Abstract
Background
Updated seroprevalence estimates are important to describe the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) landscape and to guide public health decisions. The aims are to describe longitudinal changes in seroprevalence in children in a region in Northern Spain and to analyze factors associated with SARS-CoV-2 seropositivity.
Methods
Prospective multicenter longitudinal study with subjects recruited from July to September 2020. Children (up to 14 years old) were included and followed up until September 2021. Venous blood samples were collected every six months during three testing rounds and were analyzed for SARS-CoV-2 antibodies. The data regarding epidemiological features, contact tracing, symptoms, and virological tests were collected. The evolution of SARS-CoV-2 seroprevalence during the study and the differences between children with positive and negative SARS-CoV-2 antibody tests were analyzed.
Results
Two hundred children were recruited (50.5% girls, median age 9.7 years). The overall seroprevalence increased from round 1 [1.5%, 95% confidence interval (CI) 0.3%–4.3%] to round 2 (9.1%, 95% CI 4.6%–12.7%) and round 3 (16.6%, 95% CI 9.5%–19.6%) (P < 0.001). Main changes occurred in children aged zero to four years (P = 0.001) who lived in urban areas (P < 0.001). None of the children who were previously positive became seronegative. Following multivariable analysis, three variables independently associated with SARS-CoV-2 seropositivity were identified: close contact with coronavirus disease 2019 (COVID-19) confirmed or suspected cases [odds ratio (OR) = 3.9, 95% CI 1.2–12.5], previous positive virological test (OR = 17.1, 95% CI 3.7–78.3) and fatigue (OR = 18.1, 95% CI 1.7–193.4).
Conclusions
SARS-CoV-2 seroprevalence in children has remarkably increased during the time of our study. Fatigue was the only COVID-19-compatible symptom that was more frequent in seropositive than in seronegative children.
Similar content being viewed by others
Introduction
World Health Organization (WHO) declared coronavirus disease 2019 (COVID-19) a Public Health Emergency of International Concern (PHEIC) on January 30 [1] and as a global pandemic on March 11 owing to the rapid increase of COVID-19 cases spread throughout the world [2]. On January 31, Spain declared the first case of COVID-19 [3], and on February 29 the first case in Asturias was reported [4].
On March 14, 2020, a total lockdown was declared in Spain [5]. Most of the nonessential activities were forbidden. Citizens were still permitted to travel to work and to buy essential items. This state of alarm initially imposed for 14 days lasted until June 21 [6]. Schools and kindergartens were closed in Asturias from March 13 to September 22, 2020, opening after the summer holiday [7]. Some preventive measures were implemented, such as masks for school staff and children, restriction of large group activities, as well as contact tracing in schools [8].
In April 2020, the Spanish Ministry of Health and the Institute of Health Carlos III, in collaboration with the health services of the Spanish regions, launched ENE-COVID, a nationwide, population-based, longitudinal, seroepidemiological study to investigate seropositivity for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in the noninstitutionalized Spanish population. The study included more than 61,000 individuals from randomly selected households and three successive follow-up rounds of data collection from April to June 2020 [9]. The prevalence of SARS-CoV-2 antibodies for the entire country was between 5.0% and 5.2% during the three rounds of the study. Estimates varied markedly across provinces. In the central part of Spain, including Castilla La Mancha and Madrid, the seroprevalence was around 10%, whereas in Asturias, it was 1.9%, 1.6%, and 1.9% in the three rounds of the study [10].
In the first wave, the seroprevalence in Spain was lower in children, especially in infants younger than one year: 1.1%, 2.1%, 3.1%, and 4% for the following age groups: < 1 year, 1–4 years, 5–9 years, and 10–14 years, respectively. Although the seroprevalence was still lower in children in the third round of the study, there was an important growth, especially for the youngest children: 3.7% for children under one year [10].
From November 16 to November 29, 2020, a 4th round of ENE-COVID was conducted to estimate the seroprevalence of SARS-CoV-2 in the country after easing restriction measures and increasing mobility. The global seroprevalence in this last round was 9.9% for the country and 4.7% for Asturias [11].
