Abstract
Background
Cystatin C (Cys-C) is an emerging biomarker of renal diseases and its clinical use, particularly for screening the communities affected by chronic kidney disease of unknown etiology (CKDu), is hindered due to the lack of reference intervals (RIs) for diverse ethnic and age groups. The present study aimed to define RIs for urinary Cys-C (uCys-C) for a healthy pediatric population in Sri Lanka and in turn compare the renal function of the residential children in CKDu endemic and non-endemic regions in Sri Lanka.
Methods
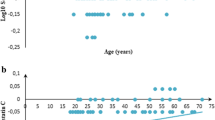
A cross-sectional study was conducted with 850 healthy children (10–17 years) from selected locations for reference interval establishment, while a total of 892 children were recruited for the comparative study. Urine samples were collected and analyzed for Cys-C, creatinine (Cr) and albumin. Cr-adjusted uCys-C levels were partitioned by age, and RIs were determined with quantile regression (2.5th, 50th and 97.5th quantiles) at 90% confidence interval.
Results
The range of median RIs for uCys-C in healthy children was 45.94–64.44 ng/mg Cr for boys and 53.58–69.97 ng/mg Cr for girls. The median (interquartile range) uCys-C levels of children in the CKDu endemic and non-endemic regions were 58.18 (21.8–141.9) and 58.31 (23.9–155.3) ng/mg Cr with no significant difference (P = 0.781). A significant variation of uCys-C was noted in the children across age.
Conclusions
Notably high uCys-C levels were observed in children with elevated proteinuria. Thus, uCys-C could be a potential biomarker in identifying communities at high risk of CKDu susceptibility.



Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available due restrictions under the approval of the ethics review board, but are available from the corresponding author on reasonable request.
References
GBD Chronic Kidney Disease Collaboration. Global, regional, and national burden of chronic kidney disease, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2020;395:709–33.
Agampodi SB, Amarasinghe GS, Naotunna PGCR, Jayasumana CS, Siribaddana SH. Early renal damage among children living in the region of highest burden of chronic kidney disease of unknown etiology (CKDu) in Sri Lanka. BMC Nephrol. 2018;19:115.
Leibler JH, Ramirez-Rubio O, Velázquez JJA, Pilarte DL, Obeid W, Parikh CR, et al. Biomarkers of kidney injury among children in a high-risk region for chronic kidney disease of uncertain etiology. Pediatr Nephrol. 2021;36:387–96.
Ramírez-Rubio O, Amador JJ, Kaufman JS, Weiner DE, Parikh CR, Khan U, et al. Urine biomarkers of kidney injury among adolescents in Nicaragua, a region affected by an epidemic of chronic kidney disease of unknown aetiology. Nephrol Dial Transplant. 2016;31:424–32.
Babich R, Ulrich JC, Ekanayake EMDV, Massarsky A, De Silva PMCS, Manage PM, et al. Kidney developmental effects of metal-herbicide mixtures: implications for chronic kidney disease of unknown etiology. Environ Int. 2020;144:106019.
Groesbeck D, Köttgen A, Parekh R, Selvin E, Schwartz GJ, Coresh J, et al. Age, gender, and race effects on cystatin C levels in US adolescents. Clin J Am Soc Nephrol. 2008;3:1777–85.
Madsen MG, Nørregaard R, Palmfeldt J, Olsen LH, Frøkiær J, Jørgensen TM. Urinary NGAL, cystatin C, β2-microglobulin, and osteopontin significance in hydronephrotic children. Pediatr Nephrol. 2012;27:2099–106.
Laterza OF, Price CP, Scott MG. Cystatin C: an improved estimator of glomerular filtration rate? Clin Chem. 2002;48:699–707.
Newman DJ, Thakkar H, Edwards RG, Wilkie M, White T, Grubb AO, et al. Serum cystatin C measured by automated immunoassay: a more sensitive marker of changes in GFR than serum creatinine. Kidney Int. 1995;47:312–8.
Fan L, Levey AS, Gudnason V, Eiriksdottir G, Andresdottir MB, Gudmundsdottir H, et al. Comparing GFR estimating equations using cystatin C and creatinine in elderly individuals. J Am Soc Nephrol. 2015;26:1982–9.
