Abstract
Introduction
There is a medical need for a safe, effective nonopioid postoperative analgesic for older subjects, including those with mild to moderate renal impairment.
Methods
Participants (≥ 65 years) were stratified by no, mild, or moderate renal impairment defined as creatinine clearance 60–89 mL/min for mild and 30–59 mL/min for moderate. Subjects were randomized to receive a loading dose of 6.25 mg of ketorolac tromethamine drug candidate NTM-001 followed by a 1.75 mg/h continuous intravenous (IV) infusion over 24 h or an IV bolus injection of ketorolac tromethamine (KETO-BOLUS) of 15 mg every 6 h. There were four treatment periods of 24 h for each subject with a minimum 7-day washout between them. This was a crossover study so subjects served as their own controls. Blood drawn from the subjects was used to plot concentration–time profiles against target profiles. Adverse events were monitored.
Results
Thirty-nine subjects enrolled. Concentration–time profiles showed low intersubject variability. Model-predicted curves for those with renal impairment closely matched observed plasma concentrations. Continuous infusion maintained higher mean plasma concentrations than the bolus regimen. No serious or unexpected adverse events were observed. No deaths occurred.
Conclusions
NTM-001 was considered safe and well tolerated in this population of participants ≥ 65 years, including in those with mild or moderate renal impairment. There were fewer adverse events in the continuous infusion group. The predictable pharmacologic properties and blood concentration levels suggest that continuous IV infusion of ketorolac can be used as an effective postoperative pain reliever in older subjects.
Plain Language Summary
Controlling postoperative pain can lead to faster recovery. Ketorolac tromethamine is a nonsteroidal anti-inflammatory drug (NSAID), like ibuprofen and naproxen, that can be as effective as morphine without the same risks. In hospitals, ketorolac is usually administered intravenously (IV) either continuously or as a bolus injection. A bolus of ketorolac may result in adverse gastrointestinal side effects. In this study, a new formulation of ketorolac tromethamine, NTM-001, was administered IV as a continuous 24 h infusion compared to IV boluses of ketorolac tromethamine every 6 h in volunteers. Volunteers were older (≥ 65 years) and had no, mild, or moderate kidney dysfunction. One randomized group received a starting IV dose of 6.26 mg followed by a continuous IV infusion of 1.75 mg/h of over 24 h. The other group received single NTM-001 IV bolus injections of ketorolac tromethamine 15 mg every 6 h over 24 h (4 doses, 60 mg) over the 24 h. After completing the first study, subjects waited at least a week and then switched groups, giving the study a crossover design so it could be observed how each subject responded to both regimens. Blood drawn from the subjects was tested for standard pharmacokinetic (PK) parameters. The data show that blood concentrations of NTM-001 can be reliably predicted. Side effects were mild and the continuous infusion reduced side effects. No unexpected adverse events occurred. These data show that NTM-001 can be used safely in older individuals, including those with mild or moderate kidney impairment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why do this study? |
Opioids are effective pain relievers, but they often have treatment-limiting side effects and are associated with tolerance, dependence, and opioid use disorder. |
An equally effective but safer analgesic is needed for postoperative pain, particularly for patients ≥ 65 years with mild to moderate renal compromise. |
A prior study found that NTM-001, a novel formulation of ketorolac tromethamine, had reliable pharmacokinetic (PK) and pharmacodynamic (PD) properties in healthy young volunteer subjects. |
What did the study ask? |
The study asked whether NTM-001 or ketorolac tromethamine would be safe and exhibit predictable pharmacological properties in participants ≥ 65 years with and without renal impairment. |
The study looked at two groups. One group received a loading dose and then continuous infusion of NTM-001 while the other group received bolus intravenous (IV) dosing of ketorolac tromethamine every 6 h. |
This was a crossover study, so subjects served as their own controls. |
What did the study find? |
NTM-001 was found to be safe in this population. There were no serious adverse events, no unexpected adverse events, and the continuous infusion group had fewer adverse events than the bolus group. |
Blood concentration levels were predictable in both groups but the continuous infusion group had higher mean blood concentration levels over 24 h. |
What was learned? |
The use of intravenously administered NTM-001 and ketorolac tromethamine was safe in participants ≥ 65 years, even those with mild to moderate kidney dysfunction. The continuous infusion group using NTM-001 had lower variability in plasma concentrations and fewer adverse events. |
Introduction
While opioids are effective analgesics, their use and widespread prescribing has been associated with the public health crisis of opioid overdose and opioid use disorder [1]. The use of nonopioid analgesics for perioperative pain control has been advocated and would eliminate or at least reduce the need for opioids in the postoperative hospital setting [2]. Finding the optimal nonopioid analgesic for postoperative pain has been an important and sometimes frustrating search.
