Abstract
Background
The interaction of adropin, glucagon-like peptide-2 (GLP2), angiopoietin-like protein 4 (ANGPTL4), and with childhood obesity and glucose metabolism is inconsistent. This study is to evaluate the association of the three cytokines and glucose homeostasis.
Methods
This was a cross-sectional study of children with obesity ranging from 5 to 14 years compared to age- and sex-matched children of normal weight. Fasting plasma glucose (FPG), oral glucose tolerance test 2-hour plasma glucose (OGTT2hPG), and insulin (INS) were measured, and serum adropin, GLP2, and ANGPTL4 levels were measured by enzyme-linked immunosorbent assay. The body mass index (BMI), BMI-Z scores, waist-to-hip ratio (WHR), and homeostasis model assessment of insulin resistance (HOMA-IR) were calculated.
Results
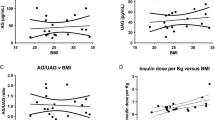
Thirty-nine children (9.70 ± 1.71 years, 18 females) with obesity and 29 normal weight children (8.98 ± 1.98 years, 16 females) were assessed. The levels of INS, HOMA-IR and GLP2 of the obesity group were significantly higher than the controls (P < 0.05). Pearson correlation analysis showed that serum GLP2 was positively associated with WHR, FPG, and OGTT2hPG, and adropin was negatively associated with BMI, BMI-Z, WHR, INS, and HOMA-IR (all P < 0.05). Furthermore, GLP2 were negatively associated with adropin and ANGPTL4 (both P < 0.05). By binary logistic regression, adropin and GLP2 were found to be independent markers of obesity. Multiple linear regression showed that GLP2 was associated with OGTT2hPG, and adropin was associated with INS and HOMA-IR (all P < 0.05).
Conclusions
Obese children had elevated GLP2 concentrations, and adropin and GLP2 associated with both childhood obesity and glucose homeostasis. Furthermore, there may be a physiologic interplay between adropin and GLP2 in obese children.


Similar content being viewed by others
References
Ogden CL, Fryar CD, Hales CM, Carroll MD, Aoki Y, Freedman DS. Differences in obesity prevalence by demographics and urbanization in US children and adolescents, 2013–2016. JAMA. 2018;319:2410–8.
Saltiel AR. New therapeutic approaches for the treatment of obesity. Sci Transl Med. 2016;8:323rv2.
Drucker DJ, Habener JF, Holst JJ. Discovery, characterization, and clinical development of the glucagon-like peptides. J Clin Investig. 2017;127:4217–27.
Baldassano S, Amato A, Mulè F. Influence of glucagon-like peptide 2 on energy homeostasis. Peptides. 2016;86:1–5.
Barja-Fernandez S, Moreno-Navarrete JM, Folgueira C, Xifra G, Sabater M, Castelao C, et al. Plasma ANGPTL-4 is associated with obesity and glucose tolerance: cross-sectional and longitudinal findings. Mol Nutr Food Res. 2018;62:e1800060.
Sadeghabadi ZA, Nourbakhsh M, Alaee M, Larijani B, Razzaghy-Azar M. Peroxisome proliferator-activated receptor gamma expression in peripheral blood mononuclear cells and angiopoietin-like protein 4 levels in obese children and adolescents. J Endocrinol Invest. 2018;41:241–7.
Stevens JR, Kearney ML, St-Onge MP, Stanhope KL, Havel PJ, Kanaley JA, et al. Inverse association between carbohydrate consumption and plasma adropin concentrations in humans. Obesity (Silver Spring). 2016;24:1731–40.
Chang JB, Chu NF, Lin FH, Hsu JT, Chen PY. Relationship between plasma adropin levels and body composition and lipid characteristics amongst young adolescents in Taiwan. Obes Res Clin Pract. 2018;12(Suppl 2):101–7.
Li H, Zong XN, Ji CY, Mi J. Body mass index cut-offs for overweight and obesity in Chinese children and adolescents aged 2–18 years. Zhonghua Liu Xing Bing Xue Za Zhi. 2010;31:616–20 (in Chinese).
Li H, Ji CY, Zong XN, Zhang YQ. Height and weight standardized growth charts for Chinese children and adolescents aged 0 to 18 years. Zhonghua Er Ke Za Zhi. 2009;47:487–92 (in Chinese).
Vegiopoulos A, Rohm M, Herzig S. Adipose tissue: between the extremes. EMBO J. 2017;36:1999–2017.
Amato A, Baldassano S, Mulè F. GLP2: an underestimated signal for improving glycaemic control and insulin sensitivity. J Endocrinol. 2016;229:R57–66.
Baldassano S, Rappa F, Amato A, Cappello F, Mulè F. GLP-2 as beneficial factor in the glucose homeostasis in mice fed a high fat diet. J Cell Physiol. 2015;230:3029–36.
Baldassano S, Amato A, Caldara GF, Mulè F. Glucagon-like peptide-2 treatment improves glucose dysmetabolism in mice fed a high-fat diet. Endocrine. 2016;54:648–56.
Geloneze B, Lima MM, Pareja JC, Barreto MR, Magro DO. Association of insulin resistance and GLP-2 secretion in obesity: a pilot study. Arq Bras Endocrinol Metabol. 2013;57:632–5.
Morris A. Obesity: ANGPTL4 - the link binding obesity and glucose intolerance. Nat Rev Endocrinol. 2018;14:251.
Ganesh Kumar K, Zhang J, Gao S, Rossi J, McGuinness OP, Halem HH, et al. Adropin deficiency is associated with increased adiposity and insulin resistance. Obesity (Silver Spring). 2012;20:1394–402.
Kocaoglu C, Buyukinan M, Erdem SS, Ozel A. Are obesity and metabolic syndrome associated with plasma adropin levels in children? J Pediatr Endocrinol Metab. 2015;28:1293–7.
Gao S, McMillan RP, Zhu Q, Lopaschuk GD, Hulver MW, Butler AA. Therapeutic effects of adropin on glucose tolerance and substrate utilization in diet-induced obese mice with insulin resistance. Mol Metab. 2015;4:310–24.
Funding
This study was supported by Technology Innovation Team Train Project of Fuzhou Health Committee in China (2016-S-wp1), and sponsored by key Clinical Specialty Discipline Construction Program of Fuzhou, Fujian, China (201610191).
Author information
Authors and Affiliations
Contributions
RMC conceptualized and designed the study, and reviewed and revised the manuscript. XY drafted the initial manuscript. QO and ZZA collected data and carried out the initial analyses. XQL did the laboratory testing. YZ and XHY collected cases. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethical approval
This study was reviewed and approved by the Ethics Committee of Fuzhou Children’s Hospital of Fujian, and was conducted in agreement with the Declaration of Helsinki Principles. Written informed consent was obtained from all participants for publication of this research and any accompanying clinical data. A copy of the written consent is available for review by the Editor of this journal.
Conflict of interest
All authors have indicated that they have no potential conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chen, RM., Yuan, X., Ouyang, Q. et al. Adropin and glucagon-like peptide-2 are associated with glucose metabolism in obese children. World J Pediatr 15, 565–571 (2019). https://doi.org/10.1007/s12519-019-00296-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12519-019-00296-6