Abstract
Introduction
Empagliflozin is a sodium-glucose co-transporter-2 inhibitor used to treat type 2 diabetes (T2D) to improve glycemic control, reduce risk of cardiovascular death in patients with T2D, and treat patients with symptomatic chronic heart failure (HF) and chronic kidney disease (CKD). The safety profile of empagliflozin is well documented, although adverse events (AEs) remain of interest to clinicians. This study provides an up-to-date safety evaluation of empagliflozin.
Methods
Data were pooled from four long-term trials which included: patients with T2D and established cardiovascular disease (EMPA-REG OUTCOME), patients with HF, with/without diabetes (EMPEROR-Reduced and EMPEROR-Preserved), and patients with CKD, with/without diabetes (EMPA-KIDNEY). Since three of the four trials evaluated empagliflozin 10 mg, the meta-analysis was restricted to this dose.
Results
Total trial medication exposure was 19,727 patient-years for patients who received empagliflozin (n = 10,472) and 19,447 patient-years for placebo (n = 10,461). The percentages of patients with serious AEs, fatal AEs, and AEs leading to discontinuation were similar for both groups. The incidences of serious urinary tract infection and serious pyelonephritis or urosepsis were similar for both groups but higher for women taking empagliflozin versus placebo. Serious genital infections were not increased with empagliflozin versus placebo. There was a slight increase in ketoacidosis and serious volume depletion in patients who received empagliflozin versus placebo. The occurrence of serious acute kidney injury was lower with empagliflozin versus placebo. Empagliflozin was not associated with an increased incidence of severe hypoglycemia, bone fractures, or lower limb amputations. Empagliflozin is therefore considered safe in people without diabetes, the elderly, patients with very low estimated glomerular filtration rate, low body mass index, and HF. Safety is unaltered by blood pressure, concomitant medication for hypertension, HF, and immunosuppression.
Conclusion
This meta-analysis of long-term safety data extends current knowledge and confirms the safety and tolerability of empagliflozin.
Plain Language Summary
Empagliflozin is used in adults with type 2 diabetes mellitus (T2D) to improve blood glucose control and in people with T2D and established cardiovascular disease to reduce the risk of death from cardiovascular disease. Also, it is used to treat people with chronic heart failure or chronic kidney disease. Although many clinical trials have shown the effectiveness and safety of empagliflozin, the evaluation of adverse events (AEs) remains of interest. This study further examined the safety of empagliflozin by analyzing four large, long-term clinical trials. These trials included over 20,900 patients with T2D and established cardiovascular disease, patients with heart failure, and patients with chronic kidney disease. Adverse events of interest were pooled and analyzed. Results show the risk of the investigated AEs was similar whether patients had received empagliflozin or placebo. The risk of urinary tract infections, including those that spread to the kidneys, was higher for women taking empagliflozin versus placebo. Ketoacidosis was rare but more frequent in patients taking empagliflozin. A reduction in blood volume was slightly more frequent in people taking empagliflozin versus placebo. The risk of kidney injury was reduced in patients taking empagliflozin versus placebo. The risk of genital infections, hypoglycemia, bone fractures, or lower limb amputations was not increased with empagliflozin. No new safety concerns were raised, including in people who were elderly, had kidney disease, low body weight, T2D, or heart failure. This analysis is consistent with current knowledge of empagliflozin safety in a broad range of patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Empagliflozin is a sodium-glucose co-transporter 2 (SGLT2) inhibitor, originally developed for the treatment of adults with insufficiently controlled type 2 diabetes (T2D) as an adjunct to diet and exercise. Its use has further broadened to include patients with T2D and established cardiovascular disease to reduce the risk of death from cardiovascular disease and the treatment of patients with symptomatic chronic heart failure and chronic kidney disease. |
While a large body of clinical trial data indicates that empagliflozin is well tolerated, several potential adverse events (AEs) remain of interest to clinicians. |
The current meta-analysis provides an up-to-date evaluation of the safety of empagliflozin in a broad range of patients based on four large placebo-controlled clinical outcome trials, EMPA-REG OUTCOME, EMPEROR-Reduced, EMPEROR-Preserved, and EMPA-KIDNEY. This is the first meta-analysis of empagliflozin to include trials of all conditions for which empagliflozin is indicated. |
This meta-analysis focused on patients receiving empagliflozin 10 mg and evaluated the occurrence of selected AEs in the overall population and in key subgroups of medical interest. |
What has been learned from this study? |
