Abstract
Background
The aim of this study was to explore the associations between the aspartate aminotransferase-to-alanine aminotransferase ratio (AST/ALT) and coronary artery lesions (CALs) among patients with Kawasaki disease (KD).
Methods
Medical records of KD patients presenting to a single center between January 2019 and December 2020 were retrospectively collected and analyzed. Univariate, multivariable-adjusted analyses, subgroup analyses, restricted cubic spline test, and fitted curves were used to evaluate the associations between AST/ALT and CALs.
Results
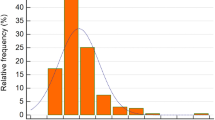
A total of 831 patients were enrolled, of which 201 (24.2%) had CALs on admission and 21 (2.5%) developed CALs de novo after intravenous immunoglobulin (IVIG). Multivariable-adjusted analyses models revealed that a lower AST/ALT was associated with an increased risk of CALs on admission when AST/ALT was a continuous variable (P = 0.007) and when it was a categorical variable (P for trend = 0.004). Each unit increase in AST/ALT was associated with a 22% lower risk of CALs on admission (odds ratio = 0.78, 95% confidence interval 0.65–0.94). A negative linear relationship was noted between AST/ALT and the risk of CALs on admission in both observed and fitted models. However, such associations were not observed in AST/ALT and CALs de novo after IVIG. None of the variables significantly modified the association between AST/ALT and CALs on admission and CALs de novo after IVIG (P > 0.05).
Conclusion
Our findings suggested that AST/ALT was a risk factor of CALs, but was not associated with progressive CALs.



Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
McCrindle BW, Rowley AH, Newburger JW, Burns JC, Bolger AF, Gewitz M, et al. Diagnosis, treatment, and long-term management of Kawasaki disease: a scientific statement for health professionals from the American Heart Association. Circulation. 2017;135:e927–99.
Xie LP, Yan WL, Huang M, Huang MR, Chen S, Huang GY, et al. Epidemiologic features of Kawasaki disease in Shanghai from 2013 through 2017. J Epidemiol. 2020;30:429–35.
Kuwabara M, Yashiro M, Kotani K, Tsuboi S, Ae R, Nakamura Y, et al. Cardiac lesions and initial laboratory data in Kawasaki disease: a nationwide survey in Japan. J Epidemiol. 2015;25:189–93.
Tacke CE, Breunis WB, Pereira RR, Breur JM, Kuipers IM, Kuijpers TW. Five years of Kawasaki disease in the Netherlands: a national surveillance study. Pediatr Infect Dis J. 2014;33:793–7.
Callinan LS, Tabnak F, Holman RC, Maddox RA, Kim JJ, Schonberger LB, et al. Kawasaki syndrome and factors associated with coronary artery abnormalities in California. Pediatr Infect Dis J. 2012;31:894–8.
Tomita Y, Fukaya T, Yamaura Y, Tsujiguchi R, Muratani H, Shimaya M. Implications of hepatic dysfunction in Kawasaki disease: time-related changes in aspartate aminotransferase, alanine aminotransferase, total bilirubin, and C-reactive protein levels. Pediatr Investig. 2019;3:19–26.
Mammadov G, Liu HH, Chen WX, Fan GZ, Li RX, Liu FF, et al. Hepatic dysfunction secondary to Kawasaki disease: characteristics, etiology and predictive role in coronary artery abnormalities. Clin Exp Med. 2020;20:21–30.
Eladawy M, Dominguez SR, Anderson MS, Glodé MP. Abnormal liver panel in acute Kawasaki disease. Pediatr Infect Dis J. 2011;30:141–4.
Yokoyama M, Watanabe T, Otaki Y, Takahashi H, Arimoto T, Shishido T, et al. Association of the aspartate aminotransferase to alanine aminotransferase ratio with BNP level and cardiovascular mortality in the general population: the Yamagata study 10-year follow-up. Dis Mark. 2016;2016:4857917.
Wang J, Li J, Ren Y, Shi H, Rong X, Zhang X, et al. Association between alanine aminotransferase/aspartate aminotransferase ratio (AST/ALT ratio) and coronary artery injury in children with Kawasaki disease. Cardiol Res Pract. 2020;2020:8743548.
