Abstract
Background
The real-world exposure levels of non-therapeutic antibiotics and neonicotinoids in type 1 diabetes (T1D) children and their associations as environmental triggers through gut microbiota shifts remained unknown. We thus investigated the antibiotics and neonicotinoids’ exposure levels and their associations with gut microbiota in pediatric T1D.
Methods
Fifty-one newly onset T1D children along with 67 age-matched healthy controls were recruited. Urine concentrations of 28 antibiotics and 12 neonicotinoids were measured by mass spectrometry. Children were grouped according to the kinds of antibiotics’ and neonicotinoids’ exposures, respectively. The 16S rRNA of fecal gut microbiota was sequenced, and the correlation with urine antibiotics and neonicotinoids’ concentrations was analyzed.
Results
The overall detection rates of antibiotics were 72.5% and 61.2% among T1D and healthy children, whereas the neonicotinoids detection rates were 70.6% and 52.2% (P = 0.044). Children exposed to one kind of antibiotic or two or more kinds of neonicotinoids had higher risk of T1D, with the odd ratios of 2.579 and 3.911. Furthermore, co-exposure to antibiotics and neonicotinoids was associated with T1D, with the odd ratio of 4.924. Antibiotics or neonicotinoids exposure did not affect overall richness and diversity of gut microbiota. However, children who were exposed to neither antibiotics nor neonicotinoids had higher abundance of Lachnospiraceae than children who were exposed to antibiotics and neonicotinoids alone or together.
Conclusion
High antibiotics and neonicotinoids exposures were found in T1D children, and they were associated with changes in gut microbiota featured with lower abundance of butyrate-producing genera, which might increase the risk of T1D.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Type 1 diabetes (T1D) is a chronic organ-specific autoimmune disease characterized by β-cell-targeted autoimmune processes and insulin deficiency [1]. It is estimated that there are over 1.11 million T1D children < 19 years old worldwide, although there are ethnic and regional differences in these estimates [2]. A ~ 2% to ~ 3% or even higher global annual incidence increasing rate and the rising proportion of cases defined by low human leukocyte antigen (HLA) risks indicate the growing effects of environmental factors [3], including infections, gut microbiota, and nutrition, on the development of T1D in addition to genetic susceptibility [1, 4, 5]. Despite recent advancements in knowledge concerning associations between gut microbiota and T1D development, much remains unknown regarding the specific role of gut microbiota in T1D [6]. T1D patients have unique gut microbiota, but lack uniformity. Some studies found a lower α diversity, high Bacteroidetes:Firmicutes ratio and low abundance of butyrate-producing species among T1D patients [4]. These characteristics might affect intestinal permeability and molecular mimicry and thereby modulate the innate and adaptive immune systems to ultimately lead to islet autoimmunity [6].
Substance intake via food, such as additives, residual pesticides, and veterinary antibiotics, can affect gut microbiota. A previous study identified perturbation of gut microbiota by antibiotics, revealing a shift in the Bacteroidetes: Firmicutes ratio due to the aminoglycoside streptomycin [7]. Use of antibiotics not only exerts short-term effects on gut microbiota but also results in prolonged pathogen susceptibility. Another study found that early life antibiotics exposure increased the risk of developing immune and metabolic diseases [8, 9]. Pulsed therapeutic antibiotics administered early in life perturbed gut microbiota and its metabolic capacities, leading to changes in T-cell populations and higher T1D incidence in mice [10], though there was no evidence that the occurrence of T1D was related to antibiotics exposures among children [4]. Moreover, oral administration of a prophylactic antibiotic mixture decreased the abundance of butyrate-producing microbes [11], with this possibly related to T1D onset.
Neonicotinoids are a class of widely used pesticides, chronic exposure to which is reportedly related to heart defects, autism spectrum disorders, and diseases of the nervous system [12]. A recent study showed that neonicotinoids affected the gut microbiota of animals, revealing that imidacloprid disrupted the balance between gut microbiota and gut–barrier function [13, 14]. However, its effect on human gut microbiota remains unclear.