The role of the children has been discussed since the beginning of the pandemic. According to the Report 101 from Red Nacional de Vigilancia Epidemiológica (RENAVE), children under 10 years old represent 9.4% of the total COVID-19 confirmed cases in Spain [12]. It is still unclear what proportion of children are asymptomatic and which symptoms are most associated with pediatric SARS-CoV-2 infections [13,14,15].
Updated seroprevalence estimates are very important to describe the SARS-CoV-2 landscape and to guide public health decisions. The aims of this study are to estimate longitudinal changes in seroprevalence in a cohort of children in a region in Northern Spain, with a very low seroprevalence of SARS-CoV-2 as compared to the national data at the beginning of the pandemic, and to analyze factors associated with SARS-CoV-2 seropositivity.
Methods
Study design and setting
A prospective, multicenter, longitudinal study was designed to analyze the evolution of SARS-CoV-2 antibodies during one year in children in Asturias, a region in Northern Spain with a total population of 1,002,097 people and 95,698 children protected by the National Health System in 2021. Asturias is divided into eight health areas (Fig. 1) with a network of primary care centers as well as a reference hospital for each of the areas. Up to 76% of the total population is concentrated into three major urban areas (Gijón, Oviedo, and Avilés) [16]. A group of 20 pediatricians from the eight health areas in Asturias was created. Patients were recruited between July 1 and September 30, 2020 in public hospitals and primary healthcare centers.
Healthcare map of Asturias with total population and population under 14 years old. This map is obtained from Servicio de Salud del Principado de Asturias [16] and it is permitted to be used publicly.
Sample size justification
The study was designed to assess the seroprevalence of SARS-CoV-2 antibodies at three time points (every six months). To achieve this, about 200 participants were required (assuming a change in the seroprevalence between 1% in the first round and 7% in the third round, alpha of 0.05, beta of 0.2, and a 15% dropout rate).
Participants and study timeline
Children aged between two days and 14 years that needed a blood sample at the time of recruitment or that voluntarily agreed on being part of the study, were eligible to participate. The follow up of the enrolled children was performed until September 2021 for monitoring the evolution of the pandemic. Venous blood samples were collected from participants during three testing rounds as followings.
(1) Round 1 (July to September 2020): baseline estimate of seroprevalence of SARS-CoV-2 after the lockdown and the national seroepidemiological study ENE-COVID.
(2) Round 2 (January to March 2021): estimate of seroprevalence three months after the reopening of schools.
(3) Round 3 (July to September 2021): estimate of seroprevalence one year after the beginning of the study.
Demographic information was collected at the beginning of the study (age, sex, household size, place of residence). The participants were later contacted after every round and a telephonic questionnaire, as well as a chart review, were carried out for COVID-19-compatible symptoms, with a virological test performed and a history of close contact with COVID-19 confirmed or suspected cases during the previous six months.
Ethical aspects
This study was conducted in accordance with the 1964 Declaration of Helsinki and its subsequent amendments. It was approved by the Asturian Research Ethics Committee (2020–315). Written informed consent was obtained from parents of participating children. Children aged 12 and older could confirm the consent themselves. Participants were free to decline consent at any time.
Laboratory analysis
Venous blood samples were collected from participants every six months. Serum was tested for antibodies to SARS-CoV-2 in the Microbiology Laboratory of Hospital Universitario Central de Asturias using the following assays: spike protein assays (DiaSorin LIAISON SARS-CoV-2 TrimericS IgG assay) and nucleocapsid assays (Roche Elecsys anti-SARS-CoV-2) [17, 18].
A summary of the tests used is represented in Table 1. SARS-CoV-2 seropositivity was defined as a positive antibody test using the manufacturer’s advised positivity cutoff in at least one of the assays.
