Abstract
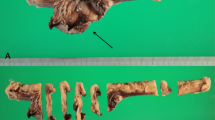
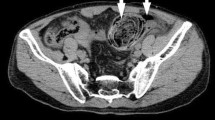
Gastrointestinal stromal tumors (GISTs) are the most common mesenchymal tumor of the human gastrointestinal tract. They usually develop in the stomach and small intestine, but extremely rarely in the colon. Although most GISTs form a mass, some cases showing a flatly proliferating lesion called planar-type GIST have been reported in the sigmoid colon and small intestine. Those are often associated with diverticular lesion and/or perforation. We present here a case of planar-type GIST of the transverse colon with perforation. A 49-year-old Japanese woman abruptly complained of abdominal pain, and was clinically diagnosed as perforation of the transverse colon. Partial resection of the transverse colon including the perforated site was done, and no apparent mass lesion was present. Histology showed that spindle cells flatly proliferated around the perforated area and replaced the layers from submucosa to subserosa. Immunohistochemistry revealed that the spindle cells were KIT-, DOG1- and CD34-positive. Codons 557 and 558 of exon 11 of the c-kit gene were heterozygously deleted at the lesional tissue but not at the normal mucosal tissue. Planar-type GIST of the transverse colon has not been reported yet, and the literature search for the similar cases was done.




Similar content being viewed by others
References
Hirota S, Isozaki K, Moriyama Y, et al. Gain-of-function mutations of c-kit in human gastrointestinal stromal tumors. Science. 1998;279:577–80.
Hirota S, Ohashi A, Nishida T, et al. Gain-of-function mutations of platelet-derived growth factor receptor α gene in gastrointestinal stromal tumors. Gastroenterology. 2003;125:660–7.
Heinrich MC, Corless CL, Duensing A, et al. PDGFRA activating mutations in gastrointestinal stromal tumors. Science. 2003;299:708–10.
Janeway KA, Kim SY, Lodish M, et al. Defects in succinate dehydrogenase in gastrointestinal stromal tumors lacking KIT and PDGFRA mutations. Proc Natl Acad Sci USA. 2011;108:314–8.
Miranda C, Nucifora M, Molinari F, et al. KRAS and BRAF mutations predict primary resistance to imatinib in gastrointestinal stromal tumors. Clin Cancer Res. 2012;18:1769–76.
Nishida T, Tsujimoto M, Takahashi T, et al. Gastrointestinal stromal tumors in Japanese patients with neurofibromatosis type I. J Gastoenterol. 2016;51:571–8.
Edge SB, Byrd DR, Compton CC, et al. AJCC cancer staging manual. 7th ed. New York: Springer; 2010.
Hirota S, Okazaki T, Kitamura Y, et al. Cause of familial and multiple gastrointestinal autonomic tumor with hyperplasia of interstitial cells of Cajal is germline mutation of the c-kit gene. Am J Surg Pathol. 2002;24:326–7.
Agaimy A, Märkl B, Arnholdt H, et al. Sporadic segmental interstitial cell of Cajal hyperplasia (microscopic GIST) with unusual diffuse longitudinal growth replacing the muscularis propria: differential diagnosis to hereditary GIST syndromes. Int J Clin Exp Pathol. 2010;3:549–56.
Xue L, Qiu T, Song Y, et al. Long segmental hyperplasia of interstitial cells of Cajal with giant diverticulum formation. Int J Clin Exp Pathol. 2013;6:2989–96.
Ikemura M, Kunita A, Miwa Y, et al. Gut wall replacing type of gastrointestinal stromal tumor presenting as a perforation of the ileal diverticulum. Pathol Res Pract. 2015;211:892–5.
Hanada M, Takahashi Y, Ikeda K. Gastrointestinal stromal tumor (GIST) of the sigmoid colon presenting as megacolon with fecaloma: a hither undescribed presentation caused by diffuse muscular infiltration by GIST. J Toyonaka Munic Hosp. 2003;4:83–9.
Yamashita D, Usami Y, Toyosawa S, et al. A case of diffuse infiltrating gastrointestinal stromal tumor of sigmoid colon with perforation. Pathol Int. 2014;64:34–8.
Ueno G, Maeda T, Arima R, et al. A planar gastrointestinal stromal tumor replacing the proper muscle layer causing fecaloma and perforation in the sigmoid colon: a case report and literature review. Clin J Gastroenterol. 2014;7:328–32.
Shintaku Y, Asano Y, Watanabe T, et al. A case of planar-type GIST of the sigmoid colon showing diverticular structure with perforation. World J Surg Oncol. 2020;18:125.
Miettinen M, Sarlomo-Rikala M, Sobin LH, et al. Gastrointestinal stromal tumors and leiomyosarcomas in the colon: a clinicopathologic, immunohistochemical, and molecular genetic study of 44 cases. Am J Surg Pathol. 2000;24:1339–52.
Feng F, Tian Y, Liu Z, et al. Clinicopathological features and prognosis of colonic gastrointestinal stromal tumors: evaluation of a pooled case series. Oncotarget. 2016;7:40735–45.
Hagger R, Gharaie S, Finlayson C, et al. Regional and transmural density of interstitial cells of Cajal in human colon and rectum. Am J Physiol. 1998;275:G1309–16.
Gomez-Pinilla PJ, Gibbons SJ, Sarr MG, et al. Changes in interstitial cells of cajal with age in the human stomach and colon. Neurogastroenterol Motil. 2011;23:36–44.
Yan L, Zou L, Zhao W, et al. Clinicopathological significance of c-KIT mutation in gastrointestinal stromal tumors: a systematic review and meta-analysis. Sci Rep. 2015;5:13718.
Wang HC, Li TY, Chao YJ, et al. KIT exon 11 codons 557–558 deletion mutation promotes liver metastasis through the CXCL12/CXCR4 axis in gastrointestinal stromal tumors. Clin Cancer Res. 2016;22:3477–87.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Human/animal rights
All procedures followed have been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Informed consent
Informed consent was obtained from all patients to be included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yamauchi, A., Chinen, Y., Chihara, T. et al. A case of planar-type gastrointestinal stromal tumor of the transverse colon with perforation. Clin J Gastroenterol 14, 1157–1162 (2021). https://doi.org/10.1007/s12328-021-01385-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12328-021-01385-8