This analysis updates and extends the findings of previous pooled analyses and confirms current knowledge of the safety and tolerability of empagliflozin based on long-term data from 20,933 participants. |
These findings were consistent across a broad range of participants, including patients with and without T2D, patients with established cardiovascular disease, patients with heart failure, and a wide range of patients with chronic kidney disease. |
Introduction
Empagliflozin is a sodium-glucose co-transporter 2 (SGLT2) inhibitor that was initially developed for the improvement of glycemic control in patients with type 2 diabetes (T2D). Following further evaluation of empagliflozin in patients with T2D with established cardiovascular disease in the phase III cardiovascular outcome trial, EMPA-REG OUTCOME, a reduction in 3-point major adverse cardiovascular outcomes (3P-MACE) was demonstrated, primarily driven by a reduction in cardiovascular death [1]. More recently, three large clinical trials have demonstrated the benefits of empagliflozin in a broader patient population, irrespective of baseline cardiovascular risk or the presence of T2D [2,3,4]. These trials were completed across the spectrum of patients with heart failure (HF): Empagliflozin Outcome Trial in Patients with Chronic Heart Failure and a reduced ejection fraction (EMPEROR-Reduced) and a trial in patients with a preserved ejection fraction (EMPEROR-Preserved) [2, 4]. In addition, patients with chronic kidney disease (CKD) were specifically investigated (Study of Heart and Kidney Protection with Empagliflozin, EMPA-KIDNEY) [3]. In addition to using empagliflozin for adults with insufficiently controlled T2D, as an adjunct to diet and exercise, its use has further broadened to include the treatment of symptomatic chronic heart failure (HF) and CKD [5].
The safety profile of empagliflozin is well documented, based on the results of various phase I–III trials and the subsequent publication of several pooled analyses of these data [6,7,8,9,10]. The safety profile of a drug can be defined in terms of adverse reactions, which are undesired and harmful effects that result from the administration of the drug. Some of the commonly reported adverse reactions associated with SGLT2 inhibitors relate to their mode of action. Blockade of SGLT2 on the proximal tubules of the kidney induces the excretion of glucose and sodium in the urine, contributing to osmotic diuresis and a reduction in plasma volume [11]. These mechanisms may increase the likelihood of adverse reactions including genital mycotic infections, urinary tract infections (UTIs), and hypotension, although serious complications are infrequent [12]. Despite published safety data, several potential AEs remain of interest to clinicians [12, 13]. A comprehensive analysis of safety data for empagliflozin (10 mg or 25 mg once daily) in patients with T2D, published in 2020, showed that the risk of hypoglycemia was similar for empagliflozin and placebo, except when co-administered with insulin and/or a sulfonylurea [6]. Based on 16,480 patient-years of exposure to empagliflozin, the main adverse reactions included events consistent with genital infection for empagliflozin 10/25 mg versus placebo (3.54 vs. 0.95/100 patient-years, respectively). The incidence of events consistent with UTI was similar for the empagliflozin 10/25 mg and placebo groups (9.27 vs. 9.70/100 patient-years, respectively). The majority of events consistent with genital infection or UTI were non-serious, mild, or moderate in intensity and led to treatment discontinuation in < 1% of patients in the empagliflozin 10/25 mg and placebo groups. The frequency of events consistent with volume depletion was similar for empagliflozin 10/25 mg and placebo (3.1% vs. 3.0%, respectively); however, these events were slightly more frequent with empagliflozin 10/25 mg than placebo in older patients (aged 75 to < 85 years) (5.9% vs. 5.0%) and in patients receiving therapy with loop diuretics at baseline (9.8% vs. 7.4%). This analysis showed no increase in the incidences of safety topics of interest, including urinary tract carcinogenicity, renal impairment, Fournier’s gangrene, liver injury, pancreatitis, diabetic ketoacidosis, bone fractures, or lower limb amputation in the empagliflozin group versus placebo. A further meta-analysis evaluated the safety of empagliflozin in 15,081 patients with T2D and advanced CKD (defined as moderate to severe CKD [category G3–4]) [10]. No new safety concerns were identified in this high-risk population, and the overall rates of AEs were similar among patients who received empagliflozin and placebo, and across eGFR categories. In addition, rates of AEs of special interest were similar for patients who received empagliflozin versus placebo. An exception was the frequency of genital infections, which was higher in the empagliflozin 10/25 mg group compared with placebo (3.54 vs. 0.85/100 patient-years), with progressively lower incidence rates across CKD categories 3A (2.75/100 patient-years), 3B (1.78), and 4 (1.13), although the frequency of genital infections was greater for empagliflozin than placebo patients in all CKD categories.