Statistical analysis
Descriptive analysis was performed using frequencies and proportions for categorical variables and medians and interquartile ranges (IQR) for continuous variables. Crude and adjusted seroprevalence for test sensitivity and specificity (Rogan−Gladen formula) [19] were calculated as a proportion with 95% confidence interval (95% CI). The prevalence of antibodies against SARS-CoV-2 was later compared in every round, globally and according to age, household size, and place of residence. When considering the dependence between repeated observations of the same population through time, a Cochran's Q and McNemar's tests were performed for multiple and double pairwise comparisons. This analysis was carried out using R software Version 4.1 (R. Foundation, Vienna, Austria).
Because there was no case of seroreversion during the follow up, the seropositive patients at the end of the study were compared with the negative ones to identify factors associated with SARS-CoV-2 seropositivity. The following variables were analyzed: sex, age, health area, place of residence, household size, contact with a confirmed or suspected COVID-case, previous COVID-19-compatible symptoms, and virological test status (never done, positive or negative) along the time of the study. Chi-square or Fisher's exact test, as appropriate (for categorical variables) and Mann-Whitney U test (for continuous quantitative variables) were carried out for the comparative analysis. To identify factors associated with SARS-CoV-2 seropositivity, each variable was first assessed using a univariate analysis and those with a P value below the cut off of 0.05 was entered later into a binary logistic regression multivariable analysis. This analysis was performed using IBM SPSS Statistics Version 25 statistical package.
Results
Baseline characteristics
In total, 204 children were recruited between June and September 2020, of whom four were excluded because they did not sign the informed consent. Out of the 200 participants, 120 (60%) were enrolled in hospitals and 80 (40%) in primary healthcare centers. Table 2 shows the baseline characteristics of the participants. The median age of the children was 9.7 years (IQR: 6.1–11.9), and 50.5% of them were female. A total of 99 participants (49.5%) reported a chronic condition. Among the participants, 149 children (74.5%) lived in urban, 14 (7%) in peri-urban and 37 (18.5%) in rural areas, and most of them (60.5%) had four to five household members. The sample represented the age and demographic distribution of the children in the region.
Of the 200 children, 195 participated in the first round, 176 in the second and 169 in the last round (dropout rate of 13.3% between the beginning and the end of the follow up).
Variation of seroprevalence
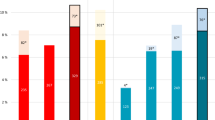
Table 3 represents the distribution of serological results at the three rounds of the study. The overall crude seroprevalence significantly increased during the study from round 1 [3/195; 1.5% (95% CI 0.3%–4.3%)] to round 2 [16/176; 9.1% (95% CI 4.6%–12.7%)] and round 3 [28/169; 16.6% (95% CI 9.5%–19.6%)] (P < 0.001). The adjustments for sensitivity and specificity of the antibody test moved the final estimates upwards, for a final adjusted seroprevalence of 1.8% (95% CI 0.4%–5.1%) in round 1, 10.7% (95% CI 5.4%–14.9%) in round 2 and 19.5% (95% CI 11.2%–23.1%) in round 3. None of the children who were previously positive became seronegative during the time of the study.
Significant differences have been found among seropositivity in all the age groups, with a substantial rise in the group from zero to four years old: from round 1 (0%, 95% CI 0.0%–9.3%) to round 2 (12.5%, 95% CI 2.9%–24.8%), and round 3 (31.0%, 95% CI 11.4%–40.2%) (P = 0.001).
Seroprevalence was the highest in the urban areas along the study (round 3: 20.5%, 95% CI 11.2%–23.8%) vs. in the rural areas (round 3: 3%, 95% CI 0.1%–14.2%), with a significant difference between periods (P < 0.001).
Significant differences in seropositivity rate have also been detected among periods for children with three or less household members: round 1 (3%, 95% CI 0.4%–10.2%), round 2 (9.8%, 95% CI 3.3%–18.2%) and round 3 (16.7%, 95% CI 7.3%–25.4%) (P = 0.005) and for those with four to five household members: round 1 (0.9%, 95% CI 0.0%–4.5%), round 2 (8.7%, 95% CI 3.5%–13.7%), and round 3 (17.3%, 95% CI 8.4%–21.5%) (P < 0.001).
