Abstract
Background
Few studies have investigated the effects of air pollutants on children with acute bronchitis. This study aimed to explore the acute effects of four air pollutants [fine particulate matter (PM2.5), inhalable particulate matter (PM10), sulfur dioxide (SO2), and nitrogen dioxide (NO2)] on the daily number of children admitted to the hospital for acute bronchitis in Sichuan Province, China.
Methods
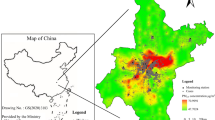
The 49,975 records of hospitalized children with acute bronchitis from medical institutions in nine cities/prefectures, Sichuan Province, China, as well as the simultaneous meteorological data and air pollution data from 183 monitoring sites, were collected from 1 January 2017 to 31 December 2018. A generalized additive model was adopted to analyze the exposure–response and lag effects of hospitalizations of children with acute bronchitis to air pollutants. Stratified analyses were conducted based on sex, age, and season.
Results
The single-pollutant model showed that a 10 µg/m3 increase at lag07 of PM2.5, PM10, SO2, and NO2 corresponded to an increase of 1.23% [95% confidence interval (CI) 0.21–2.26%], 1.33% (95% CI 0.62–2.05%), 23.52% (95% CI 11.52–36.81%), and 12.47% (95% CI 8.46–16.64%) in daily hospitalizations for children with acute bronchitis, respectively. Children aged 0–2 were more prone to PM2.5 (P < 0.05). Interestingly, the effects were stronger in the warm season than in transition seasons and the cool season for PM2.5 and PM10 (P < 0.05).
Conclusion
The higher daily average concentrations of four pollutants in Sichuan Province can result in an increased number of children hospitalized for acute bronchitis.



Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Cohen AJ, Brauer M, Burnett R, Anderson HR, Frostad J, Estep K, et al. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the global burden of diseases study 2015. Lancet. 2017;389:1907–18.
Liu C, Chen R, Sera F, Vicedo-Cabrera AM, Guo Y, Tong S, et al. Ambient particulate air pollution and daily mortality in 652 cities. N Engl J Med. 2019;381:705–15.
GBD 2019 risk factors collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet. 2020;396:1223–49.
World Health Organization. Air pollution and child health: prescribing clean air. https://www.who.int/publications/i/item/air-pollution-and-child-health. Accessed 7 July 2021.
Zhou H, Wang T, Zhou F, Liu Y, Zhao W, Wang X, et al. Ambient air pollution and daily hospital admissions for respiratory disease in children in Guiyang, China. Front Pediatr. 2019;7:400.
Mudway IS, Dundas I, Wood HE, Marlin N, Jamaludin JB, Bremner SA, et al. Impact of London’s low emission zone on air quality and children’s respiratory health: a sequential annual cross-sectional study. Lancet Public Health. 2019;4:e28-40.
Lee JY, Kim H. Ambient air pollution-induced health risk for children worldwide. Lancet Planet Health. 2018;2:e285–6.
Leung SY, Lau SYF, Kwok KL, Mohammad KN, Chan PKS, Chong KC. Short-term association among meteorological variation, outdoor air pollution and acute bronchiolitis in children in a subtropical setting. Thorax. 2021;76:360–9.
Liang Z, Meng Q, Yang Q, Chen N, You C. Size-specific particulate matter associated with acute lower respiratory infection outpatient visits in children: a counterfactual analysis in Guangzhou. China Front Public Health. 2021;9:789542.
Hua J, Yin Y, Peng L, Du L, Geng F, Zhu L. Acute effects of black carbon and PM2.5 on children asthma admissions: a time-series study in a Chinese city. Sci Total Env. 2014;481:433–8.
Kampa M, Castanas E. Human health effects of air pollution. Env Pollut. 2008;151:362–7.
Arias-Pérez RD, Taborda NA, Gómez DM, Narvaez JF, Porras J, Hernandez JC. Inflammatory effects of particulate matter air pollution. Env Sci Pollut Res Int. 2020;27:42390–404.
Feng H, Rong J, Pei K, Jing F, Zhuang Q, Lu T, et al. A systematic review protocol of Tuina for children with acute bronchitis: a protocol for systematic review. Med (Baltimore). 2020;99:e18899.
Global health data exchange. The global incidence of acute lower respiratory infections in children aged 0–14. http://ghdx.healthdata.org/gbd-results-tool. Accessed 4 July 2021.
World Health Organization. Distribution of causes of death among children aged < 5 years (%). https://www.who.int/data/gho/data/indicators/indicator-details/GH-O/distribution-of-causes-of-death-among-children-aged-5-years-(-). Accessed 4 July 2021.
Wang Y, Liu Z, Yang L, Zhou J, Li J, Liao HL, et al. Sepsis-related hospital admissions and ambient air pollution: a time series analysis in 6 Chinese cities. BMC Public Health. 2021;21:1182.
Yong ZL, Luo L, Li CY, Gu YH, Wu SZ. Excessive admission burden of unspecified asthma attributable to air pollution: an evidence from Chengdu in China. Air Qual Atmos Health. 2021;14:1133–47.
Weinmayr G, Romeo E, De Sario M, Weiland SK, Forastiere F. Short-term effects of PM10 and NO2 on respiratory health among children with asthma or asthma-like symptoms: a systematic review and meta-analysis. Env Health Perspect. 2010;118:449–57.
Xiong Q, Zhao W, Gong Z, Zhao W, Tang T. Fine particulate matter pollution and hospital admissions for respiratory diseases in Beijing, China. Int J Env Res Public Health. 2015;12:11880–92.