Currently, antibiotics and neonicotinoids are widely used in modern agriculture and animal husbandry, and children can be exposed to antibiotics and neonicotinoids through food, water, and even environmental exposure. However, their effects on children T1D in the real world via the potential gut microbiota changes are still unknown. We hypothesized that the structure of gut microbiota in children might differ depending on their level of exposure to antibiotics and neonicotinoids, which could potentially lead to differences in the risk of T1D. In the present study, we used urinary antibiotics and neonicotinoids levels to infer their exposure levels. We analyzed the gut microbiota of children with different urine antibiotics and neonicotinoids concentrations to determine associations between differences in gut microbiota and T1D onset.
Methods
Study population
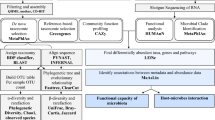
This multi-center cross-sectional study collected samples from eight cities in different regions of China, including Fuzhou, Nanchang, Shanghai, Suzhou, Jinan, Taiyuan, Changchun, and Zhengzhou. A total of 70 newly diagnosed T1D patients < 18 years old with disease duration < 1 month were included in this study during the study period from January 2019 to March 2020. The diagnosis of T1D was based on the criteria of the International Society for Pediatric and Adolescent Diabetes [15]. The healthy control group was matched with the T1D group by region, sex, age, and time of visit. Cases were excluded if they were < 2 years old, received antibiotic treatment within one month, and presented with infectious diseases, chronic or acute gastrointestinal diseases, other inherited metabolic disorders, and/or serious chronic disorders (Fig. 1). This study was approved by the Ethics Committee of Children’s Hospital of Fudan University ([2019]210), and the guardians of the children provided written informed consent before information and sample collection.
Sample collection
The clinical characteristics including sex, age, time of visit, fasting blood glucose, HbA1c, and serum C-peptide of T1D patients and healthy control children were obtained through questionnaires administered by the doctors. Fecal samples and first morning urine samples were collected in dedicated sterile containers provided by the research team. Trained medical staff guided and supervised sample collection. Fecal and urine samples were frozen in freezers immediately after collection. Frozen fecal and urine samples were transported on dry ice to the Children’s Hospital of Fudan University within 24 hours of collection and were stored at − 80 °C until analysis.
Fecal gut microbiota DNA extraction, 16S rRNA sequencing, and bioinformatics analysis
Total bacterial DNA was extracted using a DNA extraction kit according to the manufacturer’s instructions (DNeasy PowerSoil Kit). DNA was diluted to 1 ng/μL and stored at − 20 °C until further processing. The barcoded primers and Takara Ex Taq reagent (Takara, Dalian, China) were used for polymerase chain reaction (PCR) amplification of bacterial 16S rRNA genes. The 16S rRNA V3-V4 region was amplified with universal primers 343F and 798R for bacterial diversity analysis. After purification, the final amplicon was quantified with a Qubit double-strain DNA (dsDNA) assay kit. Equal quantities of purified amplicon were pooled to prepare for subsequent sequencing. After removing low-quality sequences, paired-end reads were assembled using the fast ligation-based automatable solid-phase high-throughput system with a minimum and maximum overlap of 10 bp and 200 bp, respectively, and a 20% maximum mismatch rate [16]. The 16S rRNA sequencing data were analyzed using QIIME software (v.1.8.0), and sequences were assigned to operational taxonomic units using Vsearch software (97% similarity cut-off) [17, 18]. Representative reads were annotated and subjected to a BLAST search against the Silva database (v.123.0) using the Ribosomal Database Project classifier with a 0.70 confidence threshold [19].
Selection and analysis of urine antibiotics
The selection of antibiotics was mainly based on previous studies [20]. Briefly, 28 antibiotics and five categories of metabolites (macrolide, tetracycline, fluoroquinolone, sulfonamide, and phenicol) were analyzed. All antibiotics were divided into three categories according to use: veterinary antibiotics (VA), human antibiotics (HA), and veterinary/human antibiotics (V/HA). The types of antibiotics that children can use are limited (e.g., fluoroquinolone and tetracycline are restricted for use in children); therefore, most antibiotics in the V/HA group were more likely to be exposed to children through food and water. Thus, VA + V/HA concentrations can reflect exposure to antibiotics in addition to medication. Concentrations of antibiotics were measured by isotope dilution ultra-performance liquid chromatography coupled to quadrupole time-of-flight mass spectrometry (UPLC-Q/TOF MS) according to previously described methods [20].
