attitude, intention, general coping style “seeking support,” pain coping styles “reducing demands” and “resting,” intervention status, and PA level at baseline. Again, pain severity was added.
Multivariate analysis showed that age was the only significant predictor (n = 64; ß = −0.14; p = 0.02) of more PA behavior at 6 months and explained 40% of the variance (data not shown). In the model, higher age was associated with less PA behavior. Missing analysis showed that valid participants had higher income levels (p = 0.02) than those with missing data. No multicollinearity was present.
Self-reported PA levels (using the Voorrips questionnaire) categorized into high, medium, and low tertiles showed univariate associations with age, paid work activities, attitude, intention, general coping style “active problem solving,” baseline PA, and intervention status (data not shown). Stepwise backward logistic regression analysis showed age was the only significant predictor (n = 70; ß = −0.13; p = 0.01). Again, higher age was associated with lower levels of PA behavior. The results from the two models are summarized in Table 5.
Discussion
This study explored predictors of self-reported change in PA among older adults with radiologic and clinical confirmed knee or hip OA. Six weeks after baseline, the predictors accounted for 59% of the variance in the outcome variable, and after 6 months, this was 40%. Compared with baseline, almost half of the participants indicated that they had increased their PA behavior at 6 weeks, and by 6 months, this was 37%. This finding is consistent with other studies, as the effect of change in behavior is difficult to maintain over time [31]. Even so, only a small percentage (10%) indicated that they had reduced their PA.
Of the behavioral aspect of the ASE model, only the intention to become more physically active item predicted becoming more physically active at 6 weeks, although the variables influencing intention, i.e., attitude, self-efficacy, and social norm, were not associated. This result is contrasted to other studies which show that self-efficacy in particular plays a role in PA [18, 32]. This could be due to the relatively small groups in our study and the fact that the intervention and control groups were analyzed together. Self-efficacy was in fact one of the significant results in the RCT [21], and we treated the intervention as a confounder in the analyses.
Although an intention-behavior gap does exist, intention, however, is still known as one of the best predictors of PA [33].
Results on the pain coping styles “resting” and “distraction” seem to contradict other studies that used the same instrument (PCI), where active pain coping styles such as distraction were found to be cross-sectionally associated with more sporting activity, and passive coping styles such as resting with less sporting activity [15]. The use of the pain coping style “resting” also has been shown to be a predictor of future limitations in patients with knee and hip OA [6]. These studies used OA patients recruited through rehabilitation centers which might mean more pain and subsequent limitations in their study sample. Patients might use different coping strategies when faced with more serious symptoms.
Given the fact that pain severity also predicted PA at 6 months, the association with pain coping becomes more relevant. The interaction between these aspects makes the relationship between OA and PA complex. On the one hand strenuous occupational tasks and high-intensity competitive sports are risk factors for OA of the hand, hip, and knee [34, 35], while longitudinal studies in older adults with knee or hip osteoarthritis show that higher PA levels have been associated with a slower decline in function [5]. Examining how coping mechanisms play a role and using this information might help individuals to gain better control of the disease symptoms that influence PA and the pathway to disability [36].
In our sample, being single and having more severe pain were also associated with less PA behavior at 6 weeks. Both factors are well known to negatively influence PA behavior [13, 14, 30].
At 6 months, the behavioral aspects showed only univariate associations with self-reported behavioral change and PA levels. When controlled for other demographic and health-related predictors, no relationship with behavioral aspects was found. Only higher age predicted less PA at 6 months. This outcome confirms other studies that have reported higher age being associated with less PA behavior [13]. Nevertheless, it is striking that only one predictor remained to explain change in PA behavior as well as self-reported PA levels. From univariate results, it can be seen that the more physically active group is on average 3 years younger, which is quite a large gap in an age range of 20 years. In this group also, twice as many participants were active in paid or voluntary work which contributes to higher baseline PA levels [37] which could make it difficult to further increase PA levels in this group. Alternatively, age may stand for other variables that change with age but were not included in our set of predictors, or were not sufficiently specified, i.e., the variable for chronic disease which did not specify type of disease.
Other well-known predictors of change in PA identified in the literature such as BMI, number of chronic diseases, and disability [38, 39] were in our study not significantly related to self-reported change in activity behavior. Differences between study populations could explain this discrepancy. The high variance explained by our multivariate model might indicate that enough important variables were included for our study population. Because peer education was an important part of the intervention (see Textbox 1), it is plausible that all predictors of intention (attitude, self-efficacy, and social norms in the ASE model) were positively influenced leading to a strong intention for changing behavior in PA. Indeed, we found in the earlier RCT [21] a moderate effect of the intervention on self-efficacy.
