Abstract
Purpose of the Review
To review the value of myocardial blood flow and coronary flow reserve (CFR) measurements, as assessed by positron emission tomography (PET), in women with suspected ischemic heart disease.
Recent Findings
CFR is a noninvasive measure of coronary vasomotor function that integrates the hemodynamic effects of epicardial coronary stenosis, diffuse atherosclerosis, and microvascular dysfunction on myocardial tissue perfusion and has emerged as an imaging marker of cardiovascular risk, independently of the degree of obstructive coronary artery disease (CAD).
Summary
Normal coronary arteries or nonobstructive CAD is a common finding in women with ischemia. Thus, assessment of risk based on a coronary stenosis approach may fail in women. PET is able to quantify absolute myocardial blood flow and CFR which may help to elucidate other mechanisms involved such as microvascular dysfunction and diffuse epicardial CAD, responsible for the disease in women.


Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Adamson PD, Newby DE, Hill CL, Coles A, Douglas PS, Fordyce CB. Comparison of international guidelines for assessment of suspected stable angina. JACC Cardiovasc Imaging. 2018;11(9):1301–10. https://doi.org/10.1016/j.jcmg.2018.06.021
Wolk MJ, Bailey SR, Doherty JU, Douglas PS, Hendel RC, Kramer CM, et al. ACCF/AHA/ASE/ASNC/HFSA/HRS/SCAI/SCCT/SCMR/STS 2013 multimodality appropiate use criteria for the detction and risk assessment of stable ischemic heart disease: a report of the American College of Cardiology Foundation Appropiate Use Criteria Task Force, American Heart Association, American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Failure Society of AMerica, Heart Rhythm Society, Society for Cardiovascular Angiopraphy and Interventions, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2014;63(4):380–406. https://doi.org/10.1016/j.jacc.2013.11.009.
Taqueti VR, Dorbala S, Wolinsky D, Abbott B, Heller GV, Bateman TM, et al. Myocardial perfusion imaging in women for the evaluation of stable ischemic heart disease-state-of-the-evidence and clinical recommendations. J Nucl Cardiol. 2017;24(4):1402–26. https://doi.org/10.1007/s12350-017-0926-8.
Pepine CJ, Ferdinand KC, Shaw LJ, Light-McGroary KA, Shah RU, Duvernoy C, et al. Emergence of nonobstructive coronary artery disease: a woman’s problem and need for change in definition on angiography. J Am Coll Cardiol. 2015;66(17):1918–33. https://doi.org/10.1016/j.jacc.2015.08.876.
• Sedlak TL, Lee M, Izadnegahdar M, Merz CN, Gao M, Humphries KH. Sex differences in clinical outcomes in patients with stable angina and no obstructive coronary artery disease. Am Heart J. 2013;166(1):38–44. https://doi.org/10.1016/j.ahj.2013.03.015 This study describes that women with stable angina and nonobstructive CAD are three times more likely to experience a cardiac event within the first year of cardiac catheterization than symptomatic men with nonobstructive CAD.
Eastwood JA, Johnson BD, Rutledge T, Bittner V, Whittaker KS, Krantz DS, et al. Anginal symptoms, coronary artery disease, and adverse outcomes in black and white women: the NHLBI-sponsored Women’s Ischemia Syndrome Evaluation (WISE) study. J Women's Health. 2013;22(9):724–32. https://doi.org/10.1089/jwh.2012.4031.
• Mieres JH, Bonow RO. Ischemic heart disease in women. JACC Cardiovasc Imaging. 2016;9(4):347–9. https://doi.org/10.1016/j.jcmg.2016/02.008 This review highlights the need for sex-specific approaches for the evaluation of CAD.
Baldassarre LA, Raman SV, Min JK, Mieres JH, Gulati M, Wenger NK, et al. Noninvasive imaging to evaluate women with stable ischemic heart disease. JACC Cardiovasc Imaging. 2016;9(4):421–35. https://doi.org/10.1016/j.jcmg.2016.01.004.
• Taqueti VR, Di Carli MF. Clinical significance of noninvasive coronary flow reserve assessment in patients with ischemic heart disease. Curr Opin Cardiol. 2016;31:662–9. https://doi.org/10.1097/HCO.0000000000000339 This review summarizes all the evidence about coronary flow reserve measurements as a marker of cardiac risk in special populations.
• Taqueti VR, Hachamovitch R, Murthy VL, Naya M, Foster CR, Hainer J, et al. Global coronary flow reserve is associated with adverse cardiovascular events independently of luminal angiographic severity and modifies the effect of early revascularization. Circulation. 2015;131(1):19–27. https://doi.org/10.1161/CIRCULATIONAHA.114.011939 This study highlights the prognostic impact of microvascular dysfunction and diffuse atherosclerosis over the degree of coronary stenosis.
Campisi R, Marengo FM. Coronary microvascular dysfunction in women with nonobstructive ischemic heart disease as assessed by positron emission tomography. Cardiovasc Diagn Ther. 2017;7(2):196–205. https://doi.org/10.21037/cdt.2017.0408.
