Abstract
Background
We present an automatic method for coronary artery calcium (CAC) quantification and cardiovascular risk categorization in CT attenuation correction (CTAC) scans acquired at rest and stress during cardiac PET/CT. The method segments CAC according to visual assessment rather than the commonly used CT-number threshold.
Methods
The method decomposes an image containing CAC into a synthetic image without CAC and an image showing only CAC. Extensive evaluation was performed in a set of 98 patients, each having rest and stress CTAC scans and a dedicated calcium scoring CT (CSCT). Standard manual calcium scoring in CSCT provided the reference standard.
Results
The interscan reproducibility of CAC quantification computed as average absolute relative differences between CTAC and CSCT scan pairs was 75% and 85% at rest and stress using the automatic method compared to 121% and 114% using clinical calcium scoring. Agreement between automatic risk assessment in CTAC and clinical risk categorization in CSCT resulted in linearly weighted kappa of 0.65 compared to 0.40 between CTAC and CSCT using clinically used calcium scoring.
Conclusion
The increased interscan reproducibility achieved by our method may allow routine cardiovascular risk assessment in CTAC, potentially relieving the need for dedicated CSCT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Coronary artery calcium (CAC) is a marker of atherosclerosis1 and its presence and the amount increase the risk of any cardiovascular event in symptomatic and asymptomatic individuals.2,3,4 Moreover, the amount of CAC is associated with the likelihood of myocardial ischemia.5 Traditionally, CAC is scored manually by an expert in dedicated, ECG-triggered, non-contrast, calcium scoring CT (CSCT) scans, following a previously described and strictly defined method.6 However, CAC can be quantified in any CT scan visualizing the heart,7 including CT attenuation correction scans that are acquired in nuclear imaging of the heart.8,9,10 As recommended by the Society of Cardiovascular Computed Tomography and Society of Thoracic Radiology (SCCT/STR), CAC derived from CTAC scans enables risk categorization and should be reported, although there is still insufficient evidence on which method to use.11
Specifically, in clinical practice, during the myocardial perfusion PET and SPECT scan, a CT attenuation correction (CTAC) scan is acquired that visualizes the heart. If the CTAC could be used for calcium scoring, the acquisition of CSCT scan could be omitted, which would decrease the radiation dose to the patient and increase time and cost efficiency. However, the acquisition of CTAC images is not optimized for CAC scoring, which hampers visualization of calcium lesions and hence, quantitative CAC measurement from these scans. Furthermore, the clinical CAC scoring procedure, which uses a 130 HU threshold to define calcium lesions and enables their detection, limits the reproducibility of CAC quantification12: lesions may remain partly or completely below the threshold, because non-ECG-synchronized CTAC scans are heavily affected by cardiac motion and partial volume effect. Therefore, visual calcium assessment from CTAC, which was previously described by Einstein et al and is known to have good agreement with the reference standard CSCT scans, was a proposed solution.8,13 It overcomes the discrepancy in acquisition settings between CTAC and reference standard CSCT scan and enables comparison regardless of vendor, tube voltage, slice thickness, and CT-number threshold. However, visual calcium scoring is inherently subjective and requires valuable expert reading time. Therefore, an automatic method may enable robust and time efficient CAC quantification. Therefore, we optimized and evaluated a fully automatic CAC quantification method that does not rely on the clinically used CT-number threshold14,15 in CTAC scans, but instead it is based on visual assessment of CAC. Moreover, we design automated risk categorization based on this automatic CAC quantification. Therefore, the aim of this study is threefold: to present an automatic method for optimized CAC quantification in CTAC scans of myocardial perfusion PET, to present automated risk categorization that reproduces expert visual scoring, and to compare the performance to manual calcium scoring from dedicated CSCT scans.
Materials and Methods
Patients and imaging data
In this retrospective study we included 742 consecutive patients (58 ± 10, 53.2% male) who underwent a 15O-water-PET/CTAC and a dedicated CSCT scan between 2008 and 2014 due to known or suspected coronary artery disease (CAD).16 Two CTAC scans per patient were acquired: one in rest and one in stress condition. The latter was induced pharmacologically using intravenous adenosine (140 mg/kg/min) infusion. CTAC scans were acquired on a Gemini TF64 PET/CT scanner (Philips Healthcare, Best, the Netherlands) without contrast enhancement, with 120 kVp and without ECG synchronization. Images were reconstructed to 1.17 mm in-plane resolution and 5 mm slice thickness and increment. Dedicated CSCT scans were acquired on a 256-slice Brilliance iCT-scanner (Philips Healthcare, Best, the Netherlands) without contrast enhancement, with a tube voltage of 120 kVp and with ECG synchronization for optimal visualization of the coronary arteries. Images were reconstructed to 0.36-0.47 mm in-plane resolution and 2.5 mm slice spacing and increment.
In total 50 patients were excluded; 36 were excluded due to incomplete imaging data and 14 were excluded due to uninterpretable images, e.g., severe artifacts due to low dosage (43%) or metal implants (57%), which resulted in a set of 692 patients. The study complied with the Declaration of Helsinki. The need for written informed consent was waived due to the retrospective design of the study by the institutional review board (Medical Ethics Committee of the Amsterdam UMC, Vrije Universiteit Amsterdam).