Limitations of This Study
Certain limitations of this study should be considered. An important limitation of this study was the small study population, which decreased the statistical power meaning that long-term multivariate associations of self-reported change in PA behavior could not be assessed. Even so, no multicollinearity was present and the models showed good fit. Identified univariate predictors should give a good indication of the variables to be used in other studies.
Another limitation is self-reported behavior, which may be unreliable in assessing change in behavior. Socially desirable answers could be given. In addition, levels of PA tend to be overestimated [40]. Comparison with PA levels as measured with a validated questionnaire [22] in our study showed that subjective changes corresponded quite well with reported PA levels. Also, similar results were shown for predictors of 6 months PA between the self-reported change and levels outcome.
Despite these limitations, univariate and multivariate findings of this study should be considered or taken into account for future interventions. Higher age in particular was shown to be a high risk for lower PA behavior. Similar to other studies, the ASE model and others can be recommended to provide a background for interventions [41, 42], or at least behavior-guided interventions [31, 43].
It can be safely stated that these and other results show that the relationship between OA and PA is complicated and needs further study [44,45,46]. The interplay in time between the disease and its symptoms, functional limitations, and psychological reactions such as coping styles is complex and if left unattended may lead to a downward spiral of avoidance, fear of activity, and subsequent deterioration in function and disability [47, 48].
Conclusion
In conclusion, a change in PA behavior in the short term was found to be related to behavioral factors especially intention and also pain coping styles. This, together with the other predictors of self-reported change, in particular pain severity and marital status, should be addressed in designing more effective future interventions. The intervention that we used could be a good starting point for reaching that goal.
Notes
Petty BJ, Cusack SA. Assessing the impact of a seniors' peer counseling program. Educ Gerontol 1998;15:49–64.
In Dutch, the word lichaamsbeweging was used. This includes besides exercising also other physical activities such as walking, biking, doing household activities, etc.
References
Felson DT, Lawrence RC, Dieppe PA, Hirsch R, Helmick CG, Jordan JM, et al. Osteoarthritis: new insights. Part 1: the disease and its risk factors. Ann Intern Med. 2000;133(8):635–46.
Recommendations for the medical management of osteoarthritis of the hip and knee: 2000 update. American College of Rheumatology Subcommittee on Osteoarthritis Guidelines. Arthritis Rheum. 2000;43(9):1905–15.
Fransen M, McConnell S, Harmer AR, Van der Esch M, Simic M, Bennell KL. Exercise for osteoarthritis of the knee. Cochrane Database Syst Rev. 2015;1:CD004376.
Devos-Comby L, Cronan T, Roesch SC. Do exercise and self-management interventions benefit patients with osteoarthritis of the knee? A metaanalytic review J Rheumatol. 2006;33(4):744–56.
Dunlop DD, Semanik P, Song J, Sharma L, Nevitt M, Jackson R, et al. Moving to maintain function in knee osteoarthritis: evidence from the osteoarthritis initiative. Arch Phys Med Rehabil. 2010;91(5):714–21.
Pisters MF, Veenhof C, van Dijk GM, Heymans MW, Twisk JW, Dekker J. The course of limitations in activities over 5 years in patients with knee and hip osteoarthritis with moderate functional limitations: risk factors for future functional decline. Osteoarthritis Cartilage. 2012;20(6):503–10.
Pisters MF, Veenhof C, de Bakker DH, Schellevis FG, Dekker J. Behavioural graded activity results in better exercise adherence and more physical activity than usual care in people with osteoarthritis: a cluster-randomised trial. J Physiother. 2010;56(1):41–7.
Sevick MA, Miller GD, Loeser RF, Williamson JD, Messier SP. Cost-effectiveness of exercise and diet in overweight and obese adults with knee osteoarthritis. Med Sci Sports Exerc. 2009;41(6):1167–74.
Dunlop DD, Song J, Semanik PA, Chang RW, Sharma L, Bathon JM, et al. Objective physical activity measurement in the osteoarthritis initiative: are guidelines being met? Arthritis Rheum. 2011;63(11):3372–82.
Dunlop DD, Song J, Semanik PA, Sharma L, Chang RW. Physical activity levels and functional performance in the osteoarthritis initiative: a graded relationship. Arthritis Rheum. 2011;63(1):127–36.