Selection and analysis of urine neonicotinoids
Briefly, eight neonicotinoids and four typical metabolites were detected according to previous studies, with isotope dilution UPLC-Q/TOF MS specifically used for neonicotinoid measurement [21].
Statistical analysis
The concentrations of urine antibiotics and neonicotinoids were adjusted by the urine creatinine levels (Supplementary Table 1). In case of underreporting of the history of antibiotic use in the previous month, we removed data for patients with urine creatinine-adjusted HA concentrations over the 95th percentile. Ultimately, 10 T1D cases and 8 control cases were excluded. Once a measurable value of one kind of antibiotic or neonicotinoid is detected in urine, the child was considered to be exposed to that antibiotic or neonicotinoid. Children were grouped according to the kinds of antibiotics, VA + V/HA or neonicotinoids they were exposed to (no exposure, exposure to one kind, or exposure to two or more kinds). To analyze the combined effect of antibiotics and neonicotinoids exposure, children were also grouped into four groups according to whether they were exposed to one or more kind of antibiotics and/or neonicotinoids (the no ANTI & no NEO group for children without exposure to antibiotics or neonicotinoids; the ANTI & no NEO group for children only exposed to one or more kind of antibiotics; the no ANTI & NEO group for children only exposed to one or more kind of neonicotinoids; and the ANTI & NEO group for children exposed to both one or more kind of antibiotics and one or more kind of neonicotinoids). Furthermore, the association of the urine total concentrations of antibiotics, VA + V/HA or neonicotinoids with clinical characteristics and gut microbiota structure were also analyzed.
Statistical analysis was performed using R software (https://www.r-project.org/, version 4.3). For clinical variables, we used χ2 tests to compare categorical variables. Student’s t test was used to compare differences between two groups for normally distributed continuous variables, and the Mann–Whitney U test was used for variables that were not normally distributed. The indices of α-diversity and β-diversity were calculated in R using the “vegan” and “mixOmics” packages using permutational multivariate analysis, principal component analysis and sparse partial least-squares discriminant analysis. To determine specific taxa, linear discriminant analysis (LDA) effect size was calculated online (http://huttenhower.sph.harvard.edu/galaxy/). A P < 0.05 was considered significant.
Results
Clinical characteristic of the patients
Among 51 T1D children and 67 healthy control children, 22 (43.1%) and 28 (41.8%) were female, respectively (P = 0.883), with a mean age of 7.51 ± 3.61 years and 8.10 ± 2.91 years (P = 0.325) (Table 1). The T1D group displayed severely abnormal glucose metabolism, with higher fasting blood glucose levels [17.21 mmol/L (10.55–24.60 mmol/L) vs. 4.90 mmol/L (4.72–5.16 mmol/L)] (P < 0.001) and HbA1c levels [11.80% (10.30–13.40%) vs. 5.10% (4.88–5.43%)] (P < 0.001) than the control group. The C-peptide concentration of the T1D group was 0.21 μg/mL (0.11–0.40 μg/mL).
Detection rate of urinary antibiotics and neonicotinoids
Among 28 kinds of antibiotics and metabolites, 18 kinds of antibiotics were found in all 118 urine samples, with an overall detection rate of 66.1% (78/118) (Supplementary Tables 1, 2). The detection rate of all antibiotics in the T1D group was slightly higher than that of the control group, although there was no significant difference (72.5 vs. 61.2%; P = 0.197). Among all cases, 43 children (36.4%) were exposed to one kind of antibiotics, while 45 children (38.1%) were exposed to two or more kinds of antibiotics (Supplementary Table 3). The detection rates of HA, VA, V/HA, and VA + V/HA were 26.3% (31/118), 14.4% (17/118), 47.5% (56/118), and 53.4% (63/118), respectively.
Among the five antibiotic categories, fluoroquinolone showed the highest detection frequency at 39.8% (47/118), followed by macrolide (24.6%, 29/118), sulfonamide (12.7%, 15/118), tetracycline (10.2%, 12/118), and phenicol (8.5%, 10/118). The T1D group and the control group showed similar detection rates across categories.