The aim of the current meta-analysis was to provide an up-to-date evaluation of the safety of empagliflozin in a broad range of patients based on four large placebo-controlled clinical outcome trials, EMPA-REG OUTCOME, EMPEROR-Reduced, EMPEROR-Preserved, and EMPA-KIDNEY. Although the overall results and subgroup analyses have been published for each individual trial, each trial has limited power to quantify the effects of empagliflozin on safety outcomes. Therefore, this pooled analysis evaluated the effect of empagliflozin versus placebo on the occurrence of selected AEs in the overall population and in key subgroups of medical interest. The four included clinical trials studies encompass the group of patients with conditions for which empagliflozin is indicated. The long duration of empagliflozin exposure allows the assessment of events that occur with a low incidence. This analysis updates and extends the findings of previous pooled analyses of empagliflozin and is intentionally restricted to long-term outcome trials.
Methods
Participants
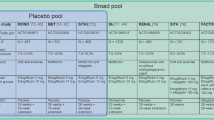
Data were pooled from four trials (Table 1) which included patients with T2D and high risk for cardiovascular events (EMPA-REG OUTCOME), patients with HF, with or without diabetes (EMPEROR-Reduced and EMPEROR-Preserved), and a broad population of patients with CKD, with or without diabetes (EMPA-KIDNEY). In EMPA-REG OUTCOME, patients were randomized to receive empagliflozin 10 mg or 25 mg or placebo in addition to standard of care. In the other three trials, only the 10 mg dose of empagliflozin was investigated. To avoid a potential indication-associated bias, this pooled analysis was restricted to empagliflozin 10 mg. Furthermore, since the safety profiles of empagliflozin 10 mg and 25 mg have already been shown to be similar in the EMPA-REG OUTCOME trial, as well as in the latest pooled safety analysis of empagliflozin [6, 14], inclusion of the 25 mg dose was not expected to add relevant further information to the analyses of the 10 mg dose. Therefore, only patients receiving empagliflozin 10 mg were included in the meta-analysis. In addition, patients with type 1 diabetes (10 patients from EMPEROR-Preserved and 68 patients from EMPA-KIDNEY) were excluded from the analyses to reflect the current indication.
The ethics committee at each center approved the trials, and all patients provided written informed consent. All original trials were performed in accordance with the Declaration of Helsinki.
Assessments and Data Analyses
Safety and tolerability were assessed based on AEs reported in each trial. Since the safety profile of empagliflozin has been comprehensively evaluated in previous trials, the collection of safety data was streamlined in EMPA-KIDNEY. Therefore, the pooled analysis of the four currently available outcome trials was restricted to the information on AEs systematically collected and documented in EMPA-KIDNEY. The selection of safety endpoints and subgroups was based on the known risks for empagliflozin or safety topics for which the medical community has expressed interest for the class of SGLT2 inhibitors. If safety endpoints were not analyzed for the EMPEROR and EMPA-REG OUTCOME trials, corresponding safety endpoints were newly derived from individual patient data in these studies. For the calculation of eGFR values, the CKD-EPI formula was applied to individual patient data from EMPA-REG Outcome to be consistent with the calculations used in the other three trials.
AEs were coded according to preferred terms in the Medical Dictionary for Regulatory Activities (MedDRA) version 23.1. AEs were identified based on investigator-reported AEs using standardized MedDRA or customized BI MedDRA queries. For EMPA-KIDNEY, adjudicated events were considered if available. AEs of interest included serious UTI, serious pyelonephritis or urosepsis, serious genital infections, and serious acute kidney injury, severe hypoglycemia, ketoacidosis, serious volume depletion, bone fracture, and lower limb amputation. Non-serious AEs were not generally reported in EMPA-KIDNEY; therefore, only serious AEs were included in this meta-analysis, with the following exceptions: bone fractures, events leading to lower limb amputation, and severe hypoglycemia (defined as investigator-reported severe hypoglycemia—i.e., requiring assistance). Since lower limb amputations were not systematically recorded in EMPA-REG OUTCOME, this was assessed on the basis of a previous medical review of the AEs, concomitant therapy, and AE narratives. All AEs were analyzed overall and by T2D status and based on subgroups relevant to the AE of interest: age, sex, eGFR, HF, baseline blood pressure, peripheral artery disease at baseline, immunosuppressive therapy, and treatment at baseline (renin-angiotensin system inhibitors, diuretics, and antihypertensives). Although harmonized endpoints and subgroups were derived, the final databases of the individual studies were not modified, for example by adding or excluding data or by applying different inclusion or exclusion criteria. In general, the analyses were based on subgroup categorizations derived for the individual trials and corresponding trial data.
