Abstract
Background
In the era of HIV treatment as prevention, little research has focused on the fertility behaviour of men living with HIV. This study examines the predictors and motivators of fertility among men living with HIV and on antiretroviral treatment in Kano, Nigeria.
Method
Using mixed methods, structured questionnaires were administered to a clinic-based sample of men living with HIV (n = 270) and HIV-negative/untested controls (n = 270), followed by in-depth interviews with a sub-group of 22 HIV-positive participants. Logistic regression and the framework approach were used to analyse the data.
Results
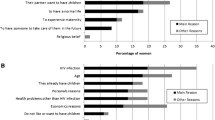
Compared to HIV-negative/untested controls, lower proportions of men living with HIV desired more children (79.3%, n = 214 vs. 91.1%, n = 246, p < 0.05) and intended to bear children within 3 years (57.0%, n = 154 vs. 67.0%, n = 181) (p < 0.05). Marital status (ever married vs. single) predicted fertility intention among men living with HIV (adjusted odds ratio, AOR = 4.70, 95% confidence interval CI, 1.75–13.64) and HIV-negative/untested controls (AOR = 4.23, 95% CI, 1.37–16.45). Men considered self and partner health status, HIV transmission risks, poverty, the effectiveness of interventions, child survival and religion when making fertility decisions.
Conclusion
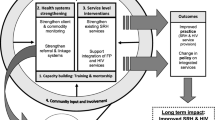
Fertility desires remain high post-HIV diagnosis. HIV services should include integrated reproductive health programs that address the fertility desires of clients and include considerations for fertility services.

Similar content being viewed by others
References
UNAIDS. UNAIDS Data 2019. https://www.unaids.org/sites/default/files/media_asset/2019-UNAIDS-data_en.pdf Last accessed 21st September 2019.
UNAIDS. New survey results indicate that Nigeria has an HIV prevalence of 1·4%. http://www.unaids.org/en/resources/presscentre/pressreleaseandstatementarchive/2019/march/20190314_nigeria Last accessed 21st September 2019.
Bogart LM, Collins RL, Kanouse DE, Cunningham W, Beckman R. Patterns and correlates of deliberate abstinence among men and women with HIV/AIDS. Am J Public Health. 2006;96(6):1078–84.
Ortiz MR. HIV, AIDS, and sexuality. Nurs Clin North Am. 2007;42(4):639–53.
Oguntibeju OO. Quality of life of people living with HIV and AIDS and antiretroviral therapy. HIV AIDS (Auckl). 2012;4:117–24.
Lemoine C, Willems N, Alain DH, Karama R, Somda I, Englert Y. Women's desire for children in an HIV population: a clinical pilot study in Burkina Faso. Curr HIV Res. 2011;9(5):346–51.
Cooper D, Moodley J, Zweigenthal V, Bekker LG, Shah I, Myer L. Fertility intentions and reproductive health care needs of people living with HIV in Cape Town, South Africa: implications for integrating reproductive health and HIV care services. AIDS Behav. 2009;13(Suppl 1):38–46.
Sheree R, Schwartz JB, Sanne I, Phofa R, Yende N, Van Rie A. Implementation of a safer conception service for HIV-affected couples in South Africa. AIDS. 2014;28(Suppl 3):S277–85.
Iliyasu Z, Abubakar IS, Kabir M, Babashani M, Shuaib F, Aliyu MH. Correlates of fertility intentions among HIV/AIDS patients in northern Nigeria. Afr J Reprod Health. 2009;13(3):71–83.
Creswell JW, Plano Clark VL. Designing and conducting mixed methods research. 2nd ed. Thousand Oaks: Sage; 2011. p. 43–51.
Iliyasu Z, Babashani M. Prevalence and predictors of tuberculosis coinfection among HIV-seropositive patients attending the Aminu Kano Teaching Hospital, northern Nigeria. J Epidemiol. 2009;19:81–7.
Magnani R. Sampling guide. IMPACT Food Security and Nutrition Monitoring Project. 1997:13–7.
