Abstract
Background
Although 99mTc-dimercaptosuccinic acid (DMSA) scan is considered the gold standard for the diagnosis of acute pyelonephritis (AP), sometimes it produces false results in children with clinical features of AP. There are no studies on the comparison of the sensitivity of DMSA and concentrating capacity test.
Methods
Eighty-five infants with AP of less than one year old were studied to evaluate whether they had real AP or not. Data were compared between infants with an abnormal (group A, n=64) and those with a normal DMSA scan (group B, n=21) respectively. A DDAVP test was performed for each infant.
Results
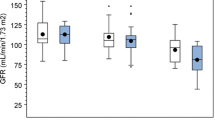
All the infants in both groups presented a high level of C-reactive protein and fever (≥38°C). There were no differences in clinical and analytical variables except C-reactive protein level in the two groups. Both groups exhibited a low urinary osmolality (87.5% in the group A vs. 85.7% in the group B). The patients with normal DMSA and decreased concentrating capacity have some renal parenchymal damage and not only a lower urinary infection. Of the infants with an abnormal DMSA scan, 33.9% showed renal scars after 6–12 months. No infant with a normal DMSA scan showed scars. The biochemical variables in both groups of infants were not related to vesicoureteral refl ux.
Conclusion
Infants with AP, normal DMSA scan and low concentrating capacity may be characterized by a localized infection in the medulla (medullonephritis) or by a false negative DMSA scan.
Similar content being viewed by others
References
Griffin MA. Pyelonephritis in infancy and childhood: its bacteriology and pathology. Arch Dis Child 1934;9:105–114.
Crabtree EG, Prien EL. Nature of renal injury in acute and chronic colon bacillus pyelonephritis in relation to hypertension: combined clinical and pathological study. J Urol 1939;42:982–985.
Jodal U, Lindberg U, Lincoln K. Level diagnosis of symptomatic urinary tract infections in childhood. Acta Paediatr Scand 1975;64:201–208.
Pylkkänen J, Vilska J, Koskimies O. The value of level diagnosis of childhood urinary tract infection in predicting renal injury. Acta Paediatr Scand 1981;70:879–883.
Garin EH, Olavarria F, Araya C, Broussain M, Barrera C, Young L. Diagnostic significance of clinical and laboratory findings to localize site of urinary infection. Pediatr Nephrol 2007;22:1002–1006.
Winberg J. Renal concentration capacity during acute, nonobstructive urinary tract infections in infancy and early childhood. Acta Paediatr 1958;47:635–645.
Clark H, Ronald AR, Cutler RE, Turck M. The correlation between site on infection and maximal concentrating ability in bacteriuria. J Infect Dis 1969;120:47–53.
Aperia A, Berg U, Broberger O. Renal function during hydropenia and water diuresis in children with recurrent urinary tract infections. Acta Paediatr Scand 1970;59:605–612.
Uttley WS, Paxton J, Thistlethwaite D. Urinary concentrating ability and growth failure in urinary tract disorders. Arch Dis Child 1972;47:436–441.
Rodríguez-Soriano J, Vallo A. Renal function disturbance in acute pielonephritis. An Pediatr (Barc) 1975;21 (Suppl 3):21–28
Abyholm G, Monn E. Intranasal DDAVP-test in the study of renal concentrating capacity in children with recurrent urinary tract infections. Eur J Pediatr 1979;130:149–154.
Berg U. Renal function in acute febrile urinary tract infection in children: pathophysiologic aspects on the reduced concentrating capacity. Kidney Int 1981;20:753–758.
Principi N, Dalla Villa A, Assael BM, Gagliardi L, Ghezzi P, Chiccoli C, et al. Urinary excretion of N-acetyl-beta-Dglucosaminidase (NAG) by children with upper or lower urinary tract infections. Acta Paediatr Scand 1982;71:1033–1034.
Everaert K, Raes A, Hoebeke P, Samijn W, Delanghe J, Van de Wiele C, et al. Combined use of urinary alpha1-microglobulin and 99mTc DMSA scintigraphy in the diagnosis and follow-up of acute pyelonephritis and cystitis in children. Eur Urol 1998;34:486–491.
Bingham JB, Maisey MN. An evaluation of the use of 99mTc-dimercaptosuccinic acid (DMSA) as a static renal imaging agent. Br J Radiol 1978;51:599–607.
Thelle T, Biskjaer N. Combined 99mTc-DMSA kidney scintigraphy and 131I-hippuran renography in children with urinary tract infections. Acta Paediatr Scand 1985;74:720–725.
National Institute for Health and Clinical Excellence. Urinary tract infection in children: diagnosis, treatment and long-term management. London: 2007. http://guidance.nice.org.uk/CG54 (accessed May 1, 2012)
Urinary tract infection in children. Clinical guideline. Spanish National Health Department. Health Sciences Institute of Aragón CS N° 2009/01 http://www.guiasalud.es/GPC/GPC_483_ITU_poblacion_pediatrica_ICS_compl.pdf. (accessed May 1, 2012)
Fretzayas A, Moustaki M, Gourgiotis D, Bossios A, Koukoutsakis P, Stavrinadis C. Polymorphonuclear elastase as a diagnostic marker of acute pyelonephritis in children. Pediatrics 2000;105:E28.
