Abstract
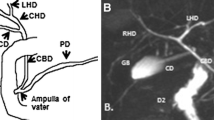
Congenital biliary dilatation (CBD) is a congenital malformation of focal dilatation of the extrahepatic bile ducts, including the common bile duct, and is often associated with pancreaticobiliary maljunction (PBM). In this article, we report a CBD case that presented with focal dilation of the common bile duct without PBM (Todani’s classification type Ib). The patient was a 32-year-old man who visited a doctor with a chief complaint of abdominal distension. Computed tomography revealed cystic dilatation of the common bile duct, and the patient was referred to our institution. Magnetic resonance cholangiopancreatography showed cystic dilatation of the common bile duct with a maximum diameter of 7 cm; however, evaluating the presence of PBM was challenging. Endoscopic ultrasonography showed small gallstones and debris in the dilated common bile duct and no thickening of the gallbladder wall. Endoscopic retrograde cholangiopancreatography revealed no PBM or markedly elevated bile amylase levels. Based on these findings, the patient was diagnosed with Todani Type Ib CBD. Since this patient did not have pancreatobiliary reflux, it was unclear whether the risk of developing biliary tract cancer was high, and since the treatment was highly invasive, the decision was to follow up without surgical treatment.





Similar content being viewed by others
References
Alonso-Lej F, Rever WB Jr, Pessagno DJ. Congenital choledochal cysts, with a report of 2 and an analysis of 94 cases. Int Abstr Surg. 1959;108:1–30.
Todani T, Watanabe Y, Narusue M, et al. Congenital bile duct cysts: classification, operative procedures, and review of thirty-seven cases including cancer arising from choledochal cyst. Am J Surg. 1977;134:263–9.
Todani T. Congenital choledochal dilatation: classification, clinical features, and long-term results. J Hep Bil Pancr Surg. 1997;4:276–82.
Hamada Y, Ando H, Kamisawa T, et al. Diagnostic criteria for congenital biliary dilatation 2015. J Hepatobiliary Pancreat Sci. 2016;23:342–6.
Takauji S, Obara M, Koizumi K, et al. Case with Todani’s type Ib congenital cystic dilatation of the common bile duct. Nihon Shokakibyo Gakkai Zasshi. 2008;105:391–6 ((in Japanese)).
Tashiro S, Imaizumi T, Ohkawa H, et al. Pancreaticobiliary maljunction: retrospective and nationwide survey in Japan. J Hepatobiliary Pancreat Surg. 2003;10:345–51.
Morine Y, Shimada M, Takamatsu H, et al. Clinical features of pancreaticobiliary maljunction: update analysis of 2nd Japan-nationwide survey. Hepatobiliary Pancreat Sci. 2013;20:472–80.
Jesudason SR, Jesudason MR, Mukha RP, et al. Management of adult choledochal cysts–a 15-year experience. HPB (Oxford). 2006;8:299–305.
Morine Y, Mori H, Utsunomiya T, et al. Epidemiology and clinical features of pancreaticobiliary maljunction. 2011;25:133-40 (in Japanese with English abstract).
Irie H, Honda H, Jimi M, et al. Value of MR cholangiopancreatography in evaluating choledochal cysts. AJR Am J Roentgenol. 1998;171:1381–5.
Park DH, Kim MH, Lee SK, et al. Can MRCP replace the diagnostic role of ERCP for patients with choledochal cysts? Gastrointest Endosc. 2005;62:360–6.
Suzuki M, Shimizu T, Kudo T, et al. Usefulness of nonbreath-hold 1-shot magnetic resonance cholangiopancreatography for the evaluation of choledochal cyst in children. J Pediatr Gastroenterol Nutr. 2006;42:539–44.
Huang CT, Lee HC, Chen WT, et al. Usefulness of magnetic resonance cholangiopancreatography in pancreatobiliary abnormalities in pediatric patients. Pediatr Neonatol. 2011;52:332–6.
Fumino S, Ono S, Kimura O, et al. Diagnostic impact of computed tomography cholangiography and magnetic resonance cholangiopancreatography on pancreaticobiliary maljunction. J Pediatr Surg. 2011;46:1373–8.
Itokawa F, Kamisawa T, Nakano T, et al. Exploring the length of the common channel of the pancreaticobiliary maljunction on magnetic resonance cholangiopancreatography. J Hepatobiliary Pancreat Sci. 2015;22:68–73.
Huang SG, Guo WL, Wang J, et al. Factors interfering with delineation on MRCP of pancreaticobiliary maljunction in paediatric patients. PLoS ONE. 2016;11: e0154178.
Kamisawa T, Ando H, Suyama M, et al. Japanese clinical practice guidelines for pancreaticobiliary maljunction. J Gastroenterol. 2012;47:731–59.
Kamisawa T, Takuma K, Anjiki H, et al. Pancreaticobiliary maljunction. Clin Gastroenterol Hepatol. 2009;7:S84–8.
Fujii H, Yang Y, Tang R, et al. Epithelial cell proliferation activity of the biliary ductal system with congenital biliary malformations. Hepatobiliary Pancreat Surg. 1999;6:294–302.
Hanada K, Itoh M, Fujii K, et al. Pathology and cellular kinetics of the gallbladder with anomalous junction of the pancreaticobiliary duct. Am J Gastroenterol. 1996;91:1007–11.
Tanno S, Obara T, Fujii T, et al. Proliferative potential and K-ras mutation in epithelial hyperplasia of the gallbladder in patients with anomalous pancreaticobiliary ductal union. Cancer. 1998;83:267–75.
Sugai M, Ishido K, Endoh M, et al. Sonographic demonstration of the wall thickness of the gallbladder in pediatric patients with pancreatico-biliary maljunction. J Hepatobiliary Pancreat Sci. 2010;17:345–8.
Tsunoda T, Furui J, Yamada M, et al. Caroli’s disease associated with hepatolithiasis: a case report and review of the Japanese literature. Gastroenterol Jpn. 1991;26:74–9.
Millwala F, Segev DL, Thuluvath PJ. Caroli’s disease and outcomes after liver transplantation. Liver Transpl. 2008;14:11–7.
Mabrut JY, Kianmanesh R, Nuzzo G, et al. Surgical management of congenital intrahepatic bile duct dilatation, Caroli’s disease, and syndrome: long-term results of the French Association of Surgery Multicenter Study. Ann Surg. 2013;258:713–21.
Malhi H, Gores GJ. Cholangiocarcinoma: modern advances in understanding a deadly old disease. J Hepatol. 2006;45:856–67.
Ishibashi H, Shimada M, Kamisawa T, et al. Japanese clinical practice guidelines for congenital biliary dilatation. J Hepatobiliary Pancreat Sci. 2017;24:1–16.
Acknowledgements
The authors would like to thank Editage (www.editage.jp) for the English language editing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Human/animal rights
All procedures were performed per the ethical standards of the 1964 Declaration of Helsinki and its amendments.
Informed consent
The patient presented in this study provided informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kiyoshita, Y., Ishii, Y., Serikawa, M. et al. A case of congenital biliary dilatation without pancreaticobiliary maljunction, so-called Type Ib according to Todani’s classification. Clin J Gastroenterol 17, 177–182 (2024). https://doi.org/10.1007/s12328-023-01873-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12328-023-01873-z