Ketorolac tromethamine is a nonsteroidal anti-inflammatory drug (NSAID) indicated for use in both adult and pediatric patients for treatment of moderate to severe pain including postoperative pain. Like other NSAIDs, ketorolac has been associated with gastrointestinal and cardiovascular adverse events that have limited its utility, particularly at high doses or for courses more than 5 days in duration [3].
The population in many developed nations is aging, and older patients often require surgery at rates higher than the general population [4]. With age come physical changes, including diminished kidney function that can complicate prescribing choices and increase the risks of surgery [5]. The rates of chronic kidney disease increase with advancing age and it is increasing with time as well, so that its prevalence is greater since 1999 than it was before [6]. About 40% of the population age 65 or older has some form of kidney dysfunction [6], which can complicate care and necessitates dosing changes of many medications.
A novel alcohol-free formulation of ketorolac has been developed for continuous IV infusion for 24 h. This product (NTM-001, Neumentum, Summit, New Jersey, USA) is available in a premixed bag. A pharmacokinetic (PK) first-in-human study was carried out in subjects ≥ 65 years of age with no, mild, or moderate degrees of renal impairment. The purpose of this randomized, open-label, crossover study was to evaluate the PK properties, bioavailability, and exposure of NTM-001 versus an IV bolus regimen of ketorolac tromethamine; to explore dose regimens and assess PK parameters; and to evaluate the safety of NTM-001 compared to IV bolus ketorolac. Note that for elderly or renally compromised subjects, dosing was reduced to help mitigate potential risks.
Methods
This was a multicenter, randomized, open-label, crossover study. Inclusion criteria for subjects required they be ≥ 65 years without severe renal impairment. Subjects were then stratified by no, mild, or moderate renal impairment. Renal function was defined by creatinine clearance. Those with no renal impairment had creatinine clearance > 90 mL/min. Creatinine clearance between 60 and 89 mL/min defined mild renal impairment, while creatinine clearance of 30–59 mL/min defined moderate renal impairment. Subjects with creatinine clearance < 30 mL/min were excluded.
This was a prospective study. Subjects were randomized to receive an intravenously administered bolus dosing regimen of ketorolac tromethamine (reference) or a loading dose/continuous infusion of intravenously administered NTM-001. Based on the approved ketorolac IV bolus dosing regimen of 15 mg every 6 h or 60 mg over 24 h, the continuous infusion group used a 6.25 mg loading dose of NTM-001 followed immediately by continuous infusion of 1.75 mg/h delivered using a preprogrammed conventional infusion pump. NTM-001 was administered as a continuous IV infusion over 24 h. Based on a model of ketorolac injection, an exposure–response modeling and simulation were employed to predict the time course of drug exposure and its analgesic effect, comparing NTM-001 to a reference regimen of IV bolus ketorolac tromethamine doses of 15 mg every 6 h over 24 h.
Subjects were stratified into three groups, those with no, mild, or moderate renal impairment. Each of these groups was studied in a randomized crossover design, allowing for a 1-week washout between doses. The first group (no renal impairment) was dosed sequentially followed by a parallel dosing plan for the renally compromised subjects.
Subjects were initially screened over a period of up to 28 days and then given a baseline assessment on day 1 when they entered the study. There were four treatment periods per subject and each treatment lasted 24 h. Blood sampling was done during the dosing and continued for 96 h after dosing. Between the four treatments, subjects had a washout period of at least 7 days.
Subjects were randomized to receive a half-dose of NTM-001 (6.25 mg loading dose, followed at once by 1.75 mg/h over 24 h continuous infusion) or a ketorolac tromethamine IV bolus (KETO-BOLUS) regimen of 15 mg delivered every 6 h over 24 h. The crossover design meant that subjects joined the opposite group after the initial dosing to act as their own controls.
The observed ketorolac concentration–time profiles were plotted on the model-predicted ketorolac target profile according to the PK base model. Concentration–time data from both NTM-001 and the KETO-BOLUS treatments were fitted with the base model using a nonlinear mixed-effects (NLME) model and Monolix 3.2 software (Lixoft, Atony, France). The median ± 95% population-predicted confidence intervals versus time were plotted over the corresponding target median and prediction intervals as set forth by the base model. The PK parameters were calculated from plasma concentration–time data using the noncompartmental methods with Phoenix® WinNonlin® version 8.1 software (Certara Company, Princeton, New Jersey, USA).
