Abstract
Introduction
Immune-mediated inflammatory diseases including rheumatoid arthritis (RA), psoriatic arthritis (PsA), ankylosing spondylitis (AS), non-radiographic axial spondylarthritis (nr-axSpA), atopic dermatitis (AD), ulcerative colitis (UC), and Crohn’s disease (CD) pose a substantial burden on patients and their quality of life. Upadacitinib is an orally administered, selective, and reversible Janus kinase inhibitor indicated for seven conditions, but data on its safety versus other active treatments are limited. A systematic literature review of indirect and direct treatment comparisons of randomized controlled trials (RCTs) was conducted to assess the safety profile of upadacitinib.
Methods
MEDLINE, Embase, and Cochrane Library databases were searched for indirect and direct treatment comparisons of RCTs that (1) included licensed upadacitinib dosages; (2) studied any of the seven conditions; (3) reported any adverse events (AEs), serious AEs (SAEs), AEs leading to discontinuation, major adverse cardiovascular event, venous thromboembolism, malignancies, infections or serious infections, and death; and (4) were published between January 2018 and August 2022.
Results
A total of 25 studies were eligible for inclusion. SAEs, AEs leading to discontinuation, and any AEs were commonly studied. RA was the most studied condition, followed by AD and UC. Most studies (16/25, 64%) reported no statistically significant difference in the studied safety outcomes between upadacitinib and other active treatments (e.g., tumor necrosis factor blockers, interleukin receptor antagonists, integrin receptor antagonists, T cell co-stimulation modulator), or placebo (placebo ± methotrexate or topical corticosteroids). Other studies (9/25, 36%) reported mixed results of no statistically significant difference and either statistically higher (8/25, 32%) or lower rates (1/25, 4%) on upadacitinib.
Conclusion
Most studies suggested that upadacitinib has no statistically significant difference in the studied safety outcomes compared to active treatments or placebo in patients with RA, PsA, AS, AD, UC, and CD. A few studies reported higher rates, but findings were inconsistent with limited interpretation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Upadacitinib is an orally administered, selective, and reversible Janus kinase inhibitor approved for the treatment of several immune-mediated inflammatory diseases including rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis, non-radiographic axial spondylarthritis, atopic dermatitis, ulcerative colitis, and Crohn’s disease, but data on its safety versus advanced therapies are limited. |
A systematic literature review of indirect and direct treatment comparisons of randomized controlled trials was conducted to evaluate upadacitinib in the following eight safety outcomes: any adverse events, serious adverse events, adverse events leading to discontinuation, major adverse cardiovascular event, venous thromboembolism, malignancies, infections or serious infections, and death. |
Serious adverse events, any adverse events, and adverse events leading to discontinuation were commonly studied outcomes. Rheumatoid arthritis was the most studied condition, followed by atopic dermatitis and ulcerative colitis. |
Most studies (16/25, 64%) reported no statistically significant difference in the rates of safety outcomes between upadacitinib and other active treatments (e.g., tumor necrosis factor blockers, interleukin receptor antagonists, integrin receptor antagonists, T cell co-stimulation modulator), or placebo (placebo ± methotrexate or placebo ± topical corticosteroids). |
Other studies (9/25, 36%) reported mixed results of no statistically significant difference and either statistically higher (8/25, 32%) or lower rates (1/25, 4%) on upadacitinib. |
Introduction
Immune-mediated inflammatory diseases (IMIDs) encompass a wide range of rheumatologic, dermatologic, and gastrointestinal conditions, including rheumatoid arthritis (RA), psoriatic arthritis (PsA), ankylosing spondylitis (AS), non-radiographic axial spondylarthritis (nr-axSpA), atopic dermatitis (AD), ulcerative colitis (UC), and Crohn’s disease (CD) [1], which lack a definitive etiology and are characterized by activation of inflammatory pathways. With an estimated collective prevalence of 5% to 7% in Western countries, IMIDs pose a substantial burden for patients and society [2].