Additionally, to enhance the training with ample examples of CAC lesions due to a high CAC burden in non-dedicated CT scans, 629 low-dose chest CT acquired at baseline from participants of the National Lung Screening Trial (NLST)17 were included. This set was previously used for development of a calcium scoring method and was designed to be diverse with respect to scanner model and reconstruction algorithm.15,18 CT scans were, like CTAC, acquired without contrast enhancement and without ECG synchronization. NLST acquisition was made with a tube voltage of 120 kVp or 140 kVp, depending on the subject’s weight. Images were reconstructed to 0.49-0.98 mm in-plane resolution, 1.0-2.5 mm slice thickness, and 0.6-2.5 mm increment. To make the slice thickness uniform in our study, the scans were resampled to 3.0 mm slice thickness and 1.5 mm increment, following earlier studies.18,19,20
For training, a set of all available NLST data and 136 CTAC scans of 68 patients were used. For evaluation two hold-out sets were used: evaluation Set 1 of 100 cardiac patients for comparison with the clinically used method and evaluation Set 2 consisting of 461 cardiac patients for comparison with visual scores only. In both evaluation sets each patient had 2 CTAC scans and a CSCT scan.
Reference data
The automatic method used in this study consists of several components. To train and evaluate each of these, expert-defined reference data were obtained.
Training automatic calcium scoring
Our method aims to quantify calcifications in CTAC scans according to visual assessment rather than using the CT-number threshold for calcium extraction. Nevertheless, manual annotation of calcified voxels in the coronary arteries would be practically infeasible. Therefore, to train the automatic CAC scoring, for each axial CT slice in the training set, the presence of CAC (yes/no) was defined by visual assessment. This was performed by an expert observer (S.G.M.V) with > 5 years of experience in calcium scoring.
Moreover, to limit the analysis to the region of interest only, i.e., to train the automatic heart segmentation in CTAC scans, the heart was manually segmented in a subset of the training data. This set comprised a randomly chosen set of 39 NLST scans and 29 CTAC scans. The segmentation was performed by voxel painting the heart by the same observer (S.G.M.V).
Manual calcium scoring
To allow comparison with standard clinically accepted calcium scoring procedure that exploits the intensity-based threshold,6 a trained observer (R.L.M.H) manually annotated calcium following the clinical procedure in all CTAC scans and CSCT scans in evaluation Set 1. This was done using in-house custom-built software for semi-automatic calcium scoring,19,21 in which the observer identified lesions with ≥ 130 HU. For each scan, CAC was quantified into Agatston score6 and assigned to one in five cardiovascular risk categories (I: 0, II: 1-10, III: 11-100, IV: 100-400, V: > 400).21,22
Visual scores
To allow comparison of the automatic CAC quantification with visual evaluation in CSCT and CTAC, visual scoring was performed in evaluation Set 1 and Set 2 by an expert observer with > 2 years of experience in visual calcium scoring (M.M.D). Visual scoring was performed as described by Einstein et al by estimating the Agatston risk category the scan belonged to.8 To enable comparison between clinically used Agatston risk categories, instead of a six-point scale used by Einstein et al, the same five-point scale as described above was used (I: 0, II: 1-10, III: 11-100, IV: 100-400, V: > 400).
Automating visually assessed CAC quantification
In CTAC scans, CAC scoring is challenged by large slice thickness, low in-plane image resolution, motion artifacts, and image noise. Hence, to detect and quantify CAC lesions partly or completely below the standardly used CT-number threshold, we utilize a method that does not rely on the clinically used CT-number threshold of 130 HU.14,15 The method decomposes an image slice containing CAC into its counterpart without CAC and a CAC-map, that is an image indicating area and density of calcifications (Figure 1). In this work, the method is specifically optimized for the CTAC scans. Moreover, to simplify the analysis, we limit generation of CAC-maps to the heart region only.
Defining the region of interest
Prior to analysis, all images were resampled to 1.0 mm in-plane resolution and 1.5 mm slice spacing. To simplify the task of CAC quantification, we identify the region of interest by heart segmentation. Since manual heart segmentation of a large (training) set is time consuming, the heart is automatically segmented using a 3D convolutional neural network (CNN) with a Resnet architecture (Figure 2). The CNN was trained with a subset of the training set (36 NLST and 26 CTAC scans), with available reference heart segmentations. The trained CNN was used to segment the heart in the remaining training scans and in the evaluation set.
Subsequently, to select slices for CAC quantification during testing, the slices containing CAC were identified through classification according to presence of visible CAC lesions. This was done using a 2D CNN with a Resnet architecture (Figure 2) that was trained using reference labels indicating the presence of CAC in an axial slice.
CAC quantification
Manual annotation of CAC by, e.g., mouse painting that is based on visual evaluation, i.e., without using a threshold, is hardly feasible. Hence, a reference standard CAC-map for training a segmentation CNN is practically not attainable. Instead, we use a method that decomposes an image with CAC into an image without CAC and a CAC-map (Figure 1).14,15 This is done by generating a synthetic image without CAC from the image containing CAC. The CAC-map is then computed as the difference between the input image with CAC and the synthetic counterpart without CAC. Standardly, generative adversarial networks (GANs) are used for image synthesis, which are often trained using paired images. However, image pairs, i.e., images of the same patient, where one image contains CAC and the other image does not, do not exist. Hence, we use an approach that allows image synthesis using unpaired training: namely, we use a CycleGAN,23 a system of CNNs that translates images from one domain to another and vice versa using unpaired training data.