The highest variation of global seroprevalence, as well as the specific estimates occurred between the first (July–September 2020) and the second rounds (January–March 2021) of the study.
Factors associated with seropositivity
At the end of the study (round 3) there were 28/169 seropositive participants (53.6% girls, median age 8.8 years). Of those with positive SARS-CoV-2 antibodies, 10/28 (35.7%) reported no symptoms during the study. The most common symptoms associated with SARS-CoV-2 seropositivity were fever 12/28 (42.9%), cough 6/28 (21.4%), sore throat 4/28 (14.3%), and fatigue (10.7%). No children reported ageusia or anosmia (Fig. 2). Out of the 28 children, 16/28 (57.1%) were previously undetected COVID-19 cases by having either no virological test performed (8/28, 28.6%) or a negative result (8/28, 28.6%); in conclusion, only 12/28 (42.9%) children had a positive virological test. None of the children had severe disease requiring hospital admission.
The univariate analysis of variables associated with SARS-CoV-2 seropositivity is shown in Table 4. Younger age (zero to four years), place of residence (urban area), and previous virological tests showed a significant association in the univariate analysis, but this was no longer significant in the multivariable analysis. The multivariable analysis (Table 5) identified three variables independently associated with SARS-CoV-2 seropositivity: close contact with COVID-19 confirmed or suspected, previous positive virological test, and fatigue.
Discussion
This is the first SARS-CoV-2 seroprevalence study conducted in children in our region, where the prevalence of SARS-CoV-2 antibodies at the beginning of the pandemic was very different compared with the rest of Spain [9]. The seroprevalence is a dynamic parameter and the longitudinal design of the study allowed us to describe its variation between July 2020 and September 2021, a period where important epidemiological changes in the development of the pandemic occurred everywhere. Furthermore, this study enabled us to learn about the behavior of SARS-CoV-2 in children and to guide public health decisions for this population.
In this study, we found that by September 2021, 19.5% (adjusted seroprevalence) of the children had developed antibodies against SARS-CoV-2 after infection, almost two times more than the seroprevalence of 10.7% estimated between January and March 2021 and eleven times more than between January and March 2020 (1.8%). All seropositivity was due to previous infection because the study was carried out before the start of vaccination in children. We must consider that some of the events that happened in Spain between the different rounds of our study could influence this increase of seroprevalence, such as the lockdown on March 14, 2020 or the school reopening on September 21, 2020 [5, 7]. The second wave of COVID-19 that occurred between September and December 2020, right before the second period of our study, was very important in the region. The infection incidence strongly increased in Asturias during this wave. On November 13, 2020, 808 COVID-19 cases were reported (seven-day incidence: 360.7 per 100,000 inhabitants), reaching the highest daily caseload since the start of the pandemic [20]. This is consistent with our data and with the remarkable increase of seroprevalence between the first and second rounds of our study.
Although some SARS-CoV-2 seroprevalence studies have included children, there are not many conducted studies specifically in this group. All of them reported a very variable seropositivity depending on the country, but mostly on the time of the study [15, 21,22,23,24,25,26,27,28,29,30]. The estimated seroprevalence in children in the Spanish, population-based, seroepidemiological study increased along the different rounds of the survey being 3.5%, 2.9%, and 4.1% for the age groups of 0–4 years, 5–9 years, and 10–14 years, respectively in the third round (8–22 June 2020) [10]. In Asturias, the situation was quite different if we look at our data. After the first round of our study, the seroprevalence was much lower: 0%, 0%, and 3.2% for the same age groups.
Interestingly, according to our data the increase in SARS-CoV-2 seroprevalence within a 12-month period was the largest among young children aged zero to four years, changing from 0% in round 1 to 31% in round 3. Between July and September 2021, the seroprevalence in this group was around two times higher than in all the other age groups. This age group may have been more affected by SARS-CoV-2 because these children were under no obligation to wear masks in combination with the constant need of close care from adults. This may be related to the close care that this group of age requires, as well as the exceptions. Nevertheless, age was later not identified as a variable independently associated with SARS-CoV-2 seropositivity. There are few studies where higher seropositivity in younger age is described [15, 30, 31]. On the contrary, a lower seroprevalence is often reported in younger children [9, 24, 26, 32].
