Abstract
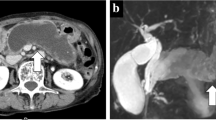
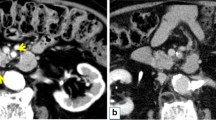
Post-transplant patients reportedly have a higher risk of de novo neoplasms. However, intraductal papillary mucinous neoplasm (IPMN) of the native pancreas after pancreas transplantation (PTx) has not been well investigated. The choice of treatment, especially invasive treatment, for de novo neoplasms in transplant patients should consider their impaired immunity. In this context, we present a case of IPMN developing in the native pancreas of a PTx patient. A 53-year-old man underwent a follow-up abdominal computed tomography scan 6 years after a simultaneous pancreas-kidney transplant for type 1 diabetes mellitus with end-stage diabetic nephropathy requiring hemodialysis. The scan revealed IPMN in the pancreas head; an enhancing internal solid component suggested a high risk of malignancy, indicating surgical resection. Partial pancreatectomy or pancreaticoduodenectomy was anatomically indicated, but considering the insulin-secreting ability of the transplanted pancreas and the potential high risk of postoperative pancreatic fistula due to immune impairment after partial pancreatectomy, total pancreatectomy (TP) was performed. The patient is alive with good pancreas graft function, no signs of indigestion for 18 months after TP, and no evidence of IPMN recurrence. This report should help clinicians characterize de novo IPMN in the native pancreas and determine IPMN therapeutic options for transplant patients.



Similar content being viewed by others
References
Tomimaru Y, Ito T, Kenmochi T. The registry of Japanese pancreas and islet transplantation. Ishoku. 2020;2020(55):277–83.
Tomimaru Y, Eguchi H, Doki Y, et al. Current state of pancreas transplantation in Japan based on the nationwide registry. Ann Gastroenterol Surg. 2021;00:1–8.
Tomimaru Y, Ito T, Marubashi S, et al. De novo malignancy after pancreas transplantation in Japan. Transplant Proc. 2015;47:742–5.
de Mier MVP-R, Aguera ML, Navarro MD, et al. Prevalence and survival of cancer after pancreas-kidney transplantation. Transplant Proc. 2018;50:669–72.
Manzia TM, Angelico R, Gazia C, et al. De novo malignancies after liver transplantation: the effect of immunosuppression-personal data and review of literature. World J Gastroenterol. 2019;25:5356–75.
Kim S, Rovgaliyev B, Lee JM, et al. Clinical significance of de novo malignancy after liver transplant: a single-center study. Transplant Proc. 2021;53:200–6.
Sanaei AK, Aliakbarian M, Kazemi K, et al. De novo malignancy after liver transplant. Exp Clin Transplant. 2015;13:163–6.
Santangelo M, Clemente M, Spiezia S, et al. Wound complications after kidney transplantation in nondiabetic patients. Transplant Proc. 2009;41:1221–3.
Lau NS, Ahmadi N, Verran D. Abdominal wall complications following renal transplantation in adult recipients—factors associated with interventional management in one unit. BMC Surg. 2019;19:10.
Ohashi K, Murakami Y, Maruyama M, et al. Four cases of mucus-secreting pancreatic cancer (in Japanese). Prog Digest Endosc. 1982;20:348–51.
Klöppel G, Solcia E, Longnecker D, et al. Histological typing of tumours of the exocrine pancreas. In: International histological classification of tumours. 2nd ed. Berlin: Springer-Verlag; 1996.
Hruban RH, Takaori K, Klimstra DS, et al. An illustrated consensus on the classification of pancreatic intraepithelial neoplasia and intraductal papillary mucinous neoplasms. Am J Surg Pathol. 2004;28:977–87.
Oyama H, Tada M, Takagi K, et al. Long-term risk of malignancy in branch-duct intraductal papillary mucinous neoplasms. Gastroenterology. 2020;158:226–37.
Al-Qaoud TM, Martinez EJ, Sollinger HW, et al. Prevalence and outcomes of cystic lesions of the transplant pancreas: The University of Wisconsin Experience. Am J Transplant. 2018;18:467–77.
Darstein F, Konig C, Hoppe-Lotichius M, et al. Impact of pancreatic comorbidities in patients with end-stage liver disease on outcome after liver transplantation. Eur J Intern Med. 2014;25:281–5.