Despite the lack of curative treatments for IMIDs, the landscape of disease-modifying antirheumatic drugs (DMARDs) has evolved substantially over the past two decades with the emergence of novel therapeutic options. Compared with conventional synthetic DMARDs (csDMARDs) that have a dampening effect on the whole immune system, newer biologic DMARDs (bDMARDs) and targeted synthetic DMARDs (tsDMARDs) are more selective [3].
Upadacitinib is an orally administered, selective, and reversible Janus kinase (JAK) inhibitor that has been approved by the US Food and Drug Administration (FDA), European Medicines Agency (EMA), and other regulatory authorities for the treatment of patients with moderately to severely active RA, active PsA, active AS, active nr-axSpA with objective signs of inflammation, moderate to severe AD, moderately to severely active UC, and moderately to severely active CD [4,5,6,7,8]. The approvals of upadacitinib in these conditions were based on its pivotal trials, including SELECT phase III program for RA [9], SELECT-PsA 1 and SELECT-PsA 2 for PsA [10, 11], SELECT-AXIS 1 and SELECT-AXIS 2 for AS and nr-axSpA [12, 13], Measure Up 1, Measure Up 2, and AD Up for AD [14, 15], U-ACHIEVE and U-ACCOMPLISH for UC [16], and U-EXCEED, U-EXCEL, and the U-ENDURE maintenance for CD [17,18,19].
While evaluating the efficacy of upadacitinib, these clinical trials systematically collected safety data, the analyses of which demonstrate a favorable benefit–risk profile for upadacitinib in each of the seven indications [16, 20, 21]. Given that individual clinical trials for upadacitinib have not been statistically powered to compare the rates of any safety outcomes, many safety analyses have been conducted by synthesizing the results of multiple trials to provide more robust safety evidence. Additionally, an active treatment arm was only included in a few clinical trials, including two studies in RA (SELECT-COMPARE and SELECT-CHOICE), one study in PsA (SELECT-PsA 1), and one study in AD (Heads Up), which directly evaluated upadacitinib vs. adalimumab, abatacept, or dupilumab. No active treatments were included in other upadacitinib clinical trials to allow direct comparisons of the safety profiles between upadacitinib and other active therapies.
Given the lack of safety evidence for upadacitinib across RA, PsA, AS, nr-axSpA, AD, UC, and CD, a systematic literature review (SLR) of indirect and direct treatment comparison studies of randomized controlled trials (RCTs) was conducted to assess the safety profile of upadacitinib vs. active treatments with other mechanisms of action or placebo (including placebo ± methotrexate [in RA], and placebo ± topical corticosteroids [in AD], and placebo alone in other conditions). The present study focused on assessing safety outcomes including overall AE categories (i.e., any AEs, serious AEs [SAEs], AEs leading to discontinuation) [10, 11, 13, 14, 16, 22, 23] and the AEs of special interest (AESIs) (i.e., major adverse cardiovascular event [MACE], venous thromboembolism [VTE], malignancy, infection or serious infection, and death).
Methods
The SLR was designed, performed, and reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines [24]. Specifically, a search of (1) Ovid MEDLINE and Epub Ahead of Print, In-Process, In-Data-Review & Other Non-Indexed Citations, Daily and Versions; (2) Embase; and (3) Cochrane Database of Systematic Reviews was conducted on August 3, 2022 to identify published indirect and direct treatment comparisons reporting safety outcomes of upadacitinib in RA, PsA, AS, nr-AxSpA, AD, UC, and CD, which was further augmented by a manual search via advanced search on Google Scholar.
Inclusion and Exclusion Criteria
Table 1 lists the inclusion and exclusion criteria for the SLR, which were defined according to the elements of Population, Interventions, Comparators, Outcomes, and Study Design (PICOS) [25]. The primary eligibility criteria were indirect treatment comparisons (e.g., network meta-analysis [NMA], Bucher comparison, matching-adjusted indirect comparison, and simulated treatment comparison) and direct treatment comparisons (i.e., meta-analysis [MA]) that assessed the following eight safety outcomes in patients with RA, PsA, AS, nr-AxSpA, AD, UC, and CD treated with upadacitinib: any AEs, SAEs, AEs leading to discontinuation, MACE, VTE, malignancies, infections or serious infections, and death.