As mentioned previously, the adjusted seroprevalence at the end of our study was found to be 19.5%, implying that around 18,700 children in Asturias had been infected by September 30, 2021. By this date, only 6041 pediatric cases had officially been reported in the region [33]. Our estimated seroprevalence was three times greater compared with the cumulative incidence of SARS-CoV-2 infections in children in Asturias. The underreporting of COVID-19 cases has also been described in other publications. Chen et al. described that the ratio of serologically detected infections to virologically confirmed cases varied across locations, with a pooled ratio of 11.1 (95% CI 8.3–14.9), suggesting that for each virologically confirmed COVID-19 case, there were at least ten undetected infections [34]. Ulyte et al. reported that the ratio of children (four to five years old) diagnosed with SARS-CoV-2 infection to those who were seropositive was as high as 1 to 13 [23].
The presence of COVID-19-compatible symptoms was not definite to the seropositive children. Fever and cough are considered to be more specific symptoms [35], but in our study there were no differences between seropositive and seronegative children. Fatigue was the only COVID-19-compatible symptom that was associated with SARS-CoV-2 antibody positivity. Anosmia was not reported by any of the seropositive children. This is consistent with the reports from other studies [15, 22], even though the proportion of asymptomatic infections described in different studies varies greatly ranging from 21.9% to 50% [9, 15, 22]. We must consider that most of the viral upper respiratory infections in children can produce any of the COVID-19-compatible symptoms. On top of that, fatigue is a very unspecific and difficult to measure symptom that could potentially be overestimated by the parents. These mild, unspecific symptoms could explain the high proportion of seropositive children who were not previously diagnosed with a virological test.
A close contact with a COVID-19 confirmed or suspected case was found to be a variable associated with SARS-CoV-2 seropositivity, as well as having a previous positive virological test. This can justify the importance of contact tracing in children, that have more mild, unspecific symptoms and are in lower proportion fully vaccinated. The place of residence was not shown to be associated with SARS-CoV-2 seropositivity in our study, in contrast to the most surveys that reflect a higher incidence of COVID-19 in urban, more populated areas, like estimates from the Spanish seroepidemiological study [10]. We must be careful while interpreting these results, which could be affected by some bias that will be detailed here below.
Some of the limitations of this study are as follows: first, there is a selection bias in terms of who is being tested for SARS-CoV-2 antibodies because we used convenience sampling, which is not completely representative of the population. Patients who have accessed health care or required blood testing for other reasons were included. About 50% of the sample were children with comorbidities. Therefore, seropositivity rates rather than true population prevalence has been calculated; second, the absolute sample size of seropositive participants is relatively small and could bias the multivariable analysis; third, there is a risk of recall bias due to the retrospective nature of data collection relating to symptomatology. Although we attempted to mitigate this problem by the chart review, this bias cannot be ignored, and fourth this study was carried out before the Omicron wave occurred and changed the SARS-CoV-2 scenery. Seroprevalence estimates in children at this moment should certainly be higher.
Our study has several major strengths: first, it is a prospective, multicenter study that includes children from all the different health areas in Asturias; second, the investigation of seroprevalence better estimates the real extent of the infection revealing asymptomatic cases; third, the longitudinal sample allowed us to see the dynamic changes of SARS-CoV-2 antibodies, and fourth the dropout rate during the study was not very high, and all the seropositive patients completed the follow-up.
In conclusion, our study provides seroprevalence estimates of SARS-CoV-2 antibodies in a sample of children in a region in Northern Spain. Our findings highlight how the seroprevalence in children has increased remarkably during the first year of the pandemic. COVID-19-compatible symptoms are very unspecific in children, which could partly explain the high proportion of seropositive children who were not previously diagnosed. The only factors independently associated with SARS-CoV-2 seropositivity were close contact with COVID-19 confirmed or suspected case, previous positive virological test, and fatigue.