Adverse events were monitored and assessed for severity by the principal investigator. Predefined adverse events of special interest (AESIs) and stopping criteria were predefined. An independent data safety and monitoring board (DSMB) reviewed safety and exposure data on a continuous basis over the course of the study.
Protocols were approved by the IntegReview institutional review board in Austin, Texas. The study protocol is NTM-001-HP001. All patients signed informed consent before entry into the study. The study complied with the Good Clinical Practice requirements described in the current International Council for Harmonization (ICH) guidelines and current federal regulations. This study was not registered with ClinicalTrials.gov.
This study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments.
Results
Thirty-nine subjects enrolled in the study, see Table 1 for demographic data. The study enrolled 51% women and 85% of participants were white.
Two subjects discontinued the study early by withdrawing consent; they were both in the group with no renal impairment. One other participant with no renal impairment dropped out of the study because of an adverse event (cellulitis), but the adverse events was deemed to be not related to the study treatment. All other subjects, except the aforementioned three, completed the study.
There was low intersubject variability for the individual subject ketorolac concentration–time profiles. Median concentrations following administration of the reduced-dose regimens (50% dose reduction) for both NTM-001 and the KETO-BOLUS groups were approximately 50% in the group with no renal impairment, 60% in the group with mild renal impairment, and 75% in the group with moderate renal impairment compared to the predicted concentration targets that would be obtained with the full-dose regimens.
Plots of observed versus predicted data were distributed symmetrically around the line of identity and there was no systematic departure from that line. This suggests that the equations and error models used to fit the data were appropriate for the older subjects and for subjects with mild and moderate renal impairment. Additional modeling of the output for both treatments was assessed and supported this finding. There was no need to update the model for better fit.
Based on the target curves for a full dose from an earlier study by the same investigators [7], the model-predicted concentration curves were approximately 50% lower for the healthy subjects, 40% lower for those with mild renal impairment, and 25% lower for those with moderate impairment. This shows that the target curves reduce as the degree of renal impairment increases. A comparison among the groups appears in Table 2.
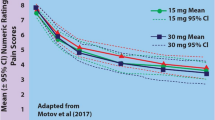
An overlay of NLME-predicted median plasma ketorolac concentrations versus time curves for the three groups (no renal impairment, mild renal impairment, moderate renal impairment) shows close similarities. The NTM-001 continuous infusion protocol was expected to have rapid onset of action due to the loading dose. See Fig. 1.
Based on NLME models, the median plasma ketorolac concentrations are illustrated for the KETO-BOLUS group (left) and the NTM-001 continuous IV infusion group (right). The three groups (healthy elderly, vs. mild or moderate renal impairment) exhibit similar concentration curves to the NTM-001 regimen exhibiting no peaks and troughs
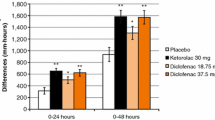
Ketorolac exposure in both the NTM-001 and KETO-BOLUS groups was similar, but values were highest in those subjects with moderate renal impairment and lowest in the group with no renal impairment. Compared to healthy subjects with no renal impairment, clearance values were approximately 80% or 60% in those with mild or moderate renal impairment, respectively. The ratio of NTM-001 to KETO-BOLUS clearance was essentially 1.0 within each renal function category, indicating that the administration of NTM-001 as a continuous infusion had no effect on clearance rates. This was expected. Treatment with NTM-001 continuous infusion maintains minimum concentrations (Cmin) higher than the trough values for the KETO-BOLUS regimen, independent of dose level and the subjects’ degree of renal impairment. These NTM-001 concentrations are always greater than the target 50% effective concentration (EC50) values for pain control. See Fig. 2.
Plasma ketorolac concentrations for both treatment regimens (NTM-001 and KETO-BOLUS) at the times of each KETO-BOLUS predose trough, depicted by group, and the relationship of those trough values to the effective concentration EC50 value for pain control (0.37 mg/L) determined by the PK/PD model. Comparative values from younger healthy subjects with no renal impairment are derived from an earlier study by these same investigators and are shown for comparison purposes [7]
The ratio of the respective Cmax values for the NTM-001 and KETO-BOLUS groups fell in the range of 26–34%. This suggests that NTM-001 continuous infusion will provide more continuous exposure above the EC50 target without causing undesirably high Cmax levels.