Gunasekara TDKSC, De Silva PMCS, Herath C, Siribaddana S, Siribaddana N, Jayasumana C, et al. The utility of novel renal biomarkers in assessment of chronic kidney disease of unknown etiology (CKDu): a review. Int J Environ Res Public Health. 2020;17:9522
McWilliam SJ, Antoine DJ, Sabbisetti V, Pearce RE, Jorgensen AL, Lin Y, et al. Reference intervals for urinary renal injury biomarkers KIM-1 and NGAL in healthy children. Biomark Med. 2014;8:1189–97.
U.S. Food and Drug Administration. List of qualified biomarkers. 2021. https://www.fda.gov/drugs/biomarker-qualification-program/list-qualified-biomarkers. Accessed 2 Oct 2021
Mussap M, Plebani M. Biochemistry and clinical role of human cystatin C. Crit Rev Clin Lab Sci. 2004;41:467–550.
Harmoinen A, Ylinen E, Ala-Houhala M, Janas M, Kaila M, Kouri T. Reference intervals for cystatin C in pre- and full-term infants and children. Pediatr Nephrol. 2000;15:105–8.
Herget-Rosenthal S, Feldkamp T, Volbracht L, Kribben A. Measurement of urinary cystatin C by particle-enhanced nephelometric immunoassay: precision, interferences, stability and reference range. Ann Clin Biochem. 2004;41:111–8.
Herget-Rosenthal S, van Wijk JAE, Bröcker-Preuss M, Bökenkamp A. Increased urinary cystatin C reflects structural and functional renal tubular impairment independent of glomerular filtration rate. Clin Biochem. 2007;40:946–51.
Fellström B, Helmersson-Karlqvist J, Lind L, Soveri I, Thulin M, Ärnlöv J, et al. Strong associations between early tubular damage and urinary cytokine, chemokine, and growth factor levels in elderly males and females. J Interferon Cytokine Res. 2021;41:283–90.
van Donge T, Welzel T, Atkinson A, van den Anker J, Pfister M. Age-dependent changes of kidney injury biomarkers in pediatrics. J Clin Pharmacol. 2019;59:S21-32.
Hassan M, Hatata EZ, Al-Arman M, Aboelnaga MM. Urinary cystatin C as a biomarker of early renal dysfunction in type 2 diabetic patients. Diabetes Metab Syndr. 2021;15:102152.
Park MY, Choi SJ, Kim JK, Hwang SD, Lee YW. Urinary cystatin C levels as a diagnostic and prognostic biomarker in patients with acute kidney injury. Nephrology (Carlton). 2013;18:256–62.
Sato Y, Takahashi M, Yanagita M. Pathophysiology of AKI to CKD progression. Semin Nephrol. 2020;40:206–15.
Bökenkamp A, Domanetzki M, Zinck R, Schumann G, Byrd D, Brodehl J. Cystatin C—a new marker of glomerular filtration rate in children independent of age and height. Pediatrics. 1998;101:875–81.
Redmon JH, Levine KE, Lebov J, Harrington J, Kondash AJ. A comparative review: chronic kidney disease of unknown etiology (CKDu) research conducted in Latin America versus Asia. Environ Res. 2021;192:110270.
Orantes-Navarro CM, Herrera-Valdés R, Almaguer-López MA, Brizuela-Díaz EG, Reed NPAMMA, Fuentes-de Morales EJ, et al. Chronic kidney disease in children and adolescents in Salvadoran farming communities: NefroSalva Pediatric Study (2009–2011). MEDICC Rev. 2016;18:15.
Lozano-Kasten F, Sierra-Diaz E, de Jesus Celis-de la Rosa A, Margarita Soto Gutiérrez M, Aarón Peregrina Lucano A, Research Group on Social and Environmental Determinants in Childhood. Prevalence of albuminuria in children living in a rural agricultural and fishing subsistence community in Lake Chapala, Mexico. Int J Environ Res Public Health. 2017;14:1577.
Wu D, Yang H, Luo J, Zhang G, Li S, Wang M, et al. Age- and gender-specific reference values for urine albumin/creatinine ratio in children of southwest China. Clin Chim Acta. 2014;431:239–43.