Analyses of AEs were based on participants who were dispensed trial medication. Treatment was evaluated as randomized. The safety analyses were based on the number of patients with AEs rather than the number of AEs. The AE analyses included data from the date of randomization to trial completion (date of last follow-up for safety) (intention-to-treat approach). Incidence rates for AEs were calculated per 100 patient-years. The 95% confidence interval (CI) for the incidence rate was based on the exact (Clopper-Pearson) CIs. Time at risk was defined as (date of onset of AE − randomization date + 1) for patients with event. Patients without event were considered at risk until trial completion. Pooled risk ratio estimates were calculated from the Cochran-Mantel-Haenszel procedure stratified by trial. The pooled risk difference and its 95% CI were calculated by pooling the risk differences of each trial across the trials. Studies were weighted according to their size (total number of patients). For the analysis of AEs, interpretation was based not only on the statistical test (indicated by the 95% CI) but also on overall knowledge of AEs commonly associated with empagliflozin. Formal statistical tests were not performed as the study was not powered to assess differences in safety findings or adjusted for multiple comparisons. A supplemental analysis was performed for patients who initiated chronic dialysis and continued trial medication while on dialysis. The occurrence of AEs, serious AEs, and AEs leading to treatment discontinuation was assessed from start of dialysis to trial completion.
Results
Patient Disposition, Exposure, and Baseline Characteristics
The analysis set included 20,933 patients, of whom 10,472 received empagliflozin 10 mg and 10,461 placebo. The median duration of follow-up was 2.1 years. The median exposure to the trial medication was 1.8 years. The total trial medication exposure was 19,727 patient-years in the empagliflozin group and 19,447 patient-years for placebo. Patient demographics and baseline characteristics were well matched between the empagliflozin and placebo groups (Table 2). In total, 61% of patients were aged > 65 years, 3.0% were aged ≥ 85 years, and 74% had renal disease at baseline.
Overall Safety and Safety Topics of Interest
The percentages of patients with serious AEs, fatal AEs, and AEs leading to discontinuation were also similar for both groups (Table 3).
Serious UTI
The incidence of serious UTI was comparable between empagliflozin and placebo groups (0.78 vs. 0.76 events/100 patient-years, respectively; rate ratio, 1.03 [0.83, 1.27]) (Table 4). Female patients experienced a higher incidence of serious UTIs than male patients (Table 5). The event rates for serious UTIs were higher in female patients in the empagliflozin group versus placebo (rate ratio 1.33 [0.97, 1.82]) but not in male patients (rate ratio 0.81 [0.61, 1.09]). In the placebo group, patients with a history of HF also showed an increased incidence of serious UTI compared with individuals without HF (0.89 vs. 0.64 events/100 patient-years). A numerical increase was seen in the empagliflozin group versus placebo, with rate ratio of 1.18 (0.89, 1.56). In patients without a history of HF, the incidence of serious UTI was lower in those who received empagliflozin versus placebo (rate ratio 0.83 [0.60; 1.16]). There was no increased risk between empagliflozin and placebo for patients with T2D compared with patients without diabetes. The rates of serious UTI increased in the placebo group with decreasing eGFR; however, a similar pattern was not seen in the empagliflozin group. The event rates were comparable between empagliflozin and placebo groups across all eGFR categories in general.
Serious Pyelonephritis or Urosepsis
Similar rates of serious pyelonephritis or urosepsis were shown for empagliflozin versus placebo (0.28 vs. 0.25/100 patient-years, respectively; rate ratio, 1.09 [0.76, 1.56]) (Supplementary Material, Table S1). Subgroup analysis indicated an increased incidence with empagliflozin in women but not in men (rate ratios, 1.87 vs. 0.64 respectively). The risk of serious pyelonephritis or urosepsis was not consistently affected by empagliflozin; it was increased in the 75 to < 85 years age group for empagliflozin versus placebo (rate ratio 1.75 [0.93, 3.31]) but not in patients aged ≥ 85 years (rate ratio 0.90 [0.24, 3.36]).