National Population Commission, Nigeria Demographic and Health Survey (NDHS). NPC and ICF international, Abuja. Nigeria. 2008;2009.
Wekesa E, Coast E. Fertility desires among men and women living with HIV/AIDS in Nairobi slums: a mixed methods study. PLoS One. 2014;9(8):e106292.
Wagner GJ, Wanyenze R. Fertility desires and intentions and the relationship to consistent condom use and provider communication regarding childbearing among HIV clients in Uganda. ISRN Infect Dis. 2013.
Miller WB. Childbearing motivations, desires, and intentions: a theoretical framework. Genet Soc Gen Psychol Monogr. 1994;120(2):223–58.
National Heart Foundation and Faculty of Public Health and Department of Health, 2007. Lightening the load: tackling overweight and obesity: a toolkit for developing local strategies to tackle overweight and obesity in children and adults. [Online] London: Department of Health. Available at: http://www.dh.gov.uk/en/Publicationsandstatistics/ Publications/PublicationsPolicyAndGuidance/DH_073936 [Accessed March 2019].
Crankshaw TL, Matthews LT, Giddy J, Kaida A, Ware NC, Smit JA, et al. A conceptual framework for understanding HIV risk behavior in the context of supporting fertility goals among HIV-serodiscordant couples. Reprod Health Matters. 2012;20(39 Suppl):50–60.
IBM Corporation. IBM SPSS statistics for windows, Version 21.0, 2012.
Pope C, Ziebland S, Mays N. Qualitative research in health care. Analysing qualitative data. BMJ. 2000;320(7227):114–6.
Farmer T, Robinson K, Elliott SJ, John ED. Developing and implementing a triangulation protocol for qualitative health research. Qual Health Res. 2006;16:377.
National Population Commission, Nigeria Demographic and Health Survey (NDHS) 2013, NPC and ICF international, Abuja, Nigeria, 2014.
Apondi R, Bunnell R, Ekwaru JP, Moore D, Bechange S, Khana K, et al. Sexual behavior and HIV transmission risk of Ugandan adults taking antiretroviral therapy: 3 year follow-up. AIDS. 2011;25(10):1317–27.
Leggett H. Becoming a positive parent: reproductive options for people with HIV. BETA. 2011:43–8.
National Population Commission, Nigeria Demographic and Health Survey (NDHS). NPC and ORC macro. Abuja, Nigeria. 2003;2004:33–42.
Caldwell JC, Caldwell P. The cultural context of high fertility in sub-Saharan Africa. Popul Dev Rev. 1987;13(3):409–37.
Isiugo-abanihe UC. The socio-cultural context of high fertility among Igbo women. Int Sociol. 1994 Jun;9(2):237–58.
Cooper D, Harries J, Myer L, Omer P, Bracken H. Life is still going on: reproductive intentions among HIV positive women and men in South Africa. Soc Sci Med. 2007;65:274–83.
Adilo TM, Wordofa HM. Prevalence of fertility desire and its associated factors among 15- to 49-year-old people living with HIV/AIDS in Addis Ababa, Ethiopia: a cross-sectional study design. HIV AIDS (Auckl). 2017;9:167–76.
Nakayiwa S, Abang B, Packel L. Desire for children and pregnancy risk behavior among HIV-infected men and women in Uganda. AIDS Behav. 2006;10(4 Suppl):S95–104.
Khidir H, Psaros C, Greener L, et al. Developing a safer conception intervention for men living with HIV in South Africa. AIDS Behav. 2018;22:1725–35.
Dunlap J, Foderingham N, Bussell S, Wester CW, Audet CM, Aliyu MH. Male involvement for the prevention of mother-to-child HIV transmission: a brief review of initiatives in East, West and Central Africa. Curr HIV/AIDS Rep. 2014;11(2):109–18.
Sonnenberg P, Copas A, Glynn JR, Bester A, Nelson G, Shearer S, et al. The effect of HIV infection on time off work in a large cohort of gold miners with known dates of seroconversion. Occup Environ Med. 2011;68(9):647–52.
