Abstract
A 64-year-old man suffering from an acute posterior wall myocardial infarction underwent primary percutaneous coronary intervention. After several aspiration attempts, tirofiban infusion and pre- and post-dilatation, a bare-metal stent was successfully implanted in the culprit right coronary artery. While the patient did not show any neurological symptoms before or during the procedure, he exhibited hemiplegia and loss of spontaneous speech. Additional magnetic resonance imaging showed an extensive brain stem infarction. This is the first report of a brain stem infarction as a complication of percutaneous coronary intervention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
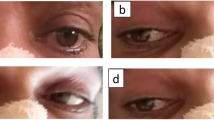
Here we present a case of a 64-year-old man, without any history of cardiovascular risk factors or other comorbidities, who underwent acute percutaneous coronary intervention (PCI) for an acute posterior wall myocardial infarction. Coronary angiography revealed an occluded right coronary artery (Fig. 1a, Online Video 1). In addition, the left circumflex coronary artery showed a non-occlusive thrombus, and the left anterior descending coronary artery revealed a Thrombolysis in Myocardial Infarction grade II flow (Fig. 1b, Online Video 2). After several aspiration attempts and intracoronary administration of tirofiban, the right coronary artery could be reopened with several pre-dilatations and implantation of a Driver Sprint bare-metal 4.5 15-mm stent (Medtronic Inc, Minnesota, USA) with subsequent 5.0 NC balloon post-dilatation. Because of the high thrombus load, successful reperfusion of the posterolateral branch was not possible (Fig. 1c, Online Video 3). A temporary pacemaker was placed before the PCI due to bradycardia. After the procedure, the patient became hemiplegic and exhibited loss of spontaneous speech. Cerebral magnetic resonance imaging revealed an extensive left-sided infarction in the brain stem expanding into the cerebral and cerebellar peduncle (Fig. 2). Thrombolysis was not possible, as dual anti-platelet therapy, heparinisation and continuous intravenous tirofiban had already been initiated. Subsequently, he was mechanically ventilated and treated with antibiotics for 6 days after which he developed aspiration pneumonia caused by neural dysphagia. Although he was extubated after 9 days, he received a tracheostoma due to persistent dysphagia and high risk for aspiration. He was transferred to the stroke unit for further rehabilitation. Coronary angiography and/or percutaneous coronary interventions have been associated with cerebral ischaemic complications. The complication rate varies between 0.07 and 0.4 % of the procedures [1–4]. However, a brain stem infarction is highly unusual compared with cerebral stroke considering the difficult anatomical path for an embolus originating from the aortic arch. Before the embolus reaches the basilar artery, it needs to pass through the subclavian (or the brachiocephalic trunk for right-sided lesions) and the vertebral artery. To our knowledge, this is the first report of an acute pontine infarction as a complication of percutaneous coronary intervention.
References
Dukkipati S, O’Neill WW, Harjai KJ, et al. Characteristics of cerebrovascular accidents after percutaneous coronary interventions. J Am Coll Cardiol. 2004;43:1161–7.
Fuchs S, Stabile E, Kinnaird TD, et al. Stroke complicating percutaneous coronary interventions: incidence, predictors, and prognostic implications. Circulation. 2002;106:86–91.
Palmerini T, Biondi-Zoccai G, Reggiani LB, et al. Risk of stroke with coronary artery bypass graft surgery compared with percutaneous coronary intervention. J Am Coll Cardiol. 2012;60:798–805.
Werner N, Bauer T, Hochadel M, et al. Incidence and clinical impact of stroke complicating percutaneous coronary intervention: results of the euro heart survey percutaneous coronary interventions registry. Circ Cardiovasc Interv. 2013;6:362–9.
Funding
None.
Conflict of interest
Dr. F. Arslan is an associate editor of the Netherlands Heart Journal.
Author information
Authors and Affiliations
Corresponding author
Online video legends
12471_2015_717_MOESM2_ESM.mov
Online Video 2(MOV 424 kb) Coronary angiography showing Thrombolysis in Myocardial Infarction grade II flow in the left anterior descending coronary artery and a non-occlusive thrombus in the left circumflex coronary artery
12471_2015_717_MOESM3_ESM.mov
Online Video 3(MOV 899 kb) Coronary angiography showing Thrombolysis in Myocardial Infarction grade III flow in the right coronary artery after percutaneous coronary intervention with stent placement
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Arslan, F., Mair, J., Franz, WM. et al. Acute pontine infarction after percutaneous coronary intervention: a very rare but devastating complication. Neth Heart J 23, 366–367 (2015). https://doi.org/10.1007/s12471-015-0717-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12471-015-0717-2