Search Strategy
Database searches were conducted using a combination of free text (i.e., keywords), subject headings (e.g., Medical Subject Headings terms in MEDLINE and Emtree terms in Embase), and combined (e.g., with a Boolean operator) search terms in the following domains: (1) diseases (e.g., RA), (2) treatments (e.g., upadacitinib), and (3) study type (e.g., NMA). Detailed search terms and strategies for the three searched databases are provided in Supplementary Material Table S1. The search was restricted to English language publications of human studies, and to 2018 and later to reflect the recent treatment landscape.
Level I and II Screening and Data Extraction
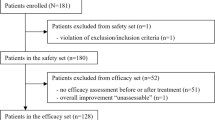
Study selection involved three steps—namely, two levels of article screening and data extraction (Fig. 1). The criteria listed in Table 1 were used as a guideline to ensure consistency in the decision to include or exclude a study.
For level I screening, the title and abstract of identified studies were independently screened by two reviewers after removing duplicates. Any discrepancy between reviewers in the decision to include/exclude a publication was resolved by a third reviewer. Citations that did not match the eligibility criteria were excluded at level I. In cases where a decision could not be made to include or exclude an article on the basis of the title and abstract, the full text was assessed at level II.
For level II screening, the full texts of publications identified from level I screening were independently reviewed by the two reviewers according to the inclusion/exclusion criteria. Any discrepancy between reviewers in the decision to include/exclude a publication was resolved by the third reviewer. Articles retained from this process were used for data extraction. A PRISMA flow diagram of the study selection process that includes the reasons for excluding publications at each level of screening and list of articles selected for data extraction is shown in Fig. 2.
Study-level information (e.g., interventions, number of trials included, upadacitinib dosage) and safety outcomes (e.g., whether a statistically significant difference was reported between upadacitinib and other active treatments/placebo) were extracted from the selected studies. The data extraction was independently performed by two reviewers to ensure accuracy. A third reviewer was consulted to reach a consensus in case of disagreement on inclusion or exclusion decisions or extracted information. As the objective of this study was to directionally assess the safety of upadacitinib, the extraction was focused on statistical significance of comparisons. That is, whether one study reported that upadacitinib had statistically significantly higher, lower, or comparable safety outcomes than a comparator. Additionally, only studies reporting licensed dosages of upadacitinib were included, i.e., 15 mg once daily (QD) for RA, PsA, AS, and nr-axSpA; 15 and 30 mg QD for AD; and 15, 30, and 45 mg QD for UC and CD [26, 27].
Ethical Approval
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Results
Study Selection
The PRISMA flow diagram for the study selection process is shown in Fig. 2. A total of 3951 unique studies were identified, which included 3949 studies from the systematic search and two studies from the supplemental manual search. After level I screening of titles and/or abstracts and level II screening of the full texts based on the inclusion/exclusion criteria, a total of 62 studies were eligible for data extraction, including 35 indirect treatment comparisons, 24 direct treatment comparisons, and 3 studies that evaluated both indirect and direct treatment comparison results. For the last three studies, data from the indirect and direct treatment comparisons were extracted separately to maximize data utilization. Therefore, a total of 38 indirect treatment comparisons (35 indirect treatment comparisons, and the data of indirect treatment comparison from the 3 studies that included both indirect and direct treatment comparisons) and 27 direct treatment comparisons (24 direct treatment comparisons, and the data of direct treatment comparison from the 3 studies that included both indirect and direct treatment comparisons) were reviewed and further selected on the basis of safety outcomes reported with licensed dosages of upadacitinib.
