Abstract
Background
There are limited studies comparing budesonide inhalation suspension (BIS) with montelukast in real-world settings where treatment adherence and persistency may be suboptimal. This real-world study aims to investigate the control effectiveness of montelukast or BIS as a monotherapy in Chinese children with mild asthma.
Methods
Data were derived from a retrospective questionnaire-based analysis of 2‒14-year-old children with mild persistent asthma, who received either 500 µg of BIS (n = 153) or 4‒5 mg of montelukast (n = 240) once daily. The indicators of asthma control, the Asthma Control Test (ACT)/Childhood ACT (C-ACT) score, and the asthma-related medical costs were assessed. The differences between the two groups were compared using an unpaired t-test (normally distributed), Mann–Whitney U test (non-normally distributed) or chi-squared test (categorical variables).
Results
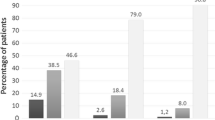
Medication compliance in the past 3-month period was better in the montelukast group than in the BIS group (P = 0.042). The montelukast group exhibited better asthma control in the past 4-week period, including lower percentages of asthmatic children with symptoms more than twice a week (P = 0.021), had night waking or night coughing (P = 0.022), or required reliever medication more than twice a week (P < 0.001). The montelukast group had a lower percentage of children with an ACT/C-ACT score ≤ 19 (P = 0.015). Caregivers reported a significantly better exercise tolerance in the children who received montelukast vs. BIS in the past 12 months (P < 0.001). Significantly higher medical expenditures attributable to asthma in the past 12 months were observed in the BIS group vs. montelukast group (P < 0.001).
Conclusion
Both treatments provided acceptable overall asthma control in children with mild persistent asthma; however, more reliever medication and more medical expenditures attributable to asthma were needed for BIS vs. montelukast in real-world settings, where factors such as compliance were also taken into account.

Similar content being viewed by others
Data availability
The datasets generated and analysed during the current study are available from the corresponding author on reasonable request.
References
Global Initiative for Asthma (GINA). 2019 GINA report, global strategy for asthma management and prevention. Available at: https://ginasthma.org/. Accessed 23 Mar 2020.
Pearce N, Ait-Khaled N, Beasley R, Mallol J, Keil U, Mitchell E, et al. Worldwide trends in the prevalence of asthma symptoms: phase III of the International Study of Asthma and Allergies in Childhood (ISAAC). Thorax. 2007;62:758–66.
Chen YZ, National Cooperation Group On Childhood Asthma. A nationwide survey in China on prevalence of asthma in urban children. Chinese J Pediatr. 2003;41:123–7.
National Cooperative Group on Childhood Asthma, Institute of Environmental Health and Related Product Safety, Chinese Center for Disease Control and Prevention, Chinese Center for Disease Control and Prevention. Third nationwide survey of childhood asthma in urban areas of China. Chin J Pediatr. 2013;51:729–35.
Guo X, Li Z, Ling W, Long J, Su C, Li J, et al. Epidemiology of childhood asthma in mainland China (1988–2014): a meta-analysis. Allergy Asthma Proc. 2018;39:15–29.
Montuschi P. Pharmacotherapy of patients with mild persistent asthma: strategies and unresolved issues. Front Pharmacol. 2011;2:35.
Navaratnam P, Friedman HS, Urdaneta E. The impact of adherence and disease control on resource use and charges in patients with mild asthma managed on inhaled corticosteroid agents. Patient Prefer Adherence. 2010;4:197–205.
Ducharme FM, Noya FJ, Allen-Ramey FC, Maiese EM, Gingras J, Blais L. Clinical effectiveness of inhaled corticosteroids versus montelukast in children with asthma: prescription patterns and patient adherence as key factors. Curr Med Res Opin. 2012;28:111–9.
Klok T, Kaptein AA, Duiverman EJ, Brand PL. It’s the adherence, stupid (that determines asthma control in preschool children)! Eur Respir J. 2014;43:783–91.
Fitzpatrick AM, Kir T, Naeher LP, Fuhrman SC, Hahn K, Teague WG. Tablet and inhaled controller medication refill frequencies in children with asthma. J Pediatr Nurs. 2009;24:81–9.
Subspecialty Group of Respiratory Diseases, Society of Pediatrics, Chinese Medical Association, Editorial Board, Chinese Journal of Pediatrics. Guideline for the diagnosis and optimal management of asthma in children (2016). Chin J Pediatr. 2016;54:167–81.
Castro-Rodriguez JA, Rodrigo GJ. The role of inhaled corticosteroids and montelukast in children with mild-moderate asthma: results of a systematic review with meta-analysis. Arch Dis Child. 2010;95:365–70.
Hon KL, Leung TF, Leung AK. Clinical effectiveness and safety of montelukast in asthma. What are the conclusions from clinical trials and meta-analyses? Drug Des Devel Ther. 2014;8:839–50.
Szefler SJ, Baker JW, Uryniak T, Goldman M, Silkoff PE. Comparative study of budesonide inhalation suspension and montelukast in young children with mild persistent asthma. J Allergy Clin Immunol. 2007;120:1043–50.
Shah MB, Gohil J, Khapekar S, Dave J. Montelukast versus budesonide as a first line preventive therapy in mild persistent asthma in 2–18 y. Indian J Pediatr. 2014;81:655–9.