Branchi V, Lingohr P, Willinek WA, et al. Extensive multifocal branch duct IPMN of the pancreas after liver transplantation: is surgery justified? Eur J Med Res. 2015;20:26.
Vidhyarkorn S, Siripongsakun S, Yu J, et al. Longterm follow-up of small pancreatic cystic lesions in liver transplant recipients. Liver Transpl. 2017;23:324–9.
Jie T, Harmon JV Jr, Gulbahce HE, et al. Intraductal papillary mucinous tumor of the native pancreas in a pancreas-kidney transplant recipient. Pancreas. 2004;28:446–9.
Tanaka M. Clinical management and surgical decision-making of IPMN of the pancreas. Methods Mol Biol. 2019;1882:9–22.
Chapman JR, Webster AC, Wong G. Cancer in the transplant recipient. Cold Spring Harb Perspect Med. 2013;3(7):a015677.
Hoshida Y, Tsukuma H, Yasunaga Y, et al. Cancer risk after renal transplantation in Japan. Int J Cancer. 1997;71:517–20.
Kasiske BL, Snyder JJ, Gilbertson DT, et al. Cancer after kidney transplantation in the United States. Am J Transplant. 2004;4:905–13.
Sanchez EQ, Marubashi S, Jung G, et al. De novo tumors after liver transplantation: a single-institution experience. Liver Transpl. 2002;8:285–91.
Miyazaki T, Sato S, Kondo T, et al. National survey of de novo malignancy after solid organ transplantation in Japan. Surg Today. 2018;48:618–24.
Nasser-Ghodsi N, Mara K, Watt KD. De novo colorectal and pancreatic cancer in liver transplant recipients: identifying the higher risk populations. Hepatology. 2021;74(2):1003–13.
Zhou J, Hu Z, Zhang Q, et al. Spectrum of de novo cancers and predictors in liver transplantation: analysis of the scientific registry of transplant recipients database. PLoS ONE. 2016;11:e0155179.
Roza AM, Johnson C, Juckett M, et al. Adenocarcinoma arising in a transplanted pancreas. Transplantation. 2001;72:1156–7.
Casadei R, Ricci C, Taffurelli G, et al. Prospective validation of a preoperative risk score model based on pancreatic texture to predict postoperative pancreatic fistula after pancreaticoduodenectomy. Int J Surg. 2017;48:189–94.
van Hilst J, de Rooij T, van den Boezem PB, et al. Laparoscopic pancreatoduodenectomy with open or laparoscopic reconstruction during the learning curve: a multicenter propensity score matched study. HPB (Oxford). 2019;21:857–64.
Rungsakulkij N, Mingphruedhi S, Tangtawee P, et al. Risk factors for pancreatic fistula following pancreaticoduodenectomy: a retrospective study in a Thai tertiary center. World J Gastrointest Surg. 2017;9:270–80.
van Roessel S, Mackay TM, Tol J, et al. Impact of expanding indications on surgical and oncological outcome in 1434 consecutive pancreatoduodenectomies. HPB (Oxford). 2019;21:865–75.
Pedrazzoli S. Pancreatoduodenectomy (PD) and postoperative pancreatic fistula (POPF): a systematic review and analysis of the POPF-related mortality rate in 60,739 patients retrieved from the English literature published between 1990 and 2015. Medicine (Baltimore). 2017;96:e6858.
Chen JS, Liu G, Li TR, et al. Pancreatic fistula after pancreaticoduodenectomy: risk factors and preventive strategies. J Cancer Res Ther. 2019;15:857–63.
Barkin JA, Westermann A, Hoos W, et al. Frequency of appropriate use of pancreatic enzyme replacement therapy and symptomatic response in pancreatic cancer patients. Pancreas. 2019;48:780–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008(5).
Informed consent
Informed consent was obtained from all patients included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sato, H., Tomimaru, Y., Akita, H. et al. A case of intraductal papillary mucinous neoplasm developing in the native pancreas after pancreas transplantation treated by total pancreatectomy. Clin J Gastroenterol 14, 1766–1771 (2021). https://doi.org/10.1007/s12328-021-01517-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12328-021-01517-0