As proposed in our previous work,14,15 one domain is defined by images containing CAC (CAC domain) and the other domain by images without CAC (noCAC domain) (Figure 3). Hence, the CycleGAN translates CAC images into noCAC images and vice versa.14,15 In this approach, the CAC-map is defined as the difference between the CAC image and the synthetic noCAC counterpart. The CycleGAN contains two generator CNNs that synthesize images: the removing generator (GRem) that translates from the CAC domain to the noCAC domain by generating a CAC-map and subtracting it from the input CAC image and the synthesizing generator (GSyn) that translates from the noCAC domain to the CAC domain by generating a CAC-map and adding it to the input noCAC image. Next to these, the CycleGAN contains two discriminator CNNs that determine how well the synthesized images match real images in the target domain. By optimizing the generators and discriminators together, the generators are trained to produce realistic synthetic images and hence, a realistic CAC-map.
Schematic overview of the CycleGAN used for CAC segmentation, i.e., generating the CAC-maps. Images containing CAC (CAC domain) are translated into images without CAC (noCAC domain) by predicting a CAC-map with the generator (GRem) and subtracting it from the input image. Images from the noCAC domain are translated to the CAC domain by adding the CAC-map, predicted by GSyn, to the input image without CAC. The discriminators determine how well the synthesized images match real images in their domain
To optimize the calcium quantification for the CTAC scans, the CycleGAN is trained using the training set of 629 scans from NLST and 114 CTAC scans (57 rest and 57 stress) of 57 patients that underwent 15O-water-PET/CTAC imaging. In each training scan the heart was segmented. For training, axial scan slices were assigned to either the CAC or noCAC domain based on the presence of visible CAC in the slice indicated by the reference labels. Given that images with and without CAC of the same patients do not exist, we utilize an unpaired training approach, i.e., CAC and noCAC images originate either from different patients and/or different anatomical levels. The CycleGAN was trained for 375.000 iterations, with a learning rate of 0.0001 using batches of four axial CT slices of 224 × 224 voxels. For more details on, e.g., architecture, loss functions, and hyperparameters for training, we refer to our previous work.14,15 After training the CycleGAN, its GRem was used to obtain the CAC-maps. Thereafter, in CTAC scan, CAC was quantified into CAC pseudomass. To allow comparison with clinical calcium scoring in CSCT, this was done using the original image values of the CAC area as indicated in the CAC-map, instead of directly using the CAC-maps. Since the scans are not calibrated for quantification of CAC mass, we calculate CAC pseudomass, which is the uncalibrated CAC mass. The CAC pseudomass is computed as the sum of the CT-number values in the lesion multiplied by the voxel spacing.24
Automated risk categorization
In clinical care, patients are assigned to a cardiovascular risk category to determine the risk of experiencing a CVD event and the risk of myocardial ischemia.2,5,25 The clinically used risk categories are based on Agatston scores that utilize the 130 HU threshold.6 Hence, our CAC quantification cannot be directly translated to Agatston scores or risk categories based on the Agatston scores. Moreover, since the CTAC images are heavily affected by cardiac motion artifacts and partial volume effect, previous research shows that visual scoring may have better agreement with Agatston risk categories in CSCT.8 Therefore, based on the proposed automatic CAC quantification, the scans were assigned a cardiovascular risk category (\({\mathrm{Vis}}_{\mathrm{auto}}\)) on a five-point scale that was calibrated using visual scores. For this, the CAC pseudomass is log transformed and calibrated using the following formula:
Calibration of the scaling factors (\(\alpha \) and \(\gamma \)), offset (\(\delta \)), and base of the logarithm (\(\beta \)) was performed for rest and stress CTAC separately in SPSS 28.26 For each scan type, four scans from the training set with a visual score of 2, 3, 4, and 5 were randomly selected, totaling 16 scans. These scans were not used in evaluation in any way. Regression between the CAC pseudomass and visual score of these scans was used to determine \(\alpha \), \(\beta \), \(\gamma \), and \(\delta \). The following parameters for calibration were found: \(\alpha = 3.1, \beta = 9.0, \gamma = 1.1\) and \(\delta =1.6\) for rest CTAC; \(\alpha = 3.5, \beta = 9.0, \gamma = 1.0\) and \(\delta = 1.5\) for stress CTAC.
Evaluation
The performance of automatic calcium scoring in CTAC scans was evaluated using standard clinical calcium scoring with a 130 HU threshold in CSCT scans as a reference. For comparison, the amount of CAC in both CTAC and CSCT was quantified with CAC pseudomass. Please note that the scans are not calibrated for CAC mass. Furthermore, automatic scoring in CTAC (without CT-number threshold) was compared with manual clinical calcium scoring following the clinical scoring protocol (using 130 HU threshold).
The performance of the proposed method was evaluated through the interscan reproducibility of CAC quantification, between CTAC and CSCT scan pairs, using average absolute relative differences (\({\Delta }_{R}\)). This is computed as the absolute difference between CAC scores in CTAC and CSCT divided by their mean:
Moreover, Bland–Altman plots with 95% limits of agreement were assessed. Because errors tend to increase with increasing amount of CAC, the limits of agreement were determined using regression to model the variation of the absolute differences between measures from CTAC and CSCT and multiplying by \(1.96\cdot (\pi /2{)}^{1/2}\) because the absolute differences have a half-normal distribution.27
Next, the ability of the automatic method to detect the presence of CAC in CTAC scans using CSCT as the reference was determined using sensitivity, specificity, and F1 score.