Murthy VL, Bateman TM, Beanlands RS, Berman DS, Borges-Neto S, Chareonthaitawee P, et al. Clinical quantification of myocardial blood flow using PET: joint position paper of the SNMMI cardiovascular council and the ASNC. J Nucl Cardiol. 2018;25:269–97. https://doi.org/10.1007/s12350-017-1110-x.
Al Badarin F, Aljizeeri A, Almasoudi F, Al-Mallah MH. Assessment of myocardial blood flow and coronary flow reserve with positron emission tomography in ischemic heart disease: current state and future directions. Heart Fail Rev. 2017;22(4):441–53. https://doi.org/10.1007/s10741-017-9625-4.
Camici PG, Rimoldi OE. The clinical value of myocardial blood flow measurement. J Nucl Med. 2009;50(7):1076–87. https://doi.org/10.2967/jnumed.108.054478.
Schindler TH. Myocardial blood flow: putting it into clinical perspective. J Nucl Cardiol. 2016;23(5):1056–71. https://doi.org/10.1007/s12350-015-0372-4.
García EV. Proceedings of the cardiac PET summit meeting12 may 2014: cardiac PET and SPECT instrumentation. J Nucl Cardiol. 2015;22:563–70. https://doi.org/10.1007/s12350-015-0114-7.
Gewirtz H, Dilsizian V. Integration of quantitative positron emission tomography absolute myocardial blood flow measurements in the clinical management of coronary artery disease. Circulation. 2016;133(22):2180–96. https://doi.org/10.1161/CIRCULATIONAHA.115.018089.
Gould KL, Johnson NP, Bateman TM, Beanlands RS, Bengel FM, Bober R, et al. Anatomic versus physiologic assessment of coronary artery disease. Role of coronary flow reserve, fractional flow reserve, and positron emission tomography imaging in revascularization decision-making. J Am Coll Cardiol. 2013;62(18):1639–53. https://doi.org/10.1016/j.jacc.2013.07.076.
Naya M, Murthy VL, Taqueti VR, Foster CR, Klein J, Garber M, et al. Preserved coronary flow reserve effectively excludes high-risk coronary artery disease on angiography. J Nucl Med. 2014;55(2):248–55. https://doi.org/10.2967/jnumed.113.121442.
Naya M, Murhty VL, Blankstein R, Sitek A, Hainer J, Foster C, et al. Quantitative relationship between the extent and morphology of coronary atherosclerotic plaque and downstream myocardial perfusion. J Am Coll Cardiol. 2011;58(17):1807–16. https://doi.org/10.1016/j.jacc.2011.06.051.
Rodriguez-Granillo GA, Campisi R, Carrascosa P. Noninvasive cardiac imaging in patients with known and suspected coronary artery disease: what is in it for the interventional cardiologist? Curr Cardiol Rep. 2016;18:3. https://doi.org/10.1007/s11886-015-0680-y.
Driessen RS, Stuijfzand WJ, Raijmakers PG, Danad I, Min JK, Leipsic JA, et al. Effect of plaque burden and morphology on myocardial blood flow and fractional flow reserve. J Am Coll Cardiol. 2018;71(5):499–509. https://doi.org/10.1016/j.jacc.2017.11.054.
Nandalur KR, Dwamena BA, Choudhri AF, Nandalur SR, Reddy P, Carlos RC. Diagnostic performance of positron emission tomography in the detection of coronary artery disease: a meta-analysis. Acad Radiol. 2008;15:444–51. https://doi.org/10.1016/j.acra.2007.08.012.
Beanlands R, Heller G. Proceedings of the ASNC cardiac PET summit, 12 May 2014, Baltimore, MD: 1: the value of PET: integrating cardiovascular PET into the care continuum. J Nucl Cardiol. 2015;22(3):557–62. https://doi.org/10.1007/s12350-015-0129-0.
Mc Ardle BA, Dowsley TF, de Kemp RA, Wells GA, Beanlands RS. A systematic review and meta-analysis. Does rubidium-82 PET have superior accuracy to SPECT perfusion imaging for the diagnosis of obstructive coronary disease? J Am Coll Cardiol. 2012;60(8):1828–37. https://doi.org/10.1016/j.jacc.2012.07.038.
Parker MW, Iskandrian A, Limone B, Perugini A, Kim H, Jones C, et al. Diagnostic accuracy of cardiac positron emission tomography versus single photon emission computed tomography for coronary artery disease: a bivariate meta-analysis. Circ Cardiovasc Imaging. 2012;5(6):700–7. https://doi.org/10.1161/CIRCIMAGING.112.97827.
Bateman TM, Heller GV, McGhie AI, Friedman JD, Case JA, Bryngelson JR, et al. Diagnostic accuracy of rest/stress ECG-gated Rb-82 myocardial perfusion PET: comparison with ECG-gated Tc-99m sestamibi SPECT. J Nucl Cardiol. 2006;13(1):24–33. https://doi.org/10.1016/j.nuclcard.2005.12.004.
Dorbala S, Di Carli MF, Beanlands RS, Merhige ME, Williams BA, Veledar E, et al. Prognostic value of stress myocardial perfusion positron emission tomography: results from a multicenter observational registry. J Am Coll Cardiol. 2013;61(2):176–84. https://doi.org/10.1016/j.jacc.2012.09.043.