Eleven kinds of neonicotinoids and metabolites were detected in all urine samples [detection rate: 60.2% (71/118)]. There were 37 children (31.4%) exposed to one kind of neonicotinoid, while 34 (28.8%) were exposed to two or more. The neonicotinoid-detection rate in the T1D group was significantly higher than that in the control group (70.6 vs. 52.2%; P = 0.044).
The association between antibiotics/neonicotinoids’ exposure and T1D risks
Children who were exposed to one kind of antibiotics were at higher risk of T1D compared to children without antibiotics exposure [odds ratio (OR) = 2.579, 95% confidence interval (CI): 1.061–6.271; P = 0.037] (Supplementary Table 4). Furthermore, children who were exposed to two or more kinds of neonicotinoids also presented higher risk of T1D (OR = 3.911, 95% CI: 1.538–9.945; P = 0.004]. When analyzing the combined effect of antibiotics and neonicotinoids, we found that children who were exposed to both one or more kinds of antibiotics and one or more kinds of neonicotinoids had higher risk of T1D than those who were not exposed to antibiotics or neonicotinoids, with the odd ratio of 4.924 (95% CI 1.239–19.572; P = 0.024) (Supplementary Table 4).
Moreover, fasting blood glucose levels were elevated according to increases in the urine creatinine-adjusted neonicotinoids concentration (r = 0.436, 95% CI 0.720–1.853; P < 0.001), with these levels similar only when considering T1D cases (r = 0.369, 95% CI 0.201–1.393; P = 0.010) (Fig. 2). Among the neonicotinoids-positive T1D cases, the onset age was significantly negatively correlated with the urine creatinine-adjusted neonicotinoids’ concentration (r = − 0.398, 95% CI − 0.580 to − 0.063; P = 0.026), whereas the urine creatinine-adjusted antibiotics concentration showed no significant relationship with T1D-onset age (P = 0.166) or fasting blood glucose (P = 0.848).
The association between the adjusted neonicotinoids’ concentrations and the fasting blood glucose levels or the onset age of type 1 diabetes (T1D) among T1D children a The association between the adjusted neonicotinoids’ concentrations and the fasting blood glucose levels. The violet bar showed the 95% confidence interval (CI); b the association between the adjusted neonicotinoids’ concentrations and the onset age of T1D. The green bar showing 95% CI
Gut microbiota features in T1D
The T1D group showed a characteristic gut–microbiota structure. Both the Shannon index (P = 0.016) and Chao1 index (P = 0.007) were significantly decreased in the T1D group relative to the control group (Supplementary Fig. 1a, b). Permutational multivariate analysis of variance indicated significant differences in β-diversity between the T1D and control groups (P = 0.032, R2 = 0.022) (Supplementary Fig. 1c).
At the phylum level, the T1D group showed a significantly lower abundance of Firmicutes (P = 0.001) and a higher abundance of Proteobacteria (P = 0.001) relative to the control group. Furthermore, the T1D group was characterized by a decrease in butyrate-producing genera within Lachnospiraceae and Ruminococcaceae (i.e., Faecalibacterium, Agathobacter, Lachnospira, Roseburia, and Blautia) and an increase in opportunistic pathogens within Enterobacteriaceae (Escherichia and Shigella) (Supplementary Fig. 2).
Association between urinary antibiotic/neonicotinoid concentrations and gut microbiota
Alpha diversity and beta diversity
The antibiotics and neonicotinoids’ exposure did not perturb the diversity and richness of gut microbiota. We found no significant difference in the Shannon index and Chao1 index between the control and the T1D group with one kind of, two or more kinds of and without antibiotics, VA + V/HA or neonicotinoids’ exposure (Supplementary Fig. 3). Additionally, β-diversity was similar among these groups. There was also no significant difference of the diversity and richness of gut microbiota among the no ANTI & no NEO group; the ANTI & no NEO group; the no ANTI & NEO group; and the ANTI & NEO group.