Sueud T, Hadi NR, Abdulameer R, Jamil DA, Al-Aubaidy HA. Assessing urinary levels of IL-18, NGAL and albumin creatinine ratio in patients with diabetic nephropathy. Diabetes Metab Syndr. 2019;13:564–8.
Takahashi S, Tanaka F, Yonekura Y, Tanno K, Ohsawa M, Sakata K, et al. The urine albumin-creatinine ratio is a predictor for incident long-term care in a general population. PLoS One. 2018;13: e0195013.
Bellera CA, Hanley JA. A method is presented to plan the required sample size when estimating regression-based reference limits. J Clin Epidemiol. 2007;60:610–5.
Lim JU, Lee JH, Kim JS, Hwang YI, Kim TH, Lim SY, et al. Comparison of World Health Organization and Asia-Pacific body mass index classifications in COPD patients. Int J Chron Obstruct Pulmon Dis. 2017;12:2465–75.
Arya R, Antonisamy B, Kumar S. Sample size estimation in prevalence studies. Indian J Pediatr. 2012;79:1482–8.
Henny J. The IFCC recommendations for determining reference intervals: strengths and limitations. J Lab Med. 2009;33:45–51.
van Donge T, Staub E, Atkinson A, Gotta V, van den Anker J, Risch L, et al. Age appropriate reference intervals for eight kidney function and injury markers in infants, children and adolescents. Clin Chem Lab Med. 2021;59:373–82.
Bennett MR, Nehus E, Haffner C, Ma Q, Devarajan P. Pediatric reference ranges for acute kidney injury biomarkers. Pediatr Nephrol. 2015;30:677–85.
Cai T, Karlaftis V, Hearps S, Matthews S, Burgess J, Monagle P, et al. Reference intervals for serum cystatin C in neonates and children 30 days to 18 years old. Pediatr Nephrol. 2020;35:1959–66.
Marmarinos A, Garoufi A, Panagoulia A, Dimou S, Drakatos A, Paraskakis I, et al. Cystatin-C levels in healthy children and adolescents: influence of age, gender, body mass index and blood pressure. Clin Biochem. 2016;49:150–3.
Daly CH, Liu X, Grey VL, Hamid JS. A systematic review of statistical methods used in constructing pediatric reference intervals. Clin Biochem. 2013;46:1220–7.
Acknowledgements
The authors would like to thank all the participants children who participated in the study, parents, academic and nonacademic staff members of the schools, government authorities school principals, teachers, and parents for their valuable support.
Funding
This research was funded by the Accelerating Higher Education Expansion and Development (AHEAD) Operation of the Ministry of Higher Education funded by the World Bank (No. AHEAD DOR 02/40).
Author information
Authors and Affiliations
Contributions
SPMMA contributed to data curation, formal analysis, investigation, software, visualization, writing of the original draft, review and editing. DSPMCS contributed to conceptualization, data curation, formal analysis, funding acquisition, investigation, methodology, project administration, resources, software, supervision, validation, review and editing. GTDKSC contributed to data curation, formal analysis, investigation, software, visualization, writing of the original draft, review and editing. GSD contributed to data curation, formal analysis, and investigation. PRAI contributed to data curation and investigation. HC, JSS and CEPS contributed to resources, supervision, validation, review and editing. JN contributed to conceptualization, project administration, resources, supervision, validation, review and editing.
Corresponding author
Ethics declarations
Ethical approval
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Ethics Review Committee of the Faculty of Medicine, University of Ruhuna (reference no: 2020.P.124; date: 29.01.2021). Informed consent to participate in the study have been obtained from the children and their parents.
Conflict of interest
No financial or non-financial benefits have been received or will be received from any party related directly or indirectly to the subject of this article. None of the authors was involved in the journal’s review of, or decisions related to, this manuscript. The authors have no conflict of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sandamini, P.M.M.A., De Silva, P.M.C.S., Gunasekara, T.D.K.S.C. et al. Urinary cystatin C: pediatric reference intervals and comparative assessment as a biomarker of renal injury among children in the regions with high burden of CKDu in Sri Lanka. World J Pediatr 18, 196–205 (2022). https://doi.org/10.1007/s12519-022-00513-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12519-022-00513-9