Serious Genital Infection
The incidence of serious genital infection was not increased for patients who received empagliflozin versus placebo (rate ratio 0.62 [0.28, 1.37]) (Table 4). No risk increase for empagliflozin was indicated in any subgroup category (Supplementary Material, Table S1).
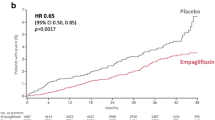
Serious Acute Kidney Injury
The risk of serious acute kidney injury was lower in the empagliflozin group versus placebo (0.73 [0.64, 0.83]) (Table 4). Although higher event rates were seen in patients with T2D, HF, worsening eGFR, and increasing age in both the empagliflozin and placebo groups, rates of serious acute kidney injury were consistently lower in the empagliflozin group versus placebo across all subgroups (Supplementary Material, Table S1).
Severe Hypoglycemia
The incidence of severe hypoglycemia was similar for patients in the empagliflozin and placebo groups (0.97 [0.78, 1.22]) (Table 4). No risk increase for empagliflozin was indicated in any subgroup category (Supplementary Material, Table S1).
Ketoacidosis
Ketoacidosis was reported in a small number of patients in the empagliflozin and placebo groups (15 vs. 7 patients; 0.07 events vs. 0.03 events/100 patient-years, respectively; rate ratio, 2.13 [0.87, 5.24]) (Table 6). Ketoacidosis occurred in only one patient without T2D in the empagliflozin group.
Serious Volume Depletion
Serious volume depletion was slightly more common in patients who received empagliflozin versus placebo (0.94 vs. 0.88 events/100 patient-years, respectively; rate ratio, 1.08 [0.88, 1.31]) (Table 4). The incidence of serious volume depletion increased with age. The highest incidence of volume depletion for empagliflozin versus placebo was among patients aged ≥ 85 years (15 vs. 6 patients; 2.56 vs. 1.00/100 patient-years; rate ratio, 2.39 [0.92, 6.21]) (Supplementary Material, Table S1).
Bone Fractures
The incidence of bone fracture was similar in the empagliflozin group versus placebo (2.03 vs. 1.93/100 patient-years; rate ratio, 1.05 [0.92, 1.20]) (Table 4). The subgroup analyses did not indicate an increased risk of bone fractures with empagliflozin (Supplementary Material, Table S1).
Lower Limb Amputation
The occurrence of lower limb amputation was similar among patients who received empagliflozin versus placebo (0.43 vs. 0.42 events/100 patient-years; rate ratio, 1.01 [0.76, 1.35]) (Table 4). For the subgroup of patients with body mass index (BMI) < 25 kg/m2, there was a numerical increase in the rate of lower limb amputations (rate ratio 2.12 [0.92, 4.89]) (Table 6). This finding is based on a relatively small number of patients with events (8 vs. 18 for placebo and empagliflozin, respectively) with consequently broad confidence intervals. This finding is likely related to the unusually high frequency of lower limb amputation in the empagliflozin 10 mg group with BMI < 25 kg/m2 of the EMPA-REG OUTCOME trial and is considered to be a chance finding. The analyses did not show a consistent trend across the four BMI categories evaluated (Table 6).
The remaining subgroup analyses do not indicate inconsistent findings among the individual subgroups.
Patients Who Initiated Chronic Dialysis
A total of 54 patients in the empagliflozin group and 83 who received placebo initiated chronic dialysis and continued with study treatment while on dialysis. Although this is not a randomized comparison, the results do not indicate an increase in AEs with empagliflozin regarding the frequency of investigator-defined drug-related AEs, AEs leading to treatment discontinuation, serious AEs, or fatal AEs in patients on dialysis (Table 7).
Discussion
This meta-analysis of pooled safety, based on more than 19,727 patient-years of exposure to empagliflozin, indicates no safety concerns with empagliflozin. This is the first meta-analysis of empagliflozin to include trials of all conditions for which empagliflozin is indicated and extends the findings of previous pooled analyses [6,7,8] by inclusion of a broad range of participants including patients with T2D and established cardiovascular disease, patients with HF, with or without diabetes, and a wide range of patients with CKD, with or without diabetes, enabling analyses in a range of subgroups. Since the assessment of non-serious (or not leading to treatment discontinuation) UTI and genital infections, acute kidney injury, and volume depletion was not included in the EMPA-KIDNEY trial, the present meta-analysis focused on serious AEs in these categories. However, data for non-serious AEs have already been published in patients with T2D [6] and HF [2, 4] and are in line with the results of the present analysis.