Differential abundance of taxa
Separate and combined exposure to antibiotics or neonicotinoids did not significantly affect the structure of gut microbiota both among T1D children and healthy children at the phylum level (Supplementary Fig. 4). However, at the family level, the no ANTI & no NEO group had significantly higher abundance of Lachnospiraceae than the other three groups (P = 0.021, Fig. 3a). According to LDA, higher abundance of Lachnospiraceae, including Eubacterium eligens, Coprococcus_1 and Lachnospiraceae_UCG_004, and Saccharimonadaceae were found in the no ANTI & no NEO group; while a higher abundance of Ruminococcaceae_UBA1819 was found in the ANTI & NEO group (Fig. 3b). Furthermore, the abundance of Lachnospiraceae was negatively related with the concentrations of adjusted antibiotics (r = −0.20, P = 0.031) and neonicotinoids (r = −0.21, P = 0.022) (Fig. 3c).
Alterations in gut microbiota between children with different exposure levels to VA + V/HA and neonicotinoids. a The relative abundance of Lachnospiraceae among different groups; b LDA results among the no ANTI & no NEO group, the ANTI & no NEO group, the no ANTI & NEO group, and the ANTI &NEO group of all cases; c The association of adjusted urine VA + V/HA and neonicotinoids’ concentrations and the relative abundance of gut microbiota. The heatmap showed the Spearman’s rank correlation coefficient between the relative abundance of bacterial families with a mean relative abundance ≥ 1% and the adjusted concentration of antibiotics and neonicotinoids. Asterisks represent statistically significant odds ratios. *P < 0.05, †P < 0.01. No ANTI & no NEO group for children without exposure to antibiotics or neonicotinoids, ANTI & no NEO group for children only exposed to one or more kind of antibiotics, no ANTI & NEO group for children only exposed to one or more kind of neonicotinoids, ANTI & NEO group for children exposed to both one or more kind of antibiotics and one or more kind of neonicotinoids, LDA linear discriminant analysis, VA + V/HA veterinary antibiotics and veterinary/human antibiotics (V/HA), T1D type 1 diabetes, NS not significant
Discussion
This study analyzed the effects of non-therapeutic doses of antibiotics and neonicotinoids in the form of environmental exposure on the gut microbiota of children and their potential association with T1D. The results showed that children exposed to antibiotics and neonicotinoids displayed specific changes in gut microbiota and more serious glucose metabolism disorders.
Because of the inappropriate use of antibiotics and pesticides in animal husbandry, aquaculture, and agriculture, excessive residues of antibiotics and pesticides are found in food, water, soil, dust, and air [22,23,24,25,26]. Children are inevitably exposed to various antibiotics and pesticides in daily life, and the exposure levels were related to living and eating habits [20, 21]. Wang et al. [20] reported an overall detection rate of 56.0% for antibiotics and 50.7% for VA + V/HA in urine from school children in Shanghai. Among preschool and primary school children in Hong Kong of China, the VA detection rate was 77.4% [23]. In the present study, we found slightly higher detection rates for all antibiotics and VA + V/HA compared to that reported by Wang et al. [20], but we found lower than that from the study in Hong Kong, China [23]. The differences in detection rates might be due to various factors, such as diet structure, regional differences, and local restrictions on the use of antibiotics. The detection frequency of neonicotinoids was slightly higher than that for VA + V/HA, with 60.2% found in the present study compared to 81.3% in a previous study among Shanghai children [21]. Although Osaka et al. [27] identified a lower detection frequency of neonicotinoids (58%), they reported detection rates > 90% for other classes of pesticides.
Increasing attention has been focused on the potential health effects associated with intake of undetected antibiotics and neonicotinoids. In addition to antibiotic resistance, long-term exposure to antibiotic residues is related to metabolic disorders, including obesity, type 2 diabetes, immune diseases, and even reproductive problems [8, 9, 28]. Neonicotinoids exert neurotoxic effects on nicotinic acetylcholine receptors and have been associated with disorders related to dysfunctional nervous system development [12]. Additionally, recent studies found that neonicotinoids are related to the development of congenital heart defects and autism spectrum disorders, as well as their associations with immunotoxicity, hepatotoxicity, nephrotoxicity, and reproductive toxicity in mammals [12, 21, 29, 30]. However, most existing studies on the health risks caused by antibiotics and pesticides tend to focus on the effect of high levels of exposure over short periods, because relationships between long-term low-dose exposure and health risks are ambiguous and difficult to study. As a result, the mechanisms associated with their adverse effects on health remain unclear.
