Abstract
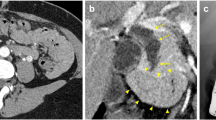
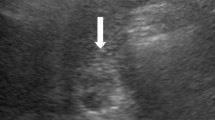
A 59-year-old man with anorexia who had a history of cholecystectomy was referred to our hospital. Imaging examinations revealed a contrast-enhanced tumor in the residual cystic duct and a part of the common bile duct. Endoscopic retrograde cholangiopancreatography and peroral-cholangioscopy showed a papillary tumor with movement and a change in the shape. Under a diagnosis of primary cystic duct cancer, subtotal stomach-preserving pancreaticoduodenectomy was performed. The microscopic examination of a resected specimen revealed intracholecystic papillary-tubular neoplasm located in the residual cystic duct, forming a polypoid protrusion to the common bile duct and extensive intraepithelial progress in the common bile duct.









Similar content being viewed by others
References
Zen Y, Fujii T, Itatsu K, et al. Biliary papillary tumors share pathological features with intraductal papillary mucinous neoplasm of the pancreas. Hepatology. 2006;44:1333–43.
Adsay V, Jang KT, Roa JC, et al. Intracholecystic papillary-tubular neoplasms (ICPN) of the gallbladder (neoplastic polyps, adenomas, and papillary neoplasms that are ≥ 1.0 cm): clinicopathologic and immunohistochemical analysis of 123 cases. Am J Surg Pathol. 2012;36:1279–301.
Japanese society of hepato-biliary-pancreatic surgery. General rules for clinical and pathological studies on cancer of the biliary tract, 6th ed. Kanehara Shuppan; 2013.
Farrar DA. Carcinoma of the cystic duct. Br J Surg. 1951;39:183–5.
Ozden I, Kamiya J, Nagino M, et al. Cystic duct carcinoma: a proposal for a new “working definition”. Langenbecks Arch Surg. 2003;387:337–42.
Hashimoto S, Horaguchi J, Fujita N, et al. Intracholecystic papillary-tubular neoplasm of the gallbladder presenting with jaundice. Intern Med. 2014;53:2313–7.
Nakanuma Y, Kubota K. Subclassification of intraductal papillary neoplasm of bile duct (IPNB)—proposal by Japan–Korea Study Group on IPNB from pathological stand points of view. Biliary Tract. 2017;31:390.
Furukawa T, Hatori T, Fujita I, et al. Prognostic relevance of morphological types of intraductal papillary mucinous neoplasms of the pancreas. Gut. 2011;60:509–16.
Wan X, Shi J, Whang A, et al. Gallbladder papillary neoplasms share pathological features with intraductal papillary neoplasm of the bile duct. Oncotarget. 2017;8:31532–9.
Sakamoto E, Hayakawa N, Kamiya J, et al. Treatment strategy for mucinous-producing intrahepatic cholangiocarcinoma: Value of percutaneous transhepatic biliary drainage and cholangioscopy. World J Surg. 1999;23:1038–44.
Yeh TS, Tseng JH, Chiu CT, et al. Cholangiographic spectrum of intraductal papillary mucinous neoplasm of the bile ducts. Ann Surg. 2006;244:248–53.
Jung G, Park KM, Lee SS, et al. Long-term clinical outcome of the surgically resected intraductal papillary neoplasm of the bile duct. J Hepatol. 2012;57:787–93.
Noda Y, Fujita N, Kobayashi G, et al. Intraductal ultrasonography before biliary drainage and transpapillary biopsy in assessment of the longitudinal extent of bile duct cancer. Dig Endosc. 2008;20:73–8.
Ogawa T, Ito K, Koshita S, et al. Usefulness of cholangioscopic-guided mapping biopsy using SpyGlass DS for preoperative evaluation of extrahepatic cholangiocarcinoma: a pilot study. Endosc Int Open. 2018;6:E199–204.
Sakai Y, Tsuyuguchi T, Ishihara T, et al. Usefulness of peroral cholangioscopy in preoperative diagnosis of intraductal papillary neoplasm of the bile duct. Hepatogastroenterology. 2010;57:691–3.
Osanai M, Itoi T, Igarashi Y, et al. Peroral video cholangioscopy to evaluate indeterminate bile duct lesions and preoperative mucosal cancerous extension: a prospective multicenter study. Endoscopy. 2013;45:635–42.
Nishikasa T, Tsuyuguchi T, Sakai Y, et al. Preoperative assessment of longitudinal extension of cholangiocarcinoma with peroral video-cholangioscopy: a prospective study. Dig Endosc. 2014;26:450–7.
Kawakami H, Kuwatani M, Etoh K, et al. Endoscopic retrograde cholangiography versus peroral cholangioscopy to evaluate intraepithelial tumor spread in biliary cancer. Endoscopy. 2009;41:959–64.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Human rights
All procedures followed have been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Informed consent
Informed consent was obtained from all patients for being included in the study
Rights and permissions
About this article
Cite this article
Fujii, Y., Noda, Y., Koshita, S. et al. Intracholecystic papillary-tubular neoplasm of the gallbladder originating in the cystic duct with extensive intraepithelial progress in the common bile duct. Clin J Gastroenterol 12, 197–204 (2019). https://doi.org/10.1007/s12328-018-0927-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12328-018-0927-4