Tang Y, Yan W, Sun L, Xu Q, Ding Y, Lv H. Coronary artery aneurysm regression after Kawasaki disease and associated risk factors: a 3-year follow-up study in East China. Clin Rheumatol. 2018;37:1945–51.
Ae R, Abrams JY, Maddox RA, Schonberger LB, Nakamura Y, Kuwabara M, et al. Outcomes in Kawasaki disease patients with coronary artery abnormalities at admission. Am Heart J. 2020;225:120–8.
Dallaire F, Dahdah N. New equations and a critical appraisal of coronary artery Z scores in healthy children. J Am Soc Echocardiogr. 2011;24:60–74.
De Ritis F, Coltorti M, Giusti G. An enzymic test for the diagnosis of viral hepatitis: the transaminase serum activities. 1957. Clin Chim Acta. 2006;369:148–52.
Yilmaz M, Sahin Y, Ates HA, Hacibey I, Cil G. De Ritis ratio: how effectively can we use in bladder cancer management? Biomark Med. 2020;14:1453–60.
Su S, Liu L, Li C, Zhang J, Li S. Prognostic role of pretreatment De Ritis ratio (aspartate transaminase/alanine transaminase ratio) in urological cancers: a systematic review and meta-analysis. Front Oncol. 2020;10:1650.
Kang M, Shin SJ, Sung HH, Jeon HG, Jeong BC, Jeon SS, et al. Clinical significance of pre-to-postoperative dynamics of aspartate transaminase/alanine transaminase ratio in predicting the prognosis of renal cell carcinoma after surgical treatment. Dis Mark. 2020;2020:8887605.
Mori K, Janisch F, Mostafaei H, Kimura S, Lysenko I, Karakiewicz PI, et al. Prognostic role of preoperative De Ritis ratio in upper tract urothelial carcinoma treated with nephroureterectomy. Urol Oncol. 2020;38:e17-24.
Nam JS, Kim WJ, An SM, Choi DK, Chin JH, Lee EH, et al. Age-dependent relationship between preoperative serum aminotransferase and mortality after cardiovascular surgery. Aging (Albany NY). 2019;11:9060–74.
Liu Z, Que S, Xu J, Peng T. Alanine aminotransferase-old biomarker and new concept: a review. Int J Med Sci. 2014;11:925–35.
Le Couteur DG, Blyth FM, Creasey HM, Handelsman DJ, Naganathan V, Sambrook PN, et al. The association of alanine transaminase with aging, frailty, and mortality. J Gerontol A Biol Sci Med Sci. 2010;65:712–7.
Cheng F, Kang L, Zhang F, Ma H, Wang X, Dong Y, et al. Analysis of hyperbilirubinemia in patients with Kawasaki disease. Medicine (Baltimore). 2020;99:e21974.
Muto T, Nakamura N, Masuda Y, Numoto S, Kodama S, Miyamoto R, et al. Serum free carnitine levels in children with Kawasaki disease. Pediatr Int. 2021. https://doi.org/10.1111/ped.14849.
Tang Y, Yan W, Sun L, Huang J, Qian W, Ding Y, et al. Prediction of intravenous immunoglobulin resistance in Kawasaki disease in an East China population. Clin Rheumatol. 2016;35:2771–6.
Egami K, Muta H, Ishii M, Suda K, Sugahara Y, Iemura M, et al. Prediction of resistance to intravenous immunoglobulin treatment in patients with Kawasaki disease. J Pediatr. 2006;149:237–40.
Kobayashi T, Inoue Y, Takeuchi K, Okada Y, Tamura K, Tomomasa T, et al. Prediction of intravenous immunoglobulin unresponsiveness in patients with Kawasaki disease. Circulation. 2006;113:2606–12.
Sano T, Kurotobi S, Matsuzaki K, Yamamoto T, Maki I, Miki K, et al. Prediction of non-responsiveness to standard high-dose gamma-globulin therapy in patients with acute Kawasaki disease before starting initial treatment. Eur J Pediatr. 2007;166:131–7.
Nikolaou M, Parissis J, Yilmaz MB, Seronde MF, Kivikko M, Laribi S, et al. Liver function abnormalities, clinical profile, and outcome in acute decompensated heart failure. Eur Heart J. 2013;34:742–9.
Niu L, An XJ, Fu MY, He XH, Wang QW. Observation of Kawasaki disease-related indexes and the study of relationship between myocardial enzyme changes and coronary artery lesions. Eur Rev Med Pharmacol Sci. 2015;19:4407–10.