The impairment of gut microbiota could represent a direct mechanism by which daily low-dose antibiotic and pesticide exposure affects health; however, a few studies have addressed this. To the best of our knowledge, the present study is the first to systematically analyze the association between the exposure to antibiotics and pesticides and gut microbiota in daily life. We found that high levels of exposure to antibiotics and neonicotinoids did not influence the richness and diversity of gut microbiota. This agreed with a study by Akagawa et al. [31], which indicated that continuous antibiotic prophylaxis of trimethoprim-sulfamethoxazole in children did not alter gut microbiota diversity. However, the findings of the present study did show that exposure to antibiotics and neonicotinoids was associated with small but critical changes to gut microbiota, specifically by perturbing certain taxa and especially butyrate-producing genera, including Lachnospiraceae. Keerthisinghe et al. [32] found that sub-pharmaceutical and dietary exposure levels to tetracycline altered vitamin, nucleotide, and amino acid metabolism by gut microbiota in vitro with a distinct dose–response relationship and induced the release of lipopolysaccharides.
The role of gut microbiota in the onset of immune-related diseases has recently received widespread attention. Reduced bacterial diversity and a decreased abundance of bacteria capable of producing butyrate or lactate were identified in children that later progressed to clinical T1D [33]. The Environmental Determinants of Diabetes in the Young study found that fermentation and biosynthesis of short-chain fatty acids were impaired in T1D children, although this was not consistently associated with particular taxa [34]. In the present study, we found that the abundance of butyrate-producing taxa was consistently lower in children who experienced exposure to antibiotics and neonicotinoids, as well as T1D children. Butyrate exhibits anti-inflammatory effects and helps maintain intestinal-barrier integrity [35]. Thus, our study suggested that exposure to antibiotics and neonicotinoids in daily life might be related to impaired intestinal-barrier function, which might lead to an auto-inflammatory response and autoimmune diseases, including T1D.
This study has some limitations. Different individuals exhibit different responses to the same exposure levels based on their respective gut microbiota. Future research should examine the characteristics of children showing a higher degree of sensitivity to antibiotics and pesticides exposure to define prevention criteria for certain groups. Furthermore, the establishment of birth cohorts to monitor the effects of antibiotics and neonicotinoids’ exposures on gut microbiota, metabolism, and immune levels over a long period of time might help us better understand the relationship between antibiotics and neonicotinoids’ exposures and the onset of T1D.
In summary, this study systematically analyzed the association between daily antibiotics and neonicotinoids’ exposure and the structure of gut microbiota of children with and without T1D. We found that children with exposure to antibiotics and neonicotinoids had small but critical changes in gut microbiota, characterizing by a lower abundance of butyrate-producing genera, especially Lachnospiraceae. Similar changes were also observed in T1D children, which were thought to be associated with the increase of autoimmune level. These findings suggest that exposure to high levels of antibiotics and pesticides in daily life might increase the risk of autoimmune diseases, such as T1D. Future work should focus on relationships between antibiotics and neonicotinoids exposure and the onset of autoimmune diseases in children, as well as the underlying mechanisms.
Data availability
Data are available on request from the authors.
References
DiMeglio LA, Evans-Molina C, Oram RA. Type 1 diabetes. Lancet. 2018;391:2449–62.
Anderson K, Norman D, Wittwer G. IDF DIABETES ATLAS Ninth edition. 2019. https://diabetesatlas.org/. Accessed 27 Dec 2019
Zhao Z, Sun C, Wang C, Li P, Wang W, Ye J, et al. Rapidly rising incidence of childhood type 1 diabetes in Chinese population: epidemiology in Shanghai during 1997–2011. Acta Diabetol. 2014;51:947–53.
Ilonen J, Lempainen J, Veijola R. The heterogeneous pathogenesis of type 1 diabetes mellitus. Nat Rev Endocrinol. 2019;15:635–50.
Patterson CC, Harjutsalo V, Rosenbauer J, Neu A, Cinek O, Skrivarhaug T, et al. Trends and cyclical variation in the incidence of childhood type 1 diabetes in 26 European centres in the 25 year period 1989–2013: a multicentre prospective registration study. Diabetologia. 2019;62:408–17.