Consistent with previous experience [6,7,8], rates of serious UTI were higher in female patients compared with male patients, in both the placebo and empagliflozin groups. In addition, the rate of serious UTI was higher among women who received empagliflozin versus placebo. The incidence of serious pyelonephritis or urosepsis was not increased among male patients but there was a small increase for women who received empagliflozin versus placebo. With a low number of events overall, serious genital infections were not increased for empagliflozin versus placebo in any subgroup including sex.
The present meta-analysis showed that the occurrence of serious acute kidney injury was lower with empagliflozin therapy compared with placebo. This finding is consistent with the finding of a meta-analysis of SGLT2 inhibitors, which showed a 30% reduction in acute kidney injury among patients who received SGLT2 inhibitors [12]. A recent meta-analysis and systematic review of the effects of SGLT2 inhibition on kidney outcomes evaluated acute kidney injury as an efficacy outcome in terms of reduction in the number of patients with progression of kidney disease [9]. The meta-analysis showed a 23% reduction in acute kidney injury associated with SGLT2 inhibition, with similar reductions in patients with and without T2D. This outcome is considered to reflect the kidney-protective effects of empagliflozin [9].
Severe hypoglycemia (i.e., requiring assistance) is a concern for patients with T2D. The findings of the present meta-analysis indicate that this risk is not increased with empagliflozin. This finding is consistent with the results of previous pooled analyses of empagliflozin [6,7,8]. Since SGLT2 inhibitors reduce plasma glucose by increasing glucose excretion by the kidneys, an effect that is independent of insulin [15], the overall risk of hypoglycemia is low when these agents are used as monotherapy [16]. Diabetic ketoacidosis is a rare AE associated with SGLT2 inhibitor therapy that may occur with minimal increases in blood glucose [17]. The likelihood of ketoacidosis is increased among patients with established T2D who are being treated with insulin and can be potentiated by fasting, intercurrent illness, or surgical intervention. A large collaborative meta-analysis of available evidence from large SGLT2 inhibitor trials showed that patients without T2D are at especially low risk of ketoacidosis associated with SGLT2 inhibitor therapy [9]. This present meta-analysis showed a small absolute increase in the incidence of ketoacidosis among patients receiving empagliflozin versus placebo. Most of these events occurred in patients with T2D, with just one event in a patient without T2D who received empagliflozin.
Empagliflozin produces transient natriuresis and increases in urine volume [18], resulting in the potential for hypotension and volume depletion, particularly among elderly individuals [5]. The findings of this meta-analysis indicate that serious volume depletion was more frequent in the empagliflozin group compared with placebo, with an increased incidence with older age in the empagliflozin group (being greatest in patients aged ≥ 85 years).
Bone fracture has been an AE of interest following The Canagliflozin Cardiovascular Assessment Study (CANVAS), which reported an increase in bone fractures among patients who received canagliflozin versus placebo (15.4 vs. 11.9 participants with fracture/1000 patient-years; HR 1.26; 95% CI 1.04, 1.52) [19]. However, an increased risk of fractures was not observed in a subsequent trial of canagliflozin [20] and has not been observed with other SGLT2 inhibitors [12, 13]. Similarly, previous pooled analyses for empagliflozin have shown no association with treatment and an increased occurrence of bone fractures [6,7,8]. The present meta-analysis provides further support for these findings based on a median 2.1-year (110 week) follow-up period.
The CANVAS study also indicated a two-fold increase in risk of lower limb amputation (primarily of the metatarsal) among patients who received canagliflozin versus placebo [19]. As a result, the occurrence of amputations has specifically been evaluated in subsequent clinical trials of SGLT2 inhibitors. As with bone fractures, no increased risk of lower limb amputation was indicated in a subsequent trial of canagliflozin [20], with other SGLT2 inhibitors [12, 13], or in previous pooled analyses for empagliflozin [6,7,8]. These findings are further supported by the present meta-analysis.