No unexpected or serious adverse events or deaths occurred. NTM-001 was well tolerated and safe in this vulnerable population. Adverse events are summarized in Table 3.
No signs of acute renal injury were observed in older subjects with renal impairment. Creatinine clearance rates during the study did not drop by 30% or more or change by 0.3–0.5 mg/dL, respectively. Hypertension, listed on the labeling of ketorolac tromethamine as a potential adverse effect, did not occur in this study nor did these regimens worsen pre-existing hypertension [3]. Infusion site reactions are of concern with any IV regimen, but no such reactions occurred with the NTM-001 continuous IV infusion. See Table 4.
Discussion
The aging populations of developed nations are both the fastest-growing segment of society and the population most likely to undergo surgery. The most rapidly expanding age group in the world are people over age 80, sometimes called the “oldest old” [8]. Postoperative analgesia can be challenging to manage in older patients because of the physiologic changes in metabolism associated with aging, particularly those involving renal and cardiovascular systems [6]. While aging is universally progressive, its physiologic and medical consequences can be highly individualized. Physicians are often advised to consider both chronological as well as biologic age, although there is no clear guidance as to how to do this [9, 10].
Opioids are not contraindicated in patients over the age of 65 years [11], but their use is increasingly coming under scrutiny for all patients. Patients with renal impairment may not be able to properly metabolize opioids, adversely affecting safety by allowing opioids to build up in the system and increase the risk for respiratory depression. In older patients on polypharmacy, opioids may lead to potentially dangerous drug–drug interactions [12, 13]. The use of a postoperative nonopioid product offers many potential and theoretical advantages, but in an older population, renal dysfunction, slowed metabolism, and other age-related physiologic changes can limit their use.
This pharmacologic study of NTM-001 in an older population demonstrated that NTM-001 had predictable pharmacologic properties and could be safely used in humans. Dosing was reduced by half for these subjects, because they were all older individuals; in all of these older subjects, including in those with mild to moderate renal impairment, the dose concentrations performed predictably over time. The loading dose followed immediately by continuous IV infusion of NTM-001 over 24 h resulted in fewer peaks and troughs and was well tolerated by subjects; the median EC50 values over the 0–24 h infusion period suggests it will be an effective pain reliever at the reduced concentrations chosen for age and degree of renal impairment. Clearance values were good.
Ketorolac tromethamine in IV administration has previously been shown to be an effective pain reliever [14,15,16]. IV and intramuscular administration of ketorolac have been compared favorably to parenteral administration of morphine for postoperative pain control [17,18,19,20]. In a study of postoperative pain control following maxillofacial surgery, intravenously administered ketorolac was as effective as tramadol with a lower incidence of vomiting (11.2% vs. 41.2%) [21]. Safety issues have raised concerns about ketorolac use, as it has been associated with several side effects, including gastrointestinal (GI) bleeding, GI perforation, platelet inhibition, and renal adverse effects. However, the risk of side effects is associated with higher doses of ketorolac, extended therapy (> 5 days), and vulnerable populations [22]. Ketorolac has been studied as an inpatient analgesic [23]. Another study involved 111 donor nephrectomy patients who were intravenously administered ketorolac or placebo for 24 h after their procedure. In a secondary analysis of these data, no significant differences in glomerular filtration rates were found between the ketorolac and placebo (saline) patients at 1 year. That study concluded that ketorolac could be safely administered intravenously for postoperative analgesia following nephrectomy [24]. A study of perioperative ketorolac administration in cholecystectomy followed by continuous infusion after surgery (n = 95) reported that ketorolac was a safe and effective pain reliever that had no negative effect on renal function [25]. A randomized multicenter trial (n = 11,245) with mixed parenteral and oral dosing for each drug found that ketorolac was as safe for relief of pain following major surgery as ketoprofen and diclofenac, but that overall risks for adverse events increased with advancing age [26].
This study has certain limitations. It is a pharmacologic study in volunteer subjects and evaluated serum drug concentrations and other pharmacologic properties rather than clinical effects. The parameters we used to define renal compromise were objective but may not capture the full spectrum of kidney disease and dysfunction. Finally, this study was small with 39 subjects. The racial balance of this study was primarily white (85%) with 13% Blacks and no Hispanics.