Zheng P, Li Z, Zhou Z. Gut microbiome in type 1 diabetes: a comprehensive review. Diabetes Metab Res Rev. 2018;34:e3043.
Thompson JA, Oliveira RA, Djukovic A, Ubeda C, Xavier KB. Manipulation of the quorum sensing signal AI-2 affects the antibiotic-treated gut microbiota. Cell Rep. 2015;10:1861–71.
Bailey LC, Forrest CB, Zhang P, Richards TM, Livshits A, DeRusso PA. Association of antibiotics in infancy with early childhood obesity. JAMA Pediatr. 2014;168:1063–9.
Hviid A, Svanström H, Frisch M. Antibiotic use and inflammatory bowel diseases in childhood. Gut. 2011;60:49–54.
Livanos AE, Greiner TU, Vangay P, Pathmasiri W, Stewart D, McRitchie S, et al. Antibiotic-mediated gut microbiome perturbation accelerates development of type 1 diabetes in mice. Nat Microbiol. 2016;1:16140.
Palleja A, Mikkelsen KH, Forslund SK, Kashani A, Allin KH, Nielsen T, et al. Recovery of gut microbiota of healthy adults following antibiotic exposure. Nat Microbiol. 2018;3:1255–65.
Cimino AM, Boyles AL, Thayer KA, Perry MJ. Effects of neonicotinoid pesticide exposure on human health: a systematic review. Environ Health Perspect. 2017;125:155–62.
Yang G, Yuan X, Jin C, Wang D, Wang Y, Miao W, et al. Imidacloprid disturbed the gut barrier function and interfered with bile acids metabolism in mice. Environ Pollut. 2020;266:115290.
Yan S, Tian S, Meng Z, Teng M, Sun W, Jia M, et al. Exposure to nitenpyram during pregnancy causes colonic mucosal damage and non-alcoholic steatohepatitis in mouse offspring: the role of gut microbiota. Environ Pollut. 2021;271:116306.
Mayer-Davis EJ, Kahkoska AR, Jefferies C, Dabelea D, Balde N, Gong CX, et al. ISPAD Clinical practice consensus guidelines 2018: definition, epidemiology, and classification of diabetes in children and adolescents. Pediatr Diabetes. 2018;19:7–19.
Reyon D, Tsai SQ, Khgayter C, Foden JA, Sander JD, Joung JK. FLASH assembly of TALENs for high-throughput genome editing. Nat Biotechnol. 2012;30:460–5.
Caporaso JG, Kuczynski J, Stombaugh J, Bittinger K, Bushman FD, Costello EK, et al. QIIME allows analysis of high- throughput community sequencing data. Nat Methods. 2010;7:335–6.
Edgar RC, Haas BJ, Clemente JC, Quince C, Knight R. UCHIME improves sensitivity and speed of chimera detection. Bioinformatics. 2011;27:2194–200.
Wang Q, Garrity GM, Tiedje JM, Cole JR. Naïve Bayesian classifier for rapid assignment of rRNA sequences into the new bacterial taxonomy. Appl Environ Microbiol. 2007;73:5261–7.
Wang H, Tang C, Yang J, Wang N, Jiang F, Xia Q, et al. Predictors of urinary antibiotics in children of Shanghai and health risk assessment. Environ Int. 2018;12:507–14.
Wang H, Yang D, Fang H, Han M, Tang C, Wu J, et al. Predictors, sources, and health risk of exposure to neonicotinoids in Chinese school children: a biomonitoring-based study. Environ Int. 2020;143:105918.
Chen J, Ying GG, Deng WJ. Antibiotic residues in food: extraction, analysis, and human health concerns. J Agric Food Chem. 2019;67:7569–86.
Li N, Ho KWK, Ying GG, Deng WJ. Veterinary antibiotics in food, drinking water, and the urine of preschool children in Hong Kong. Environ Int. 2017;108:246–52.
Wan Y, Wang Y, Xia W, He Z, Xu S. Neonicotinoids in raw, finished, and tap water from Wuhan, Central China: assessment of human exposure potential. Sci Total Environ. 2019;675:513–9.