Stevenson JD, Roach R. The benefits and barriers to physical activity and lifestyle interventions for osteoarthritis affecting the adult knee. J Orthop Surg Res. 2012;7:15.
Rosemann T, Kuehlein T, Laux G, Szecsenyi J. Factors associated with physical activity of patients with osteoarthritis of the lower limb. J Eval Clin Pract. 2008;14(2):288–93.
Fontaine KR, Haaz S. Risk factors for lack of recent exercise in adults with self-reported, professionally diagnosed arthritis. J Clin Rheumatol. 2006;12(2):66–9.
Kaplan MS, Huguet N, Newsom JT, McFarland BH. Characteristics of physically inactive older adults with arthritis: results of a population-based study. Prev Med. 2003;37(1):61–7.
Perrot S, Poiraudeau S, Kabir M, Bertin P, Sichere P, Serrie A, et al. Active or passive pain coping strategies in hip and knee osteoarthritis? Results of a national survey of 4,719 patients in a primary care setting. Arthritis Rheum. 2008;59(11):1555–62.
Rapp SR, Rejeski WJ, Miller ME. Physical function among older adults with knee pain: the role of pain coping skills. Arthritis Care Res. 2000;13(5):270–9.
Holla JF, Steultjens MP, Roorda LD, Heymans MW, Ten Wolde S, Dekker J. Prognostic factors for the two-year course of activity limitations in early osteoarthritis of the hip and/or knee. Arthritis Care Res (Hoboken). 2010;62(10):1415–25.
Maly MR, Costigan PA, Olney SJ. Self-efficacy mediates walking performance in older adults with knee osteoarthritis. J Gerontol A Biol Sci Med Sci. 2007;62(10):1142–6.
White DK, Keysor JJ, Neogi T, Felson DT, LaValley M, Gross KD, et al. When it hurts, a positive attitude may help: association of positive affect with daily walking in knee osteoarthritis. Results from a multicenter longitudinal cohort study. Arthritis Care Res (Hoboken). 2012;64(9):1312–9.
Tak ECPM. Reducing the impact of geriatric conditions by physical activity. Amsterdam: Vrije Universiteit. 2013.
Hopman-Rock M, Westhoff MH. The effects of a health educational and exercise program for older adults with osteoarthritis for the hip or knee. J Rheumatol. 2000;27(8):1947–54.
Voorrips LE, Ravelli AC, Dongelmans PC, Deurenberg P, Van Staveren WA. A physical activity questionnaire for the elderly. Med Sci Sports Exerc. 1991;23(8):974–9.
Bergner M, Bobbitt RA, Carter WB, Gilson BS. The Sickness Impact Profile: development and final revision of a health status measure. Med Care. 1981;19(8):787–805.
de Vries H. Self-efficacy: the third factor besides attitude and subjective norm as a predictor of behavioral intentions. In: Dijkstra M, editor. Health Educ Res 1988:273–82.
Damoiseaux V. Gezondheidsvoorlichting en gedragsverandering [health promotion and behavior change]. In: Van der Molen H, editor. Assen: van Gorcum; 1998.
Lorig K, Holman H. Arthritis self-management studies: a twelve-year review. Health Educ Q. 1993;20(1):17–28.
Komproe I. Social support for elderly women with cancer: helpful or harmful? In: Rijken P, editor. Utrecht: Utrecht university; 1995.
Kraaimaat FW, van Schevikhoven RE. Causal attributions and coping with pain in chronic headache sufferers. J Behav Med. 1988;11(3):293–302.
Hopman-Rock M, Kraaimaat FW, Odding E, Bijlsma JW. Coping with pain in the hip or knee in relation to physical disability in community-living elderly people. Arthritis Care Res. 1998;11(4):243–52.
Rejeski WJ, Ettinger WH, Martin K, Morgan T. Treating disability in knee osteoarthritis with exercise therapy: a central role for self-efficacy and pain. Arthritis Care Res. 1998;11(2):94–101.
Gay C, Chabaud A, Guilley E, Coudeyre E. Educating patients about the benefits of physical activity and exercise for their hip and knee osteoarthritis. Systematic literature review. Ann Phys Rehabil Med. 2016;59(3):174–83.
Berry A, McCabe CS, Halls S, Muir S, Walsh N. Beliefs, motives and gains associated with physical activity in people with osteoarthritis. Musculoskeletal Care. 2021;19(1):52–8.