Data availability
The datasets generated during and analyzed during the current study are available from the corresponding author on reasonable request.
References
World Health Organization. Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV). 2020. https://www.who.int/news/item/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov). Accessed 27 Feb 2022.
World Health Organization. Director-general’s opening remarks at the media briefing on COVID-19 - 11 March 2020. 2020. https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19%2D%2D-11-march-2020. Accessed 27 Feb 2022.
Linde P. Sanidad confirma en La Gomera el primer caso de coronavirus en España. 2020. https://elpais.com/sociedad/2020/01/31/actualidad/1580509404_469734.html. Accessed 27 Feb 2022.
LORENZO L. Asturias registra el primer caso positivo de coronavirus. 2020. https://www.elcomercio.es/asturias/coronavirus-asturias-primer-caso-positivo-20200229175739-nt.html. Accessed 27 Feb 2022.
FELIPE R. Real Decreto 463/2020, de 14 de marzo, por el que se declara el estado de alarma para la gestión de la situación de crisis sanitaria ocasionada por el COVID-19. 2020. https://www.boe.es/eli/es/rd/2020/03/14/463. Accessed 27 Feb 2022.
FELIPE R. BOE-A-2020–5767 Real Decreto 555/2020, de 5 de junio, por el que se prorroga el estado de alarma declarado por el Real Decreto 463/2020, de 14 de marzo, por el que se declara el estado de alarma para la gestión de la situación de crisis sanitaria ocasionada por el COVID-19. 2020. https://www.boe.es/buscar/act.php?id=BOE-A-2020-5767. Accessed 27 Feb 2022.
Cobierno del Principado de Asturias. Boletín Oficial del Principado de Asturias. núm. 176 de 10-IX-2020. 2020. https://sede.asturias.es/bopa/2020/09/10/20200910.pdf. Accessed 27 Feb 2022.
Ministerio de sanidad. Health preventive measures against COVID-19 in schools during 2020–2021. 2021. https://www.sanidad.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov/documentos/Medidas_centros_educativos_Curso_2020_2021_17.09.20.pdf. Accessed 27 Feb 2022.
Pollán M, Pérez-Gómez B, Pastor-Barriuso R, Oteo J, Hernán MA, Pérez-Olmeda M, et al. Prevalence of SARS-CoV-2 in Spain (ENE-COVID): a nationwide, population-based seroepidemiological study. Lancet. 2020;396:535–44.
Ministerio de Sanidad. Estudio ENE-COVID: Informe final Estudio Nacional de sero-epidemiología de la infección por SARS-CoV-2 en España. 2020. https://www.sanidad.gob.es/ciudadanos/ene-covid/docs/ESTUDIO_ENE-COVID19_INFORME_FINAL.pdf. Accessed 27 Feb 2022.
Ministerio de Sanidad. Estudio ENE-COVID: Cuarta Ronda Estudio Nacional de sero-epidemiología de la infección por SARS-CoV-2 en España. 2020. https://www.sanidad.gob.es/gabinetePrensa/notaPrensa/pdf/15.12151220163348113.pdf. Accessed 27 Feb 2022.
RNVE. Informe no 119 Situación de COVID-19 en España a 23 de febrero de 2022. 2020. https://www.isciii.es/QueHacemos/Servicios/VigilanciaSaludPublicaRENAVE/EnfermedadesTransmisibles/Documents/INFORMES/Informes%20COVID-19/INFORMES%20COVID-19%202022/Informe%20n%C2%BA%20119%20Situaci%C3%B3n%20de%20COVID-19%20en%20Espa%C3%B1a%20a%2023%20de%20febrero%20de%202022.pdf. Accessed 27 Feb 2022.
Dong Y, Mo X, Hu Y, Qi X, Jiang F, Jiang Z, et al. Epidemiology of COVID-19 among children in China. Pediatrics. 2020;145:e20200702.