Wu Z, Chen X, Li G, Tian L, Wang Z, Xiong X, et al. Attributable risk and economic cost of hospital admissions for mental disorders due to PM2.5 in Beijing. Sci Total Env. 2020;718:137274.
Altman DG, Bland JM. Interaction revisited: the difference between two estimates. BMJ. 2003;326:219.
Liu Y, Pan J, Zhang H, Shi C, Li G, Peng Z, et al. Short-term exposure to ambient air pollution and asthma mortality. Am J Respir Crit Care Med. 2019;200:24–32.
Zhu L, Ge X, Chen Y, Zeng X, Pan W, Zhang X, et al. Short-term effects of ambient air pollution and childhood lower respiratory diseases. Sci Rep. 2017;7:4414.
Li M, Tang J, Yang H, Zhao L, Liu Y, Xu H, et al. Short-term exposure to ambient particulate matter and outpatient visits for respiratory diseases among children: a time-series study in five Chinese cities. Chemosphere. 2021;263:128214.
Halonen JI, Lanki T, Yli-Tuomi T, Kulmala M, Tiittanen P, Pekkanen J. Urban air pollution, and asthma and COPD hospital emergency room visits. Thorax. 2008;63:635–41.
Madureira J, Slezakova K, Silva AI, Lage B, Mendes A, Aguiar L, et al. Assessment of indoor air exposure at residential homes: inhalation dose and lung deposition of PM10, PM2.5 and ultrafine particles among newborn children and their mothers. Sci Total Env. 2020;717:137293.
César ACG, Nascimento LF. Coarse particles and hospital admissions due to respiratory diseases in children. An ecological time series study. Sao Paulo Med J. 2018;136:245–50.
Lv Y, Xu SS, Liu WY, Zhang WH. Research progress on cytotoxic effects of PM2.5 components. Chin Prev Med. 2018;19:313–5 (in Chinese).
Deng X, Zhang F, Rui W, Long F, Wang L, Feng Z, et al. PM2.5-induced oxidative stress triggers autophagy in human lung epithelial A549 cells. Toxicol In Vitro. 2013;27:1762–70.
Pang Y, Huang W, Luo XS, Chen Q, Zhao Z, Tang M, et al. In-vitro human lung cell injuries induced by urban PM2.5 during a severe air pollution episode: variations associated with particle components. Ecotoxicol Env Saf. 2020;206:111406.
Donaldson K, Mills N, MacNee W, Robinson S, Newby D. Role of inflammation in cardiopulmonary health effects of PM. Toxicol Appl Pharm. 2005;207(2 Suppl):483–8.
Chen TM, Gokhale J, Shofer S, Kuschner WG. Outdoor air pollution: nitrogen dioxide, sulfur dioxide, and carbon monoxide health effects. Am J Med Sci. 2007;333:249–56.
Dockery DW, Cunningham J, Damokosh AI, Neas LM, Spengler JD, Koutrakis P, et al. Health effects of acid aerosols on North American children: respiratory symptoms. Env Health Perspect. 1996;104:500–5.
Liu YX. Damage effects of SO2 and its epidemiology and toxicology research. Asian J Ecotoxicol. 2007;2:225–31 (in Chinese).
Gutiérrez-Delgado RI, Barraza-Villarreal A, Escamilla-Núñez MC, Hernández-Cadena L, Cortez-Lugo M, Sly P, et al. Prenatal exposure to VOCs and NOx and lung function in preschoolers. Pediatr Pulmonol. 2020;55:2142–9.
Carey WA, Weaver AL, Mara KC, Clark RH. Inhaled nitric oxide in extremely premature neonates with respiratory distress syndrome. Pediatrics. 2018;141:e20173108.
Li D, Wang JB, Zhang ZY, Shen P, Zheng PW, Jin MJ, et al. Effects of air pollution on hospital visits for pneumonia in children: a 2-year analysis from China. Env Sci Pollut Res Int. 2018;25:10049–57.
Bateson TF, Schwartz J. Children’s response to air pollutants. J Toxicol Env Health A. 2008;71:238–43.
Hua J, Yin Y, Peng L, Du L, Geng F, Zhu L. Acute effects of black carbon and PM2.5 on children asthma admissions: a time-series study in a Chinese city. Sci Total Env. 2014;481:433–8.
Sarnat JA, Brown KW, Schwartz J, Coull BA, Koutrakis P. Ambient gas concentrations and personal particulate matter exposures: implications for studying the health effects of particles. Epidemiology. 2005;16:385–95.
Funding
The authors received financial support from the National Natural Science Foundation of China (No. 72174032), and the research projects of “Xinglin Scholars” Nursery Talent in 2021 Research Plan of Chengdu University of Traditional Chinese Medicine through grants MPRC2021013.
Author information
Authors and Affiliations
Contributions
YH initiated the idea for the study and was involved in writing of the original draft. WJ, YH, JLQ and JL developed the formal analysis and software. LJ was involved in data curation. LY was involved in reviewing and editing. LY was the PI for the fund and designed ideas of research. All the authors participated in revising manuscript according to the comments of reviewers and approved the final report.
Corresponding author
Ethics declarations
Ethical approval
All the procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki. This study was approved by the Ethics Committee of Hospital of Chengdu University of Traditional Chinese Medicine (approval no. 2020KL-001).
Conflict of interest
No financial or non-financial benefits have been received or will be received from any party related directly or indirectly to the subject of this article. The authors have no conflict of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
He, Y., Jiang, W., Liao, JQ. et al. Short-term effects of air pollutants on hospital admissions for acute bronchitis in children: a multi-city time-series study in Southwest China. World J Pediatr 18, 426–434 (2022). https://doi.org/10.1007/s12519-022-00537-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12519-022-00537-1