Anjani G, Deglurkar R, Pilania RK, Chaudhary H, Vaiphei K, Vignesh P, et al. Fulminant acute liver failure as an unusual presentation of Kawasaki disease. Scand J Rheumatol. 2021;50:327–9.
Amano S, Hazama F, Hamashima Y. Pathology of Kawasaki disease: II. Distribution and incidence of the vascular lesions. Jpn Circ J. 1979;43:741–8.
Pilania RK, Arora K, Gupta A, Vignesh P, Suri D, Singh S. A 5-year-old boy with Kawasaki disease shock syndrome, myocarditis and macrophage activation syndrome. J Paediatr Child Health. 2021;57:1312–5.
Harada M, Yokouchi Y, Oharaseki T, Matsui K, Tobayama H, Tanaka N, et al. Histopathological characteristics of myocarditis in acute-phase Kawasaki disease. Histopathology. 2012;61:1156–67.
Chuang GT, Tsai IJ, Lin MT, Chang LY. Acute kidney injury in patients with Kawasaki disease. Pediatr Res. 2016;80:224–7.
Funding
This work was financially supported by the National Natural Science Foundation of China (Nos. 81870365, 81700439, and 81801559), Gusu Health Personnel Training Project (Nos. GSWS2019048 and 2020054), Suzhou Science and Technology Development Plan Project (Nos. SYS2019084 and SS202066), and Jiangsu Province Key Medical Young Talents (No. QNRC 2016765).
Author information
Authors and Affiliations
Contributions
CL and TYJ contributed equally to this study as first co-authors. CL contributed to investigation, methodology and writing original draft. TYJ contributed to conceptualization, data curation, funding acquisition, reviewing, and editing. GM contributed to investigation and methodology. QWG, MJ, and XQQ contributed to investigation, and project administration. LHT contributed to conceptualization, funding acquisition and supervision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
The Institutional Review Board of Children’s Hospital of Soochow University approved this study (No. 2021CS086).
Conflict of interest
No financial or non-financial benefits have been received or will be received from any party related directly or indirectly to the subject of this article. The authors have no conflict of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
12519_2021_479_MOESM1_ESM.tif
Supplementary Fig. 1 Receiver-operator characteristic curves for the prediction of CALs on admission. The baseline predictors are age, sex, CRP, albumin, total bilirubin, delayed IVIG treatment after the 10th day, and IKD. AST aspartate aminotransferase, ALT alanine aminotransferase, CALs coronary artery lesions, IKD incomplete Kawasaki disease, IVIG intravenous immunoglobulin, CRP C-reactive protein
12519_2021_479_MOESM2_ESM.tif
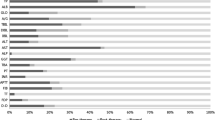
Supplementary Fig. 2 Stratified analyses by possible modifications for the association between AST/ALT and CALs on admission. Adjusted for: age, sex, CRP, albumin, total bilirubin, delayed IVIG treatment after the 10th day, and IKD. In each case, the model is not adjusted for the stratification variable. A total of 824 patients were enrolled in the analysis. AST aspartate aminotransferase, ALT alanine aminotransferase, CALs coronary artery lesions, IKD incomplete Kawasaki disease, IVIG intravenous immunoglobulin, CRP C-reactive protein, CI confidence interval, OR odds ratio
12519_2021_479_MOESM3_ESM.docx
Supplementary Fig. 3 Stratified analyses by possible modifications for the association between AST/ALT and CALs de novo after IVIG. Adjusted for: age, sex, CRP, albumin, total bilirubin, delayed IVIG treatment after the 10th day, and IKD. In each case, the model is not adjusted for the stratification variable. A total of 794 patients were enrolled in the analysis. AST aspartate aminotransferase, ALT alanine aminotransferase, CALs coronary artery lesions, IKD incomplete Kawasaki disease, IVIG intravenous immunoglobulin, CRP C-reactive protein, CI confidence interval, OR odds ratio
Rights and permissions
About this article
Cite this article
Cao, L., Tang, YJ., Gang, M. et al. AST-to-ALT ratio and coronary artery lesions among patients with Kawasaki disease. World J Pediatr 17, 659–668 (2021). https://doi.org/10.1007/s12519-021-00479-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12519-021-00479-0