Tagarro A, Epalza C, Santos M, Sanz-Santaeufemia FJ, Otheo E, Moraleda C, et al. Screening and severity of coronavirus disease 2019 (COVID-19) in children in Madrid. Spain JAMA Pediatr. 2021;175:316–7.
Ulyte A, Radtke T, Abela IA, Haile SR, Blankenberger J, Jung R, et al. Variation in SARS-CoV-2 seroprevalence across districts, schools and classes: baseline measurements from a cohort of primary and secondary school children in Switzerland. BMJ Open. 2021;11:e047483.
Consejería de Salud. Mapa Sanitario 2021 Principado de Asturias. 2021. https://www.astursalud.es/documents/35439/36965/Mapa_Sanitario_2021.pdf/f8959f7b-afa0-d23f-3aab-8e2b564c55a0. Accessed 27 Feb 2021.
Roche diagnostics International. Immunoassay for the qualitative detection of antibodies against SARS-CoV-2. https://diagnostics.roche.com/es/es/products/params/elecsys-anti-sars-cov-2.html. Accessed 27 Feb 2021.
Diasorin. Liaison SARS-CoV-2 TrimericS IgG assay. 2022. https://www.diasorin.com/sites/default/files/allegati_prodotti/liaisonr_sars-cov-2_trimerics_igg_assay_m0870004408_a_lr_0.pdf. Accessed 27 Feb 2022.
Rogan WJ, Gladen B. Estimating prevalence from the results of a screening test. Am J Epidemiol. 1978;107:71–6.
Observatorio de Salud de Asturias. Evolución nuevos casos confirmados. 2022. https://app.powerbi.com/viewr=eyJrIjoiNTdhYzlhYjUtZmFjNi00NjBhLThiNTktMmNjNDY5NzYzNjBlIiwidCI6IjI4ZmI0NmYwLTU0OWYtNDI5Ny1iOTZmLWFjNjJhZTkxY2YwYyIsImMiOjl9&pageName=ReportSectionda82d8ffb60be1590dd8. Accessed 27 Feb 2022.
Tönshoff B, Müller B, Elling R, Renk H, Meissner P, Hengel H, et al. Prevalence of SARS-CoV-2 infection in children and their parents in southwest Germany. JAMA Pediatr. 2021;175:586–93.
Waterfield T, Watson C, Moore R, Ferris K, Tonry C, Watt A, et al. Seroprevalence of SARS-CoV-2 antibodies in children: a prospective multicentre cohort study. Arch Dis Child. 2021;106:680–6.
Ulyte A, Radtke T, Abela IA, Haile SR, Berger C, Huber M, et al. Clustering and longitudinal change in SARS-CoV-2 seroprevalence in school children in the canton of Zurich, Switzerland: prospective cohort study of 55 schools. BMJ. 2021;372:n616.
Stringhini S, Zaballa ME, Pullen N, Perez-Saez J, de Mestral C, Loizeau AJ, et al. Seroprevalence of anti-SARS-CoV-2 antibodies 6 months into the vaccination campaign in Geneva, Switzerland, 1 June to 7 July 2021. Euro Surveill. 2021;26:2100830.
Nwosu K, Fokam J, Wanda F, Mama L, Orel E, Ray N, et al. SARS-CoV-2 antibody seroprevalence and associated risk factors in an urban district in Cameroon. Nat Commun. 2021;12:5851.
Yang HS, Costa V, Racine-Brzostek SE, Acker KP, Yee J, Chen Z, et al. Association of age with SARS-CoV-2 antibody response. JAMA Netw Open. 2021;4:e214302.
Ristić M, Milosavljević B, Vapa S, Marković M, Petrović V. Seroprevalence of antibodies against SARS-CoV-2 virus in Northern Serbia (Vojvodina): a four consecutive sentinel population-based survey study. PLoS ONE. 2021;16:e0254516.