Finally, to evaluate whether automated risk categorization in CTAC is feasible, agreement in cardiovascular risk categorization between automatic risk category assignment in CTAC and risk category assignment based on the Agatston scores in CSCT was evaluated using Cohen’s linearly weighted kappa \(\left( {\kappa_{LW} } \right)\). Automated risk categorization was compared with both risk categorization based on manual Agatston scores from CTAC and visual scoring performed in CSCT and CTAC, by an observer.
Results
Quantification of CAC
Using the described automatic method, CAC was identified in CTAC scans from the evaluation set. The performance was evaluated on the images of patients in the evaluation set in terms of interscan reproducibility of CAC quantification and detection of presence of CAC using standard manual clinical calcium scoring in CSCT as reference.
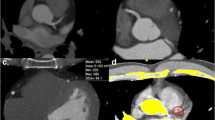
Interscan reproducibility
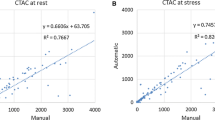
To assess the interscan reproducibility of calcium quantification in CTAC scans in evaluation Set 1, we compared the calcium scores in CTAC using here described automatic (without CT-number threshold) and manual clinical segmentation (with 130 HU threshold) with calcium scores from CSCT obtained using manual clinical procedure (with 130 HU threshold). Using the automatic CAC quantification with pseudomass, the \({\Delta }_{R}\) was 118% for rest scans and 121% for stress scans (Table 1). In concordant scan pairs, i.e., pairs in which CAC was detected in both the CTAC and CSCT scan, \({\Delta }_{R}\) was 75% and 85% in rest and stress scans, respectively. In comparison, with manual clinical calcium scoring a \({\Delta }_{R}\) in CAC pseudomass of 159% in rest scans and 153% in stress scans was found. In concordant pairs the \({\Delta }_{R}\) was 121% and 114% in CAC pseudomass, for rest and stress scans, respectively. For Agatston scores obtained using manual clinical calcium scoring similar results were obtained (Table 1). Figure 4 shows examples of CAC lesions identified on CTAC using the automatic method.
Figure 5 shows Bland–Altman plots with 95% limits of agreement in CAC pseudomass extracted from CTAC scans and CSCT scans in evaluation Set 1. It can be appreciated that the agreement is better for the automatic CAC quantification method than for manual clinical calcium scoring. Moreover, manual clinical calcium scoring shows systematic underestimation (negative differences) of the CAC pseudomass.
Bland–Altman plots of CAC pseudomass with 95% limits of agreement (dashed lines) comparing manual reference scoring in CSCT with quantification in CTAC using the automatic method (top) and manual calcium scoring (bottom) in evaluation set 1 (N = 98). 95% are represented by the following formula: \(\mathrm{Difference }=b \pm 1.96\cdot (\uppi /2{)}^{1/2}\cdot a\cdot {\mathrm{mean}}^{1/2}\). For automatic quantification the coefficients a and b are 295 and − 8757 in rest CTAC and 261 and − 3210 in stress CTAC. For manual scoring the coefficients a and b are 524 and − 17,465 in rest CTAC and 416 and − 11,251 in stress CTAC. Outliers are indicated by an arrow
Detection of presence of CAC
According to manual clinical calcium scoring in CSCT evaluation scans, CAC was present in 67 out of 98 patients (68%) in evaluation Set 1. The automatic method detected CAC in 72% and 77% of these scans (sensitivity) and found 7 and 8 false-positive scans in rest and stress CTAC scans, respectively (Table 2). In comparison, manual clinical calcium scoring in CTAC showed substantially lower sensitivity of 54% and 58%, but with 3 and 4 false-positive scans in rest and stress CTAC scans, respectively. Visual assessment of the false-positive cases of the automatic method revealed that in 53% non-coronary calcium was detected (e.g., in the ascending aorta and cardiac valves), in 13% ring artifacts were detected as CAC, and in 33% image noise in the vicinity of the coronary arteries was detected as CAC.
Automated risk categorization
According to visual scoring in CSCT, 67/98 patients (68%) in evaluation Set 1 had CAC. The automated risk categorization in CTAC showed a moderate agreement with expert visual scores in CSCT, with a \({\kappa }_{LW}\) of 0.65 (CI 0.54-0.76) in rest scans and 0.65 (CI 0.55-0.75) in stress scans (Table 3). Similarly, a moderate agreement with the clinical standard, namely with Agatston risk categories determined on CSCT, was found with a \({\kappa }_{LW}\) of 0.65 (CI 0.54-0.77) in rest CTAC and a \({\kappa }_{LW}\) of 0.65 (CI 0.55-0.76) in stress CTAC. Concordance matrixes are shown in Figure 6. When comparing automated risk categorization in CTAC with expert visual scores in the same scans, a good agreement was found with \({\kappa }_{LW}\) of 0.71 (CI 0.60-0.81) in rest scans and 0.73 (CI 0.64-0.83) in stress scans.