Conclusions
The urgent unmet medical need for safe, effective nonopioid analgesics for postoperative pain control has resulted in new studies of old agents such as ketorolac tromethamine as well as novel formulations of this same drug, NTM-001. Continuous infusion of NTM-001 has been compared to bolus IV injections every 6 h of ketorolac tromethamine in healthy adult subjects with good pharmacologic results. However, in real-world clinical practice such an analgesic option must be suitable also for all appropriate patients, including older patients with compromised renal function. This study demonstrated that NTM-001 as a continuous IV infusion was safe in older adults ≥ 65 years, including in those with mild or moderate renal impairment. Both NTM-001 and ketorolac exhibited reliable and predictable pharmacological values. There were no side effects over a 24-h course of continuous infusion in the NTM-001 group and no serious adverse events in the bolus injection group who received ketorolac tromethamine.
Data Availability
The availability of the dataset is crucial to serious research interests. The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Volkow ND, Blanco C. The changing opioid crisis: development, challenges and opportunities. Mol Psychiatry. 2021;26(1):218–33.
Mir HR, Miller AN, Obremskey WT, Jahangir AA, Hsu JR. Confronting the opioid crisis: practical pain management and strategies: AOA 2018 Critical Issues Symposium. J Bone Joint Surg Am. 2019;101(23):e126.
Toradol (ketorolac tromethamine tablets) Nutley, New Jersey: Roche Pharmaceuticals, 1997. https://www.accessdata.fda.gov/drugsatfda_docs/label/2013/019645s019lbl.pdf.
Pearce L, Bunni J, McCarthy K, Hewitt J. Surgery in the older person: training needs for the provision of multidisciplinary care. Ann R Coll Surg Engl. 2016;98(6):367–70.
Bouarich H, Chávez Guillén A, Rodríguez PD. Kidney and hypertension in older adults. Med Clin (Barc). 2021;157(4):178–84.
Coresh J, Selvin E, Stevens LA, et al. Prevalence of chronic kidney disease in the United States. JAMA. 2007;298(17):2038–47.
Pergolizzi JV Jr, Batra A, Schmidt WK. A randomized controlled trial of a novel formulation of ketorolac tromethamine for continuous infusion (NTM-001) in healthy volunteers. Adv Ther. 2024;41(2):659–671.
Coldrey JC, Upton RN, Macintyre PE. Advances in analgesia in the older patient. Best Pract Res Clin Anaesthesiol. 2011;25(3):367–78.
Falzone E, Hoffmann C, Keita H. Postoperative analgesia in elderly patients. Drugs Aging. 2013;30(2):81–90.
Hamczyk MR, Nevado RM, Barettino A, Fuster V, Andrés V. Biological versus chronological aging: JACC focus seminar. J Am Coll Cardiol. 2020;75(8):919–30.
Pergolizzi J, Boger RH, Budd K, et al. Opioids and the management of chronic severe pain in the elderly: consensus statement of an international expert panel with focus on the six clinically most often used World Health Organization Step III opioids (buprenorphine, fentanyl, hydromorphone, methadone, morphine, oxycodone). Pain Pract. 2008;8(4):287–313.
Pergolizzi JV. Quantifying the impact of drug-drug interactions associated with opioids. Am J Manag Care. 2011;17(Suppl 11):S288–92.
Pergolizzi JV Jr, Ma L, Foster DR, et al. The prevalence of opioid-related major potential drug-drug interactions and their impact on health care costs in chronic pain patients. J Manag Care Spec Pharm. 2014;20(5):467–76.
Motov S, Yasavolian M, Likourezos A, et al. Comparison of intravenous ketorolac at three single-dose regimens for treating acute pain in the emergency department: a randomized controlled trial. Ann Emerg Med. 2017;70(2):177–84.
Varrassi G, Marinangeli F, Agro F, et al. A double-blinded evaluation of propacetamol versus ketorolac in combination with patient-controlled analgesia morphine: analgesic efficacy and tolerability after gynecologic surgery. Anesth Analg. 1999;88(3):611–6.
Dwarica DS, Pickett SD, Zhao YD, Nihira MA, Quiroz LH. Comparing ketorolac with ibuprofen for postoperative pain: a randomized clinical trial. Female Pelvic Med Reconstr Surg. 2020;26(4):233–8.
Brown CR, Moodie JE, Wild VM, Bynum LJ. Comparison of intravenous ketorolac tromethamine and morphine sulfate in the treatment of postoperative pain. Pharmacotherapy. 1990;10(6 (Pt 2)):116S–121S.
Peirce RJ, Fragen RJ, Pemberton DM. Intravenous ketorolac tromethamine versus morphine sulfate in the treatment of immediate postoperative pain. Pharmacotherapy. 1990;10(6 (Pt 2)):111S–115S.