Rhodes RE, Cox A, Sayar R. What predicts the physical activity intention-behavior gap? A systematic review Ann Behav Med. 2022;56(1):1–20.
Szoeke CEI, Cicuttini FM, Guthrie JR, Clark MS, Dennerstein L. Factors affecting the prevalence of osteoarthritis in healthy middle-aged women: data from the longitudinal Melbourne Women’s Midlife Health Project. Bone. 2006;39(5):1149–55.
Verweij LM, van Schoor NM, Deeg DJ, Dekker J, Visser M. Physical activity and incident clinical knee osteoarthritis in older adults. Arthritis Rheum. 2009;61(2):152–7.
Stewart AL. Conceptual challenges in linking physical activity and disability research. Am J Prev Med. 2003;25(3 Suppl 2):137–40.
Slingerland AS, van Lenthe FJ, Jukema JW, Kamphuis CB, Looman C, Giskes K, et al. Aging, retirement, and changes in physical activity: prospective cohort findings from the GLOBE study. Am J Epidemiol. 2007;165(12):1356–63.
Dunlop DD, Semanik P, Song J, Manheim LM, Shih V, Chang RW. Risk factors for functional decline in older adults with arthritis. Arthritis Rheum. 2005;52(4):1274–82.
Sharma L, Cahue S, Song J, Hayes K, Pai YC, Dunlop D. Physical functioning over three years in knee osteoarthritis: role of psychosocial, local mechanical, and neuromuscular factors. Arthritis Rheum. 2003;48(12):3359–70.
Klesges RC, Eck LH, Mellon MW, Fulliton W, Somes GW, Hanson CL. The accuracy of self-reports of physical activity. Med Sci Sports Exerc. 1990;22(5):690–7.
van der Ploeg HP, van der Beek AJ, van der Woude LH, van Mechelen W. Physical activity for people with a disability: a conceptual model. Sports Med. 2004;34(10):639–49.
Kanavaki AM, Rushton A, Efstathiou N, Alrushud A, Klocke R, Abhishek A, et al. Barriers and facilitators of physical activity in knee and hip osteoarthritis: a systematic review of qualitative evidence. BMJ Open. 2017;7(12):e017042.
Conn VS, Hafdahl AR, Brown SA, Brown LM. Meta-analysis of patient education interventions to increase physical activity among chronically ill adults. Patient Educ Couns. 2008;70(2):157–72.
Veenhof C, Huisman PA, Barten JA, Takken T, Pisters MF. Factors associated with physical activity in patients with osteoarthritis of the hip or knee: a systematic review. Osteoarthritis Cartilage. 2012;20(1):6–12.
Stubbs B, Hurley M, Smith T. What are the factors that influence physical activity participation in adults with knee and hip osteoarthritis? A systematic review of physical activity correlates. Clin Rehabil. 2015;29(1):80–94.
Dobson F, Bennell KL, French SD, Nicolson PJ, Klaasman RN, Holden MA, et al. Barriers and facilitators to exercise participation in people with hip and/or knee osteoarthritis: synthesis of the literature using behavior change theory. Am J Phys Med Rehabil. 2016;95(5):372–89.
Dekker J, Tola P, Aufdemkampe G, Winckers M. Negative affect, pain and disability in osteoarthritis patients: the mediating role of muscle weakness. Behav Res Ther. 1993;31(2):203–6.
Steultjens MP, Dekker J, Bijlsma JW. Avoidance of activity and disability in patients with osteoarthritis of the knee: the mediating role of muscle strength. Arthritis Rheum. 2002;46(7):1784–8.
Funding
This work is funded by the Netherlands Organization for Health Research and Development (220000120).
Author information
Authors and Affiliations
Contributions
All the authors (ET, LV, AC and MH) contributed substantially in the concept, design and writing of this paper. Data-analyses have been done by LV.
Corresponding author
Ethics declarations
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standard.
Informed Consent
Informed consent was obtained from all individual participants in the study.
Conflict of Interests
The authors declare that they have no financial or competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This work is also affiliated with the former TNO Prevention and Health, Department of Physical Activity and Health.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tak, E.C.P.M., Verweij, L.M., Chorus, A.M.J. et al. What Are the Predictors of Self-Reported Change in Physical Activity in Older Adults with Knee or Hip Osteoarthritis?. Int.J. Behav. Med. 30, 199–210 (2023). https://doi.org/10.1007/s12529-022-10080-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12529-022-10080-y