The agreement of expert visual scores in CTAC with visual scores in CSCT was lower in evaluation Set 2 with a \({\kappa }_{LW}\) of 0.63 (95% CI 0.58-0.68) in rest CTAC and 0.65 (95% CI 0.60-0.70) in stress CTAC. This was due to false-negative findings, in which CAC was visible in the CSCT but not in the CTAC (Figure 7). In line with this, the agreement between automated risk categorization in CTAC and visual risk categorization in CSCT showed a \({\kappa }_{LW}\) of 0.55 (95% CI 0.55-0.61) in rest CTAC and 0.58 (95% CI 0.52-0.63) in stress CTAC. Comparing automated risk categorization in CTAC with visual scores in CTAC in evaluation Set 2 led to a \({\kappa }_{LW}\) was 0.69 (CI 0.63-0.74) in rest scans and 0.63 (CI 0.58-0.69) in stress scans.
Since a CAC Agatston score > 400 is strongly associated with myocardial ischemia in patients with suspected CAD,28 we evaluate detection of high CAC patients from CTAC. Note that manual Agatston scores are only available for evaluation Set 1. Using automated risk categorization 21 and 20 out of 21 patients in evaluation Set 1 with > 400 Agatston score on CSCT were correctly identified in rest and stress CTAC, respectively. In both rest and stress CTAC, 8 out of 77 patients with a score < 400 on the CSCT were incorrectly identified as having a > 400 score by automated risk categorization.
The automatic method correctly classified 5 patients in rest CTAC and 4 patient in stress CTAC out of 22 patients with a reference Agatston score between 1 and 100 on the CSCT. Among these 22 patients, 12 had no visible CAC in the rest CTAC scan and 10 had no visible CAC in the stress CTAC scan. The performance of manual calcium scoring in CTAC was similar, with 4 patients at rest and 5 patients at stress correctly classified. Both the automatic method and manual calcium scoring in CTAC correctly classified zero patients out of 6 with a reference Agatston score between 1 and 10 on the CSCT.
Discussion
This study presented and evaluated an automatic method for quantification of CAC that is based on visual assessment of CAC and specifically optimized for rest and stress CTAC scans acquired during myocardial perfusion PET/CT scans. CAC quantification using our method enables higher sensitivity of CAC detection and increased interscan reproducibility between CTAC and CSCT of CAC pseudomass compared with clinical calcium scoring in CTAC scans. Moreover, this study presented automated risk categorization from CTAC that showed a higher agreement with Agatston score-based CVD risk categories in CSCT than manual CAC scoring in CTAC following the clinical protocol.
Given that the presented CAC scoring does not depend on a predefined CT-number threshold for manual calcium detection, it addressed the limitations imposed by non-dedicated image acquisition protocols of CTAC scans that hamper manual CAC scoring. Recent trends in CAC scoring from all chest CT scans have led to a proliferation of studies focused on CAC assessment from CTAC scans.9,10,29 Mylonas et al achieved high agreement between manual CAC scoring from CTAC and standard clinical CSCT by decreasing the detection threshold to 50 HU.9 However, when the conventional 130 HU threshold was applied, the agreement with CSCT scan decreased to κ = 0.33. A major drawback of decreasing the detection threshold regardless of scan acquisition parameters is that it does not reflect the Agatston scoring method.6 As previously described, the CT-number threshold is dependent on the tube voltage applied in acquisition and should be adjusted accordingly.30 Moreover, this CT-number threshold would have to be changed following different PET and SPECT CT scanners and all varieties of protocols with different tube voltage levels. Therefore, our automated risk categorization method enables CAC detection regardless of the used tube voltage.
Moreover, automated CVD risk categorization in CTAC scans strongly outperformed risk categorization based on manual CAC scoring in CTAC scans. This might be explained by a high level of present motion artifacts due to lack of ECG synchronization in the CTAC scans, which cause lesions to (partly) remain below the 130 HU detection threshold used in clinical calcium scoring. Moreover, the slice thickness of CTAC used in this study was 5 mm, instead of 3 mm that is standardly used in calcium scoring, and the in-plane resolution was lower compared to typical CSCT, which both increased the partial volume effect.31 Due to partial volume effect, smaller calcifications may remain below the detection threshold and are not recognized as calcium.
The automated risk categorization, which is independent of the 130 HU threshold, gained a higher agreement with standard clinical risk categories from CSCT than manual calcium scoring in CTAC, which does rely on the detection threshold. Nevertheless, an automated method by Išgum et al that utilizes the 130 HU detection threshold reached a higher agreement with CSCT in risk categorization as compared to our automated risk categorization (rest: κ = 0.74 vs. κ = 0.65, respectively; stress κ = 0.70 vs. κ = 0.65, respectively).10 However, large differences in acquisition parameters (100 kV vs 120 kV; 3 mm vs 5 mm) hamper direct comparison of the results. This is underlined by the difference in agreement of manual calcium scoring in CTAC scans with CSCT: κ = 0.85 in the study of Išgum et al vs κ = 0.4 in our study. Nevertheless, the here presented method is not limited to the 5 mm CTAC data used in this study, but can also be applied to CT scans with other protocols.14,15 Since scans with 3 mm slice thickness allow better visualization of CAC lesions, we expect that the agreement of our method with CSCT scans improves when applied to scans with lower slice thickness.