Smith DJ, Mbakwem BC. Antiretroviral therapy and reproductive life projects: mitigating the stigma of AIDS in Nigeria. Soc Sci Med. 2010;71(2):345–52.
Dessie Y, Gerbaba M, Bedru A, Davey G. Risky sexual practices and related factors among ART attendees in Addis Ababa public hospitals, Ethiopia: a cross-sectional study. BMC Public Health. 2011;11:422.
Myer L, Morroni C, Rebe K. Prevalence and determinants of fertility intentions of HIV-infected women and men receiving antiretroviral therapy in South Africa. AIDS Patient Care STDs. 2007;21(4):278–85.
Heys J, Kipp W, Jhangri G, Alibhai A, Rubaale T. Fertility desires and infection with the HIV: results from a survey in rural Uganda. AIDS. 2009;23:S37–45.
Kaida A, Laher F, Strathdee SA, Janssen PA, Money D, Hogg RS, et al. Childbearing intentions of HIV-positive women of reproductive age in Soweto, South Africa: the influence of expanding access to HAART in an HIV hyperendemic setting. Am J Public Health. 2011;101(2):350–8. https://doi.org/10.2105/AJPH.2009.177469.
Mantell JE, Exner TM, Cooper D. Pregnancy intent among a sample of recently diagnosed HIV-positive women and men practicing unprotected sex in Cape Town, South Africa. J Acquir Immune Defic Syndr. 2014;67(Suppl 4):S202–9.
Chen JL, Philips KA, Kanouse DE, Collins RL, Miu A. Fertility desires and intentions of HIV-positive men and women. Fam Plan Perspect. 2001;33(4):144–52.
Westoff CF, Bietsch K. Religion and reproductive behavior in Sub-Saharan Africa. DHS Analyt Stud. 2015;48:24–35.
Song X, Grilo SA, Mathur S, Lutalo T, Ssekubugu R, Nalugoda F, et al. Differential impacts of HIV status on short-term fertility desires among couples in Rakai, Uganda. PLoS ONE. 2019;14(1):e0210935.
Kriel Y, Milford C, Cordero J, Suleman F, Beksinska M, Steyn P, et al. Male partner influence on family planning and contraceptive use: perspectives from community members and healthcare providers in KwaZulu-Natal, South Africa. Reprod Health. 2019;16(1):89.
Cohen MS, McCauley M, Gamble TR. HIV treatment as prevention and HPTN 052. Curr Opin HIV AIDS. 2012;7(2):99–105.
Forsyth AD, Valdiserri RO. Reaping the prevention benefits of highly active antiretroviral treatment: policy implications of HIV Prevention Trials Network 052. Curr Opin HIV AIDS. 2012;7(2):111–6.
Mutisya R, Wambua J, Nyacahe P, Kamau M, Karnad SR, Kabue M. Strengthening integration of family planning with HIV/AIDS and other services: experience from three Kenyan cities. Reprod Health. 2019;16(Suppl 1):62.
Chillag K, Guest G, Bunce A, Johnson L, Kilmarx PH, Smith DK. Talking about sex in Botswana: social desirability bias and possible implications for HIV-prevention research. J AIDS HIV Res. 2006;5(2):123–31.
Manski CF. The use of intentions data to predict behavior: a best-case analysis. J Am Stat Assoc. 1990;85(412):934–40.
Acknowledgements
We thank our research assistants, Mr. Aliyu Mande and Dr. Musa Bello.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Ethical Statement
Ethical clearance was obtained from the ethics committees of Aminu Kano Teaching Hospital, Nigeria and the School of Health and Related Research at the University of Sheffield, UK. All participants provided written informed consent.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Iliyasu, Z., Owen, J., Aliyu, M.H. et al. “I prefer not to have a child than have a HIV-positive child”: a Mixed Methods Study of Fertility Behaviour of Men Living with HIV in Northern Nigeria. Int.J. Behav. Med. 27, 87–99 (2020). https://doi.org/10.1007/s12529-019-09837-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12529-019-09837-9