Until recently, patients with CKD and eGFR < 30 ml/min/1.73 m2 and patients on dialysis have been underrepresented in trials of SGLT2 inhibitors. However, the EMPA-KIDNEY trial showed that empagliflozin was associated with preservation of kidney function across a wide range of eGFR levels, including levels as low as 20 ml/kg/1.73 m2, with no evidence of safety concerns. The present meta-analysis does not indicate that patients on dialysis are at increased risk of AEs if treated with empagliflozin. No new safety concerns were raised in the analyses of AEs by other subgroups, including age, BMI, presence of T2D, or concurrent HF. Thus, this meta-analysis does not indicate that empagliflozin is associated with an increased risk of AEs in subpopulations of interest, including patients with low eGFR, low BMI, elderly patients, and patients with or without comorbidities such as T2D and HF.
The strengths of this meta-analysis include the large number of participants and the long total exposure to treatment and follow-up period. Restricting the analyses to empagliflozin enabled an individual patient data approach and subgroup analysis to ensure the generation of high-quality data. This would not have been possible if a summary-based approach (aggregated data) had been used, as this would have required the availability of subgroup results across the trials. As with all meta-analyses, an important limitation of the present analysis is the inclusion of trials of different durations and methodologies. In addition, the analysis of lower limb amputations in the EMPA-REG OUTCOME study should be interpreted with caution in view of the manual retrieval and validation of these cases. Another limitation of the present meta-analysis is that only the AEs of interest included in EMPA-KIDNEY were analyzed. However, other AEs have been extensively analyzed in previous pooled analyses for empagliflozin [6,7,8]. Low patient numbers in some of the subgroups, including the group who started dialysis during the study, mean that the data collected were insufficient for generating conclusions and should, therefore, be interpreted with caution.
Conclusion
This meta-analysis of 20,933 participants of four large, randomized, placebo-controlled clinical trials of empagliflozin extends previous pooled safety analyses and confirms previous knowledge of the safety and tolerability of empagliflozin. These findings were consistent across a broad range of participants, including patients with and without T2D, patients with HF, and a wide range of patients with CKD, and various subgroups of specific interest. Furthermore, there was no evidence to indicate that patients on dialysis are at increased risk of AEs when treated with empagliflozin.
Data Availability
To ensure independent interpretation of clinical study results and enable authors to fulfill their role and obligations under the ICMJE criteria, Boehringer Ingelheim grants all external authors access to relevant clinical study data. In adherence with the Boehringer Ingelheim Policy on Transparency and Publication of Clinical Study Data, scientific and medical researchers can request access to clinical study data, typically, 1 year after the approval has been granted by major Regulatory Authorities or after termination of the development program. Researchers should use the https://vivli.org/ link to request access to study data and visit https://www.mystudywindow.com/msw/datasharing for further information.
References
Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373:2117–28.
Anker SD, Butler J, Filippatos G, et al. Empagliflozin in heart failure with a preserved ejection fraction. N Engl J Med. 2021;385:1451–61.
Herrington WG, Staplin N, Wanner C, et al. Empagliflozin in patients with chronic kidney disease. N Engl J Med. 2023;388:117–27.
Packer M, Anker SD, Butler J, et al. Cardiovascular and renal outcomes with empagliflozin in heart failure. N Engl J Med. 2020;383:1413–24.
Boehringer Ingelheim Limited. Jardiance 10 mg film-coated tablets. Summary of Product Characteristics, Updated 14 Sep 2023. https://www.medicines.org.uk/emc/product/5441/smpc#about-medicine. Accessed 8 Feb 2024.
Kinduryte Schorling O, Clark D, Zwiener I, Kaspers S, Lee J, Iliev H. Pooled safety and tolerability analysis of empagliflozin in patients with type 2 diabetes mellitus. Adv Ther. 2020;37:3463–84.
Kohler S, Salsali A, Hantel S, et al. Safety and tolerability of empagliflozin in patients with type 2 diabetes. Clin Ther. 2016;38:1299–313.
Kohler S, Zeller C, Iliev H, Kaspers S. Safety and tolerability of empagliflozin in patients with type 2 diabetes: pooled analysis of phase I–III clinical trials. Adv Ther. 2017;34:1707–26.
Nuffield Department of Population Health Renal Studies G, Consortium SiM-AC-RT. Impact of diabetes on the effects of sodium glucose co-transporter-2 inhibitors on kidney outcomes: collaborative meta-analysis of large placebo-controlled trials. Lancet. 2022; 400:1788–801.