According to conventional, visual CAC scoring methods, in the study by Einstein et al and Engbers et al 63% and 71% of CAC scores, respectively, were classified to a correct risk category.8,13 In our study, 65% of rest CTAC and 62% of stress CTAC scans analyzed with automated risk categorization were assigned to a correct risk category, which shows potential for further improvement. Importantly, as opposed to Einstein et al and Engebers et al, who used a 6-point risk scale,8,13 in our study a 5-point risk scale was applied, to facilitate comparison with previous works that performed manual and automatic calcium scoring in CTAC.9,10
The agreement between automated risk categories in CTAC and expert visual risk categorization in CSCT was lower in evaluation Set 2 compared to evaluation Set 1. In line with this, the agreement between visual scores in CTAC and visual scores in CSCT was lower than in Set 1. This underlines the challenges presented by the suboptimal acquisition protocol for calcium scoring of the CTAC scans, hampering visualization of lesions and sometimes even making them invisible in the CTAC scans. Future work could evaluate the performance of the method in CTAC scans with thinner slices compared to visual scoring.
As indicated by He et al, the magnitude of CAC and the stress-induced myocardial ischemia determined by PET and SPECT are positively correlated. Moreover, this relation was quantified by dividing the amount of CAC into previously used five risk groups. As a result, almost half of patients with CAC ≥ 400 were also diagnosed with myocardial ischemia.28 These findings were further supported in the meta-analysis which revealed that zero and low CAC score is rarely associated with ischemia.5 In our study the agreement in risk classification between automated risk categorization and manual reference scoring was moderate (κ = 0.65). Nevertheless, all CAC from the rest CTAC were correctly assigned to the ≥ 400 group by automated risk categorization. From stress CTAC scans, 4.7% was underestimated and classified into a lower risk category. This finding indicates that automated risk categorization may improve the likelihood assessment of myocardial ischemia in patients with marginal PET and SPECT results.
A zero CAC score is the most powerful negative predictor of cardiac events in an asymptomatic population of patients.32 Moreover, in symptomatic patients, who are referred to myocardial perfusion PET and SPECT scans, a low calcium score indicates a lower risk of CVD events.2 This is especially important for patients with normal PET and SPECT results, because the lack of myocardial ischemia does not rule out the presence of atherosclerotic disease. As indicated in our study, the sensitivity and specificity of CAC detection were good which indicates that automated risk categorization based on CTAC is a reliable method for CAC detection. Hence, CAC directly demonstrates the presence of the atherosclerotic process and it may help clinicians to identify patients of a higher cardiovascular risk and initiate a medical therapy, as specified in guidelines.2,3,4,11,33,34,35 Nevertheless, several patients had a false-negative result, mostly due to CAC lesions that are not visible on the CTAC scan. Moreover, several false-positive detections were found in image noise and ring artifacts. Automatic noise reduction36 and artifact removal37 may offer a solution.
Our study has several limitations. First, the automatic method is evaluated on a single-center dataset and the CTAC scans were acquired on one PET/CT scanner, therefore a direct comparison of performance with different CTAC protocols was not possible. Second, in this study not a 3 mm slice thickness but 5 mm slice thickness of CTAC scans was applied. Nevertheless, the results demonstrate a good agreement with scoring in CSCT scans which indicates feasibility of the approach. Moreover, we expect further improvement when applied on CTAC acquired with 3 mm slice thickness. Third, both the CSCT and the CTAC scans were not calibrated for CAC mass. However, we expect minor impact on the quantification and expect conclusions to remain the same if corrections would be applied. Fourth, the correspondence between calcifications detected on CTAC scans and CSCT scans was not investigated. Therefore, only patient-based analysis, not lesion-based analysis was performed.
Conclusion
We presented an automatic method for CAC quantification in CTAC that is based on visual assessment of CAC and independent of the CT-number threshold. The described automatic CAC quantification in CTAC improves the agreement with standard manual calcium scoring in CSCT compared with manual calcium scoring in CSCT using the threshold. Moreover, automatic risk categorization in CTAC improves agreement with reference Agatston risk categories in CSCT compared with manual calcium scoring in CTAC indicating potential for routine CVD risk assessment from CTAC, potentially relieving the need for dedicated CSCT.
New knowledge gained
Automatic CVD risk categorization based on visual assessment of CAC in CTAC scans shows improved agreement with risk categories determined on dedicated CSCT, as compared to standard manual calcium scoring in CTAC.
Abbreviations
- CAC:
-
Coronary artery calcification
- CTAC:
-
CT attenuation correction
- CSCT:
-
Calcium scoring CT
- PET:
-
Positron emission tomography
- CAD:
-
Coronary artery disease
- CVD:
-
Cardiovascular disease
- GAN:
-
Generative adversarial network
- CNN:
-
Convolutional neural network
References
Yuoness SA, Goha AM, Romsa JG, et al. Very high coronary artery calcium score with normal myocardial perfusion SPECT imaging is associated with a moderate incidence of severe coronary artery disease. Eur J Nucl Med Mol Imaging 2015;42:1542‐50. https://doi.org/10.1007/s00259-015-3072-z.
Chang SM, Nabi F, Xu J, et al. The coronary artery calcium score and stress myocardial perfusion imaging provide independent and complementary prediction of cardiac risk. J Am Coll Cardiol 2009;54:1872‐82. https://doi.org/10.1016/j.jacc.2009.05.071.