Wang A, Mahai G, Wan Y, Jiang Y, Meng Q, Xia W, et al. Neonicotinoids and carbendazim in indoor dust from three cities in China: spatial and temporal variations. Sci Total Environ. 2019;695:133790.
Wei R, He T, Zhang S, Zhu L, Shang B, Li Z, et al. Occurrence of seventeen veterinary antibiotics and resistant bacterias in manure-fertilized vegetable farm soil in four provinces of China. Chemosphere. 2019;215:234–40.
Osaka A, Ueyama J, Kondo T, Nomura H, Sugiura Y, Saito I, et al. Exposure characterization of three major insecticide lines in urine of young children in Japan-neonicotinoids, organophosphates, and pyrethroids. Environ Res. 2016;147:89–96.
Chou H, Wang J, Chang C, Lee J, Shau W, Lai M. Risk of severe dysglycemia among diabetic patients receiving levofloxacin, ciprofloxacin, or moxifloxacin in Taiwan. Clin Infect Dis. 2013;57:971–80.
Carmichael SL, Yang W, Roberts E, Kegley SE, Padula AM, English PB, et al. Residential agricultural pesticide exposures and risk of selected congenital heart defects among offspring in the San Joaquin Valley of California. Environ Res. 2014;135:133–8.
Keil AP, Daniels JL, Hertz-Picciotto I. Autism spectrum disorder, flea and tick medication, and adjustments for exposure misclassification: the CHARGE (CHildhood Autism Risks from Genetics and Environment) case-control study. Environ Heal A Glob Access Sci Source. 2014;13:1–10.
Akagawa Y, Kimata T, Akagawa S, Yamaguchi T, Kato S, Yamanouchi S, et al. Impact of long-term low dose antibiotic prophylaxis on Gut microbiota in children. J Urol. 2020;204:1320–5.
Keerthisinghe TP, Wang M, Zhang Y, Dong W, Fang M. Low-dose tetracycline exposure alters gut bacterial metabolism and host-immune response: “personalized” effect? Environ Int. 2019;131:104989.
Knip M, Siljander H. The role of the intestinal microbiota in type 1 diabetes mellitus. Nat Rev Endocrinol. 2016;12:154–67.
Vatanen T, Franzosa EA, Schwager R, Tripathi S, Arthur TD, Vehik K, et al. The human gut microbiome in early-onset type 1 diabetes from the TEDDY study. Nature. 2018;562:589–94.
Feng Y, Wang Y, Wang P, Huang Y, Wang F. Short-Chain fatty acids manifest stimulative and protective effects on intestinal barrier function through the inhibition of NLRP3 inflammasome and autophagy. Cell Physiol Biochem. 2018;49:190–205.
Acknowledgements
We would like to thank the parents and children for participating in the study. We thank the doctors and nursing staffs of these centers for their detailed assessment and dedicated care of these young patients. We also would like to thank Xiaohong Yang, Fang Liu, Dandan Zhang, Rui Fan, Shule Zhang, Qiao Shi, and Mei Feng for their contribution to sample collection.
Funding
This work was supported by the National Key Research and Development Program of China (2016YFC1305302) and the Clinical special project of integrated traditional Chinese and Western medicine in 2019, Shanghai Municipal Health Commission, Shanghai Municipal Administrator of Traditional Chinese Medicine.
Author information
Authors and Affiliations
Contributions
FL: supervision and conceptualization; RC, HW, LC HD, GL, YY, XC, and XF: data curation and supervision; XY: data curation and formal analysis; ZX: formal analysis and writing—original draft.
Corresponding author
Ethics declarations
Conflict of interest
No financial or non-financial benefits have been received or will be received from any party related directly or indirectly to the subject of this article. The authors have no conflict of interest to declare.
Ethical approval
This study was approved by the Ethics Committee of Children’s Hospital of Fudan University ([2019]210). The guardians of the children provided written informed consent before information and sample collection.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Xu, ZR., Yuan, XX., Chen, RM. et al. Association between new onset type 1 diabetes and real-world antibiotics and neonicotinoids’ exposure-related gut microbiota perturbation. World J Pediatr 18, 671–679 (2022). https://doi.org/10.1007/s12519-022-00589-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12519-022-00589-3