Lin DS, Huang SH, Lin CC, Tung YC, Huang TT, Chiu NC, et al. Urinary tract infection in febrile infants younger than eight weeks of age. Pediatrics 2000;105:E20.
Aronson AS, Svenningsen NW. DDAVP test for estimation of renal concentrating capacity in infants and children. Arch Dis Child 1974;49:654–659.
Monnens L, Smulders Y, van Lier H, de Boo T. DDAVP test for assessment of renal concentrating capacity in infants and children. Nephron 1981;29:151–154.
García-Nieto V, González-Cerrato S, García-Rodríguez VE, Mesa-Medina O, Hernández-González MJ, Monge-Zamorano M, et al. Should a cystography be performed on all breastfeeding infants with mild to moderate dilatation of the urinary tract? Renal function tests can help to answer this question Nefrologia 2011;31:192–198.
Yap C, Yap HK, Chio LF. Urine microalbumin/creatinine ratios in Singapore children. The Singapore Paediatr Soc 1991;33:101–106.
Caballo Roig N, Yep Chullen G, de la Torre E, Ruiz Jarabo C, Asensio Antón J, Sánchez Bayle M. Variations in the excretion of N-acetyl-glucosaminidase in the first year of life. An Esp Pediatr 1991;34:142–144.
Beck D, Freedman LR, Levitin H, Ferris TF, Epstein FH. Effect of experimental pyelonephritis on the renal concentrating ability of the rat. Yale J Biol Med 1961;34:52–59.
Gonick HC, Goldberg G, Rubini ME, Guze LB. Functional abnormalities in experimental pyelonephritis. I. Studies of concentrating ability. Nephron 1965;2:193–206.
Kaye D, Rocha H. Urinary concentrating ability in early experimental pyelonephritis. J Clin Invest 1970;49:1427–1437.
Miller TE, Layzell D, Stewart E. Experimental pyelonephritis: the effect of chronic active pyelonephritis on renal function. Kidney Int 1976;9:23–29.
Bricker NS, Dewey RR, Lubowitz H, Stokes J, Kirkensgaard T. Observations on the concentrating and diluting mechanisms of the diseased kidney. J Clin Invest 1959;38:516–523.
Weinstein E, Manitius A, Epstein FH. The importance of aerobic metabolism in the renal concentrating process. J Clin Invest 1969;48:1855–1861.
Rodionova EA, Kuznetsova AA, Shakhmatova EI, Prutskova N, Nielsen S, Holtbäck U, et al. Urinary aquaporin-2 in children with acute pyelonephritis. Pediatr Nephrol 2006;21:361–367.
Pecile P, Miorin E, Romanello C, Falleti E, Valent F, Giacomuzzi F, et al. Procalcitonin: a marker of severity of acute pyelonephritis among children. Pediatrics 2004;114:e249–254.
Kotoula A, Gardikis S, Tsalkidis A, Mantadakis E, Zissimopoulos A, Deftereos S, et al. Comparative efficacies of procalcitonin and conventional inflammatory markers for prediction of renal parenchymal inflammation in pediatric first urinary tract infection. Urology 2009;73:782–786.
Virkola R, Westerlund B, Holthöfer H, Parkkinen J, Kekomäki M, Korhonen TK. Binding characteristics of Escherichia coli adhesins in human urinary bladder. Infect Immun 1988;56:2615–2622.
Chassin C, Tourneur E, Bens M, Vandewalle A. A role for collecting duct epithelial cells in renal antibacterial defences. Cell Microbiol 2011;13:1107–1113.
Chassin C, Goujon JM, Darche S, du Merle L, Bens M, Cluzeaud F, et al. Renal collecting duct epithelial cells react to pyelonephritis-associated Escherichia coli by activating distinct TLR4-dependent and -independent inflammatory pathways. J Immunol 2006;177:4773–4784.
Preda I, Jodal U, Sixt R, Stokland E, Hansson S. Normal dimercaptosuccinicacid scintigraphy makes voiding cystourethrography unnecessary after urinary tract infection. J Pediatr 2007;151:581–584.
Lee J, Kwon DG, Park SJ, Pai KS. Discordant findings on dimercaptosuccinic acid scintigraphy in children with multidetector row computed tomography-proven acute pyelonephritis. Korean J Pediatr 2011;54:212–218.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
García-Nieto, V., González-Cerrato, S., Luis-Yanes, M.I. et al. Decreased concentrating capacity in children with febrile urinary tract infection and normal 99mTc-dimercaptosuccinic acid scan: does medullonephritis exist?. World J Pediatr 10, 133–137 (2014). https://doi.org/10.1007/s12519-014-0482-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12519-014-0482-0