Lo-Kioeng-Shioe MS, Vavere AL, Arbab-Zadeh A, et al. Coronary calcium characteristics as predictors of major adverse cardiac events in symptomatic patients: Insights from the CORE320 Multinational Study. J Am Heart Assoc 2019;8:e007201. https://doi.org/10.1161/JAHA.117.007201.
Rozanski A, Berman DS. Coronary artery calcium scanning in symptomatic patients: Ready for use as a gatekeeper for further testing? J Nucl Cardiol 2017;24:835‐8. https://doi.org/10.1007/s12350-017-0794-2.
Bavishi C, Argulian E, Chatterjee S, Rozanski A. CACS and the frequency of stress-induced myocardial ischemia during MPI. JACC Cardiovasc Imaging 2016;9:580‐9. https://doi.org/10.1016/j.jcmg.2015.11.023.
Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol 1990;15:827‐32. https://doi.org/10.1016/0735-1097(90)90282-T.
Hecht HS. Coronary artery calcium scanning: Past, present, and future. JACC Cardiovasc Imaging 2015;8:579‐96. https://doi.org/10.1016/j.jcmg.2015.02.006.
Einstein AJ, Johnson LL, Bokhari S, et al. Agreement of visual estimation of coronary artery calcium from low-dose CT attenuation correction scans in hybrid PET/CT and SPECT/CT with Standard Agatston Score. J Am Coll Cardiol 2010;56:1914‐21. https://doi.org/10.1016/j.jacc.2010.05.057.
Mylonas I, Kazmi M, Fuller L, et al. Measuring coronary artery calcification using positron emission tomography-computed tomography attenuation correction images. Eur Heart J Cardiovasc Imaging 2012;13:786‐92. https://doi.org/10.1093/ehjci/jes079.
Išgum I, de Vos BD, Wolterink JM, et al. Automatic determination of cardiovascular risk by CT attenuation correction maps in Rb-82 PET/CT. J Nucl Cardiol 2017. https://doi.org/10.1007/s12350-017-0866-3.
Hecht HS, Cronin P, Blaha MJ, et al. 2016 SCCT/STR guidelines for coronary artery calcium scoring of noncontrast noncardiac chest CT scans: A report of the Society of Cardiovascular Computed Tomography and Society of Thoracic Radiology. J Cardiovasc Comput Tomogr 2017;11:74‐84. https://doi.org/10.1016/j.jcct.2016.11.003.
Hong C, Bae KT, Pilgram TK. Coronary artery calcium: Accuracy and reproducibility of measurements with multi-detector row CT—Assessment of effects of different thresholds and quantification methods. Radiology 2003;227:795‐801. https://doi.org/10.1148/radiol.2273020369.
Engbers EM, Timmer JR, Mouden M, et al. Visual estimation of coronary calcium on computed tomography for attenuation correction. J Cardiovasc Comput Tomogr 2016;10:327‐9. https://doi.org/10.1016/j.jcct.2016.04.002.
Velzen SGMV, Vos BD de, Verkooijen HM, Leiner T, Viergever MA, Išgum I. Coronary artery calcium scoring: Can we do better? In: Medical imaging 2020: Image processing, vol 11313. International Society for Optics and Photonics; 2020, p. 113130G. https://doi.org/10.1117/12.2549557.
van Velzen SGM, de Vos BD, Noothout JM, Verkooijen HM, Viergever MA, Išgum I. Generative models for reproducible coronary calcium scoring. J Med Imaging 2022;9(5):052406. https://doi.org/10.1117/1.JMI.9.5.052406.
Bom MJ, van Diemen PA, Driessen RS, et al. Prognostic value of [15O]H2O positron emission tomography-derived global and regional myocardial perfusion. Eur Heart J Cardiovasc Imaging 2020;21:777‐86. https://doi.org/10.1093/ehjci/jez258.
The National Lung Screening Trial Research Team. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med 2011;365:395‐409. https://doi.org/10.1056/NEJMoa1102873.
Lessmann N, van Ginneken B, Zreik M, et al. Automatic calcium scoring in low-dose chest CT using deep neural networks with dilated convolutions. IEEE Trans Med Imaging 2018;37:615‐25. https://doi.org/10.1109/TMI.2017.2769839.
van Velzen SGM, Lessmann N, Velthuis BK, et al. Deep learning for automatic calcium scoring in CT: Validation using multiple cardiac CT and Chest CT protocols. Radiology 2020;295:66‐79. https://doi.org/10.1148/radiol.2020191621.
de Vos BD, Wolterink JM, Leiner T, de Jong PA, Lessmann N, Išgum I. Direct automatic coronary calcium scoring in cardiac and chest CT. IEEE Trans Med Imaging 2019;38:2127‐38. https://doi.org/10.1109/TMI.2019.2899534.
Wolterink JM, Leiner T, Takx RAP, Viergever MA, Išgum I. Automatic coronary calcium scoring in non-contrast-enhanced ECG-triggered cardiac CT with ambiguity detection. IEEE Trans Med Imaging 2015;34:1867‐78. https://doi.org/10.1109/TMI.2015.2412651.