Kay J, Dorbala S, Goyal A, Fazel R, Di Carli MF, Einstein AJ, et al. Influence of sex on risk stratification with stress myocardial perfusion Rb-82 positron emission tomography: results from the PET (positron emission tomography) prognosis multicenter registry. J Am Coll Cardiol. 2013;62(20):1866–76. https://doi.org/10.1016/j.jacc.2013.06.017.
Lertsburapa K, Ahlberg AW, Bateman TM, Katten D, Volker L, Cullom SJ, et al. Independent and incremental prognostic value of left ventricular ejection fraction determined by stress gated rubidium 82 PET imaging in patients with known or suspected coronary artery disease. J Nucl Cardiol. 2008;15(6):745–53. https://doi.org/10.1007/BF03007355.
Ong P, Camici PG, Beltrame JF, Crea F, Shimokawa H, Sechtem U, et al. International standardization of diagnostic criteria for microvascular angina. Int J Cardiol. 2018;1(250):16–20. https://doi.org/10.1016/j.ijcard.2017.08.068.
Campisi R, Nathan L, Pampaloni MH, Schoeder H, Sayre JW, Chaudhuri G, et al. Noninvasive assessment of coronary microcirculatory function in postmenopausal women and effects of short-term and long-term estrogen administration. Circulation. 2002;105(4):425–30.
Schindler TH, Campisi R, Dorsey D, Prior JO, Olschewski M, Sayre J, et al. Effect of hormone replacement therapy on vasomotor function of the coronary microcirculation in post-menopausal women with medically treated cardiovascular risk factors. Eur Heart J. 2009;30(8):978–86. https://doi.org/10.1093/eurheartj/ehp013.
Herzog BA, Husmann L, Valenta I, Gaemperli O, Siegrist PT, Tay FM, et al. Long-term prognostic value of 13N-ammonia myocardial perfusion positron emission tomography added value of coronary flow reserve. J Am Coll Cardiol. 2009;54(2):150–6. https://doi.org/10.1016/j.jacc.2009.02.069.
Ziadi MC, DeKemp RA, Williams KA, Guo A, Chow BJ, Renaud JM, et al. Impaired myocardial flow reserve on rubidium-82 positron emission tomography imaging predicts adverse outcomes in patients assessed for myocardial ischemia. J Am Coll Cardiol. 2011;58(7):740–8. https://doi.org/10.1016/j.jacc.2011.01.065.
Fukushima K, Javadi MS, Higuchi T, Lautamaeki R, Merrill J, Nekolla SG, et al. Prediction of short-term cardiovascular events using quantification of global myocardial flow reserve in patients referred for clinical 82Rb PET perfusion imaging. J Nucl Med. 2011;52(5):726–32. https://doi.org/10.2967/jnumed.110.081828.
Murthy VL, Naya M, Foster CR, Hainer J, Gaber M, Di Carli G, et al. Improved cardiac risk assessment with noninvasive measures of coronary flow reserve. Circulation. 2011;124(20):2215–24. https://doi.org/10.1161/CIRCULATIONAHA.111.050427.
Naya M, Murthy VL, Foster CR, Gaber M, Klein J, Hainer J, et al. Prognostic interplay of coronary artery calcification and underlying vascular dysfunction in patients with suspected coronary artery disease. J Am Coll Cardiol. 2013;61(20):2098–106. https://doi.org/10.1016/j.jacc.2013.02.029.
Murthy VL, Naya M, Taqueti VR, Foster CR, Gaber M, Hainer J, et al. Effects of sex on coronary microvascular dysfunction and cardiac outcomes. Circulation. 2014;129(4):2518–27. https://doi.org/10.1161/CIRCULATIONAHA.114.011939.
Taqueti VR, Shaw LJ, Cook NR, Murthy VL, Shah NR, Foster CR, et al. Excess cardiovascular risk in women relative to men referred for coronary angiography is associated with severely impaired coronary flow reserve, not obstructive disease. Circulation. 2017;135(6):566–77. https://doi.org/10.1161/CIRCULATIONAHA.116.023266.
Taqueti VR, Solomon SD, Shah AM, Desai AS, Groarke JD, Osborne MT, et al. Coronary microvascular dysfunction and future risk of heart failure with preserved ejection fraction. Eur Heart J. 2018;39(10):840–9. https://doi.org/10.1093/eurheartj/ehx721.
Acknowledgments
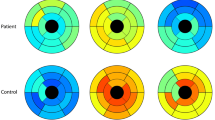
The authors are thankful to Daniel Cirigliano for the artwork.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Roxana Campisi and Fernando D. Marengo declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This Article is part of the Topical Collection on Cardiac Nuclear Imaging
Rights and permissions
About this article
Cite this article
Campisi, R., Marengo, F.D. Myocardial Perfusion Imaging for the Evaluation of Ischemic Heart Disease in Women. Curr Cardiovasc Imaging Rep 12, 4 (2019). https://doi.org/10.1007/s12410-019-9479-3
Published:
DOI: https://doi.org/10.1007/s12410-019-9479-3