Tuttle KR, Levin A, Nangaku M, et al. Safety of empagliflozin in patients with type 2 diabetes and chronic kidney disease: pooled analysis of placebo-controlled clinical trials. Diabetes Care. 2022;45:1445–52.
Abdul-Ghani MA, DeFronzo RA. Lowering plasma glucose concentration by inhibiting renal sodium-glucose cotransport. J Intern Med. 2014;276:352–63.
Staplin N, Roddick AJ, Emberson J, et al. Net effects of sodium-glucose co-transporter-2 inhibition in different patient groups: a meta-analysis of large placebo-controlled randomized trials. EClinicalMedicine. 2021;41: 101163.
Donnan JR, Grandy CA, Chibrikov E, et al. Comparative safety of the sodium glucose co-transporter 2 (SGLT2) inhibitors: a systematic review and meta-analysis. BMJ Open. 2019;9: e022577.
Inzucchi SE, Iliev H, Pfarr E, Zinman B. Empagliflozin and assessment of lower-limb amputations in the EMPA-REG OUTCOME trial. Diabetes Care. 2018;41:e4–5.
Abdul-Ghani MA, DeFronzo RA. Inhibition of renal glucose reabsorption: a novel strategy for achieving glucose control in type 2 diabetes mellitus. Endocr Pract. 2008;14:782–90.
Scheen AJ. Pharmacodynamics, efficacy and safety of sodium-glucose co-transporter type 2 (SGLT2) inhibitors for the treatment of type 2 diabetes mellitus. Drugs. 2015;75:33–59.
Palmer BF, Clegg DJ. Euglycemic ketoacidosis as a complication of SGLT2 inhibitor therapy. Clin J Am Soc Nephrol. 2021;16:1284–91.
Heise T, Jordan J, Wanner C, et al. Pharmacodynamic effects of single and multiple doses of empagliflozin in patients with type 2 diabetes. Clin Ther. 2016;38:2265–76.
Neal B, Perkovic V, Matthews DR. Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med. 2017;377:2099.
Perkovic V, Jardine MJ, Neal B, et al. Canagliflozin and renal outcomes in type 2 diabetes and nephropathy. N Engl J Med. 2019;380:2295–306.
Medical Writing/Editorial Assistance
Medical writing assistance was provided by Jennifer Garrett, MBBS, of Envision Pharma Group, which was contracted and funded by Boehringer Ingelheim (BI) & Eli Lilly and Company Diabetes Alliance. BI and Lilly were given the opportunity to review the manuscript for medical and scientific accuracy as well as intellectual property considerations.
Funding
The authors received no payment related to the development of the manuscript. The Rapid Service and Open Access fees were funded by Boehringer Ingelheim & Eli Lilly and Company Diabetes Alliance.
Author information
Authors and Affiliations
Contributions
The authors meet criteria for authorship as recommended by the International Committee of Medical Journal Editors (ICMJE). Christoph Wanner, Egon Pfarr, Hristo Iliev, and Elke Schueler were involved in conception/design of the study. Egon Pfarr, Hristo Iliev, and Elke Schueler were involved in acquisition of data/ data analysis. All authors were involved in interpretation of data and drafting the manuscript or revising it critically for important intellectual content.
Corresponding author
Ethics declarations
Conflict of Interest
Christoph Wanner has received personal fees from Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, CSL-Vifor, Eli Lilly and Company, GlaxoSmithKline, MSD, Novo Nordisk, Novartis, and Sanofi. Hristo Iliev is an employee of Boehringer Ingelheim. Vikram Thanam is an employee of Boehringer Ingelheim. Elke Schueler is employee of mainanalytics GmbH, working on behalf of Boehringer Ingelheim Pharma GmbH & Co. KG. Egon Pfarr is an employee of Boehringer Ingelheim. Ana Rita Soares is an employee of Eli Lilly and Company. Nathalia Duarte is an employee of Boehringer Ingelheim.
Ethical Approval
The ethics committee at each center approved the trials, and all patients provided written informed consent. All original trials were performed in accordance with the Declaration of Helsinki.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Wanner, C., Iliev, H., Duarte, N. et al. Safety of Empagliflozin: An Individual Participant-Level Data Meta-Analysis from Four Large Trials. Adv Ther 41, 2826–2844 (2024). https://doi.org/10.1007/s12325-024-02879-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-024-02879-w