Rumberger JA, Kaufman L. A Rosetta stone for coronary calcium risk stratification: Agatston, volume, and mass scores in 11,490 individuals. Am J Roentgenol 2003;181:743‐8. https://doi.org/10.2214/ajr.181.3.1810743.
Zhu JY, Park T, Isola P, Efros AA. Unpaired image-to-image translation using cycle-consistent adversarial networks. 2017; p. 2223-32. http://openaccess.thecvf.com/content_iccv_2017/html/Zhu_Unpaired_Image-To-Image_Translation_ICCV_2017_paper.html. Accessed 5 July 2019.
Ohnesorge B, Flohr T, Fischbach R, et al. Reproducibility of coronary calcium quantification in repeat examinations with retrospectively ECG-gated multisection spiral CT. Eur Radiol 2002;12:1532‐40. https://doi.org/10.1007/s00330-002-1394-2.
Budoff MJ, Shaw LJ, Liu ST, et al. Long-term prognosis associated with coronary calcification: Observations from a registry of 25,253 patients. J Am Coll Cardiol 2007;49:1860‐70. https://doi.org/10.1016/j.jacc.2006.10.079.
IBM Corp. Released (2021). IBM SPSS statistics for Windows, version 28.0. Armonk: IBM Corp.
Sevrukov AB, Bland JM, Kondos GT. Serial electron beam CT measurements of coronary artery calcium: Has your patient’s calcium score actually changed? Am J Roentgenol 2005;185:1546‐53. https://doi.org/10.2214/AJR.04.1589.
He ZX, Hedrick TD, Pratt CM, et al. Severity of coronary artery calcification by electron beam computed tomography predicts silent myocardial ischemia. Circulation 2000;101:244‐51. https://doi.org/10.1161/01.CIR.101.3.244.
Kaster TS, Dwivedi G, Susser L, et al. Single low-dose CT scan optimized for rest-stress PET attenuation correction and quantification of coronary artery calcium. J Nucl Cardiol 2015;22:419‐28. https://doi.org/10.1007/s12350-014-0026-y.
Thomas CK, Mühlenbruch G, Wildberger JE, et al. Coronary artery calcium scoring with multislice computed tomography: In vitro assessment of a low tube voltage protocol. Invest Radiol 2006;41:668‐73. https://doi.org/10.1097/01.rli.0000233324.09603.dd.
Mühlenbruch G, Thomas C, Wildberger JE, et al. Effect of varying slice thickness on coronary calcium scoring with multislice computed tomography in vitro and in vivo. Investig Radiol 2005;40:695‐9. https://doi.org/10.1097/01.rli.0000179523.07907.a6.
Blaha MJ, Cainzos-Achirica M, Greenland P, et al. Role of coronary artery calcium score of zero and other negative risk markers for cardiovascular disease. Circulation 2016;133:849‐58. https://doi.org/10.1161/CIRCULATIONAHA.115.018524.
Mach F, Baigent C, Catapano AL, et al. 2019 ESC/EAS guidelines for the management of dyslipidaemias: Lipid modification to reduce cardiovascular risk: The task force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and European Atherosclerosis Society (EAS). Eur Heart J 2020;41:111‐88.
Nasir K, Bittencourt MS, Blaha MJ, et al. Implications of coronary artery calcium testing among statin candidates according to American College of Cardiology/American Heart Association Cholesterol Management guidelines: MESA (Multi-Ethnic Study of Atherosclerosis). J Am Coll Cardiol 2015;66:1657‐68. https://doi.org/10.1016/j.jacc.2015.07.066.
Grundy SM, Stone NJ, Bailey AL, et al. AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: Executive summary: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2019;139:e1046‐81. https://doi.org/10.1161/CIR.0000000000000624.
Wolterink JM, Leiner T, Viergever MA, Išgum I. Generative adversarial networks for noise reduction in low-dose CT. IEEE Trans Med Imaging 2017;36:2536‐45. https://doi.org/10.1109/TMI.2017.2708987.
Liang X, Zhang Z, Niu T, et al. Iterative image-domain ring artifact removal in cone-beam CT. Phys Med Biol 2017;62:5276‐92. https://doi.org/10.1088/1361-6560/aa7017.
Acknowledgements
The authors gratefully acknowledge the Dutch Cancer Society for the financial support (NCT03206333). The authors thank the National Cancer Institute for access to NCI’s data collected by the National Lung Screening Trial. The statements contained herein are solely those of the authors and do not represent or imply concurrence or endorsement by NCI.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
S.G.M. van Velzen, M.M. Dobrolinska, P. Knaapen, R.L.M. van Herten, R. Jukema, I. Danad, R.H.J.A. Slart, M.J.W. Greuter, and I. Išgum declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The authors of this article have provided a PowerPoint file, available for download at SpringerLink, which summarizes the contents of the paper and is free for re-use at meetings and presentations. Search for the article DOI on SpringerLink.com.
Funding
M.M.D. received the “EACVI Research Grant 2020” and “Specialized Research Fellowship 2019 Grant from “Club 30” and Polish Cardiac Society.”
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
van Velzen, S.G.M., Dobrolinska, M.M., Knaapen, P. et al. Automated cardiovascular risk categorization through AI-driven coronary calcium quantification in cardiac PET acquired attenuation correction CT. J. Nucl. Cardiol. 30, 955–969 (2023). https://doi.org/10.1007/s12350-022-03047-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-022-03047-9