O’Hara DA, Fragen RJ, Kinzer M, Pemberton D. Ketorolac tromethamine as compared with morphine sulfate for treatment of postoperative pain. Clin Pharmacol Ther. 1987;41(5):556–61.
Yee JP, Koshiver JE, Allbon C, Brown CR. Comparison of intramuscular ketorolac tromethamine and morphine sulfate for analgesia of pain after major surgery. Pharmacotherapy. 1986;6(5):253–61.
Zackova M, Taddei S, Calò P, Bellocchio A, Zanello M. Ketorolac vs tramadol in the treatment of postoperative pain during maxillofacial surgery. Minerva Anestesiol. 2001;67(9):641–6.
Reinhart DI. Minimising the adverse effects of ketorolac. Drug Saf. 2000;22(6):487–97.
Vadivelu N, Gowda AM, Urman RD, et al. Ketorolac tromethamine - routes and clinical implications. Pain Pract. 2015;15(2):175–93.
Grimsby GM, Andrews PE, Castle EP, et al. Long-term renal function after donor nephrectomy: secondary follow-up analysis of the randomized trial of ketorolac vs placebo. Urology. 2014;84(1):78–81.
Varrassi G, Panella I, Piroli A, et al. The effects of perioperative ketorolac infusion on postoperative pain and endocrine-metabolic response. Anesth Analg. 1994;78(3):514–9.
Forrest JB, Camu F, Greer IA, et al. Ketorolac, diclofenac, and ketoprofen are equally safe for pain relief after major surgery. Br J Anaesth. 2002;88(2):227–33.
Acknowledgements
The authors would first like to express their gratitude to the participants in this study and to the investigators and their clinical teams whose work made this study possible.
Medical Writing/Editorial Assistance/Other
The authors wish to thank the medical writer who assisted in the preparation of this manuscript. Jo Ann LeQuang of Angleton, Texas, was the medical writer who drafted the manuscript, participated in the literature search, made and tracked author revisions, and formatted the paper for final submission. The costs for her services were covered by Neumentum. The authors gratefully acknowledge the work of Dr. Carl Peck and his team for their work that aided in the design of the initial study protocol. The authors also thank Todd Cooper of Coyote Studios of Green Valley, California, who helped take the figures from the clinical study and make them suitable for print. The authors would also like to thank Dr. Robert Colucci of NEMA Research who reviewed the manuscript and made important contributions to the section of study methodology.
Funding
The authors gratefully acknowledge the funding that made this study possible. The study was funded by Neumentum, Inc, including the Rapid Service Fee.
Author information
Authors and Affiliations
Contributions
The contributions of the authors are described here. Joseph V. Pergolizzi, Jr. was involved in the concept of the study, the organization of the paper, data analysis and interpretation, and he critically reviewed the manuscript at all stages and reviewed the final manuscript for publication. Amanjot Batra contributed to data interpretation, literature search, and reviewed the final manuscript. William K. Schmidt contributed to the data interpretation, reviewed the manuscript critically and wrote some portions, reviewed the bibliography for completeness, and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of Interest
Joseph V. Pergolizzi discloses the following relationships: He serves as consultant, speaker, owner, and/or researcher for the following companies: Neumentum, Spirify Pharma, Salix, Enalare Therapeutics, Advantx Pharmaceuticals, NEMA Research (he is chief operating officer), Innocan Pharmaceuticals, RTU Pharmaceuticals (he is director), and Bridge Therapeutics. He is Chief Executive Officer, Head of Research and Development, and Chairman of the Board for Neumentum. Amanjot Battra discloses that she is an employee of Neumentum. William K. Schmidt is associated with NorthStar Consulting and is a consultant for Neumentum.
Ethical Approval
Protocols were approved by the IntegReview institutional review board in Austin, Texas. The study protocol is NTM-001-HP001. All patients signed informed consent before entry into the study. The study complied with the Good Clinical Practice requirements described in the current International Council for Harmonization (ICH) guidelines and current federal regulations. This study was not registered with ClinicalTrials.gov. This study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Pergolizzi, J.V., Batra, A. & Schmidt, W.K. A Novel Formulation of Ketorolac Tromethamine (NTM-001) in Continuous Infusion in Adults with and without Renal Impairment: A Randomized Controlled Pharmacologic Study. Adv Ther 41, 3633–3644 (2024). https://doi.org/10.1007/s12325-024-02933-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-024-02933-7