Smith BK, Janowski AB, Fremont AC, Adams LJ, Dai YN, Farnsworth CW, et al. Progression of SARS-CoV-2 seroprevalence in St Louis, Missouri, through January 2021. mSphere. 2021;6:e0045021.
Popova AY, Smirnov VS, Andreeva EE, Babura EA, Balakhonov SV, Bashketova NS, et al. SARS-CoV-2 seroprevalence structure of the Russian population during the COVID-19 pandemic. Viruses. 2021;13:1648.
Barcellini L, Forlanini F, Sangiorgio A, Gambacorta G, Alberti L, Meta A, et al. Does school reopening affect SARS-CoV-2 seroprevalence among school-age children in Milan? PLoS ONE. 2021;16:e0257046.
Charlton CL, Nguyen LT, Bailey A, Fenton J, Plitt SS, Marohn C, et al. Pre-vaccine positivity of SARS-CoV-2 antibodies in Alberta, Canada during the first two waves of the COVID-19 pandemic. Microbiol Spectr. 2021;9:e0029121.
Viner RM, Mytton OT, Bonell C, Melendez-Torres GJ, Ward J, Hudson L, et al. Susceptibility to SARS-CoV-2 infection among children and adolescents compared with adults: a systematic review and meta-analysis. JAMA Pediatr. 2021;175:143–56.
Observatorio de Salud de Asturias. Niveles de alerta COVID 19. 2022. https://obsaludasturias.com/obsa/niveles-covid-19/. Accessed 27 Feb 2021.
Chen X, Chen Z, Azman AS, Deng X, Sun R, Zhao Z, et al. Serological evidence of human infection with SARS-CoV-2: a systematic review and meta-analysis. Lancet Glob Health. 2021;9:e598–609.
Viner RM, Ward JL, Hudson LD, Ashe M, Patel SV, Hargreaves D, et al. Systematic review of reviews of symptoms and signs of COVID-19 in children and adolescents. Arch Dis Child. 2021;106:802–7.
Acknowledgements
Authors express their gratitude to their colleagues involved in the data collection of this study. This project has been carried out with the collaboration of: Sara Lozano-Losada, Helena Higelmo-Gómez, Mª Agustina Alonso-Álvarez, Juan Pérez-Gordón, Ignacio Carvajal-Urueña, María Morán-Poladura, Cristina Suárez-Castañón, MªCristina Amigo-Bello, Reyes Fernández-Montes, Águeda García-Merino, Cristina Rodríguez-Dehli, Belén Gómez-González, Eva Braga-Riera and Laura Míguez-Martín. They are also grateful to Fundación Ernesto Sánchez Villares for the donation of a grant and to all the children and their families that wanted to participate in this study.
Funding
Elisa García-García received partial financial support from Fundación Ernesto Sánchez Villares, Sociedad de Pediatría de Asturias, Cantabria y Castilla y León (SCCALP; grant number 2021/02). The remaining authors received no external funding.
Author information
Authors and Affiliations
Contributions
CML: conceptualization, methodology, project administration, resources, software, supervision, validation, visualization. GGE: data curation, formal analysis, funding acquisition, investigation, methodology, writing–original draft. PMC: investigation, writing–review and editing. PSD: investigation. RPM: methodology, supervision, validation and visualization. CRA: project administration, resources and software. MNC: project administration, resources, software, writing–review and editing. FEMF and NGG: writing–review and editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest. Non-financial benefits have been received or will be received from any party related directly or indirectly to the subject of this article.
Ethical approval
This study was conducted in accordance with the 1964 Declaration of Helsinki and its subsequent amendments. It was approved by the Asturian Research Ethics Committee (2020–315). Written informed consent was obtained from parents of participating children. Children aged 12 and older could confirm the consent themselves. Participants were free to decline consent at any time.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
García-García, E., Rodríguez-Pérez, M., Pérez-Solís, D. et al. Variation in SARS-CoV-2 seroprevalence in children in the region of Asturias, Northern Spain. World J Pediatr 18, 835–844 (2022). https://doi.org/10.1007/s12519-022-00617-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12519-022-00617-2