Xiang L, Zhao J, Zheng Y, Liu H, Hong J, Bao Y, et al. Uncontrolled asthma and its risk factors in Chinese children: a cross-sectional observational study. J Asthma. 2016;53:699–706.
Schatz M, Sorkness CA, Li JT, Marcus P, Murray JJ, Nathan RA, et al. Asthma control test: reliability, validity, and responsiveness in patients not previously followed by asthma specialists. J Allergy Clin Immunol. 2006;117:549–56.
Bousquet J, Khaltaev N, Cruz AA, Denburg J, Fokkens WJ, Togias A, et al. Allergic Rhinitis and its Impact on Asthma (ARIA) 2008 update (in collaboration with the World Health Organization, GA2 LEN and AllerGen). Allergy. 2008;63(Suppl 86):8–160.
Zhou X, Ding FM, Lin JT, Yin KS. Validity of asthma control test for asthma control assessment in Chinese primary care settings. Chest. 2009;135:904–10.
Nguyen VN, Chavannes N, Le LT, Price D. The Asthma Control Test (ACT) as an alternative tool to Global Initiative for Asthma (GINA) guideline criteria for assessing asthma control in Vietnamese outpatients. Prim Care Respir J. 2012;21:85–9.
Liu AH, Zeiger R, Sorkness C, Mahr T, Ostrom N, Burgess S, et al. Development and cross-sectional validation of the Childhood Asthma Control Test. J Allergy Clin Immunol. 2007;119:817–25.
Leung TF, Ko FW, Sy HY, Wong E, Li CY, Yung E, et al. Identifying uncontrolled asthma in young children: clinical scores or objective variables? J Asthma. 2009;46:130–5.
Ostrom NK, Decotiis BA, Lincourt WR, Edwards LD, Hanson KM, Carranza Rosenzweig JR, et al. Comparative efficacy and safety of low-dose fluticasone propionate and montelukast in children with persistent asthma. J Pediatr. 2005;147:213–20.
Sorkness CA, Lemanske RF Jr, Mauger DT, Boehmer SJ, Chinchilli VM, Martinez FD, et al. Long-term comparison of 3 controller regimens for mild-moderate persistent childhood asthma: the Pediatric Asthma Controller Trial. J Allergy Clin Immunol. 2007;119:64–72.
Zeiger RS, Szefler SJ, Phillips BR, Schatz M, Martinez FD, Chinchilli VM, et al. Response profiles to fluticasone and montelukast in mild-to-moderate persistent childhood asthma. J Allergy Clin Immunol. 2006;117:45–52.
Rand C, Bilderback A, Schiller K, Edelman JM, Hustad CM, Zeiger RS. Adherence with montelukast or fluticasone in a long-term clinical trial: results from the mild asthma montelukast versus inhaled corticosteroid trial. J Allergy Clin Immunol. 2007;119:916–23.
Szefler SJ, Fitzgerald DA, Adachi Y, Doull IJ, Fischer GB, Fletcher M, et al. A worldwide charter for all children with asthma. Pediatr Pulmonol. 2020;55:1282–92.
Leynaert B, Neukirch F, Demoly P, Bousquet J. Epidemiologic evidence for asthma and rhinitis comorbidity. J Allergy Clin Immunol. 2000;106:S201–5.
Pinart M, Benet M, Annesi-Maesano I, von Berg A, Berdel D, Carlsen KC, et al. Comorbidity of eczema, rhinitis, and asthma in IgE-sensitised and non-IgE-sensitised children in MeDALL: a population-based cohort study. Lancet Respir Med. 2014;2:131–40.
de Groot EP, Duiverman EJ, Brand PL. Comorbidities of asthma during childhood: possibly important, yet poorly studied. Eur Respir J. 2010;36:671–8.
Acknowledgements
The authors would like to thank all of the patients and investigators for their participation to achieve this study goal. Qi Zhong helped design the research. Lin Chen helped explain the data. Both are employees of MSD China, Shanghai, China. Editorial assistance with the preparation of this article was provided by Medjaden Bioscience Limited. This assistance was supported by MSD China, Shanghai, China.
Funding
This work was supported by MSD China, Shanghai, China (grant number: 50146).
Author information
Authors and Affiliations
Contributions
ZC and DZ contributed equally to this paper. JH conceived and designed research; JH collected data and conducted research; DZ and LX analyzed and interpreted data; ZC wrote the initial paper; ZC, DZ, LX and JH revised the paper. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
This study was approved by the Ethics Committee of the Beijing Children’s Hospital, Capital Medical University (approval number: 2012-70). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Written informed consent was obtained from all individual participant’s guardians included in the study.
Conflict of interest
None of the authors declare any conflict of interest in this study. Authors Zhimin Chen and Jianguo Hong are members of the Editorial Board for the World Journal of Pediatrics. The paper was handled by the other Editor and has undergone a rigorous peer-review process. Authors Zhimin Chen and Jianguo Hong were not involved in the journal’s review of, or decisions related to, this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chen, ZM., Zhao, DY., Xiang, L. et al. Treatment of pediatric mild persistent asthma with low-dose budesonide inhalation suspension vs. montelukast in China. World J Pediatr 17, 619–625 (2021). https://doi.org/10.1007/s12519-021-00464-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12519-021-00464-7