Of the 38 indirect treatment comparison studies, 23 compared at least one of the safety outcomes between patients who received upadacitinib at the licensed dosage vs. active treatments and/or placebo (Fig. 3). The other 15 studies were excluded for the following reasons: no results were reported for any of the eight safety outcomes (N = 6); the study only reported data for the JAKi drug class, without specific data on upadacitinib (N = 4); or the results were not for a licensed dosage of upadacitinib or no upadacitinib dosage was specified (N = 5).
Of the 27 direct treatment comparison studies from which data were extracted, only three reported results with a licensed dosage of upadacitinib for at least one of the eight safety outcomes (Fig. 4). The other 24 studies were excluded for the following reasons: no results were reported for any of the eight safety outcomes (N = 2); the study only reported data for the JAKi drug class, without specific data on upadacitinib (N = 12); the results were not for a licensed dosage of upadacitinib or no upadacitinib dosage was specified (N = 7); or the study reported results based on a single trial (N = 3).
The SLR ended up including 25 indirect and direct treatment comparison studies, including 22 NMAs, 2 MAs, and 1 study with both an NMA and MA, which all evaluated at least one of the eight safety outcomes in patients treated with upadacitinib at a licensed dosage. To separately assess the safety of upadacitinib vs. other active treatments and upadacitinib vs. placebo, we stratified the 25 studies into the following three categories: studies comparing upadacitinib with other active treatments only, comparing upadacitinib with placebo only, and comparing upadacitinib with both active treatments and placebo (Figs. 3 and 4). For the third category, data for upadacitinib vs. active treatments and upadacitinib vs. placebo were separately extracted to maximize data utilization.
Study Characteristics
Characteristics of the 25 indirect and direct treatment comparison studies published between 2019 and 2022 that were included in the SLR are shown in Table 2. The time point of safety outcome assessment ranged from weeks 4 to 104, with most studies reporting outcomes at weeks 12–24. The most studied active treatments were tumor necrosis factor (TNF) blockers (e.g., adalimumab, golimumab), interleukin (IL) receptor antagonists (e.g., ustekinumab, dupilumab), integrin receptor antagonist (vedolizumab), and T cell co-stimulation modulator (abatacept). Overall, SAEs and AEs leading to discontinuation were the most studied outcomes. Deaths were not reported in any of these 25 studies. RA was the most studied condition, followed by UC and AD. There was no study reporting any of the eight safety outcomes in nr-axSpA.
Summary of Safety Outcomes
Table 3 shows the number of indirect and direct treatment comparison studies by safety outcome by condition. The distribution of statistical significance comparing upadacitinib with other treatments is provided in Supplementary Material Fig. S1.
Among the 25 studies, 13 reported results from the comparison of upadacitinib with active treatments (Table 4 and Supplementary Material Fig. S2) and 20 reported results from the comparison of upadacitinib with placebo (Table 5 and Supplementary Material Fig. S3). For studies that included both comparisons, data were separately extracted for upadacitinib vs. active treatments and upadacitinib vs. placebo.
Results by Safety Outcome
Summary of Key Findings
Table 6 summarizes the key findings for the comparison of upadacitinib vs. active treatment or placebo, by safety outcome.
Any AEs
Any AEs were reported in three studies that compared upadacitinib with active treatments, with any AEs assessed during week 4–14. Any AEs were reported in nine studies that compared upadacitinib with placebo, with any AEs assessed during week 4–24.
Of the three studies evaluating upadacitinib vs. active treatments (Fig. 5), two (one in RA [28] and one in UC [29]) found no statistically significant differences in the rate of any AEs between upadacitinib and active treatments including TNF blockers (adalimumab, golimumab, and infliximab), IL-12/23 receptor antagonist (ustekinumab), sphingosine 1-phosphate receptor modulator (ozanimod), and integrin receptor antagonist (vedolizumab). Although one study in UC [30] reported statistically significantly higher event rates with upadacitinib than with some TNF blockers (adalimumab 160/80 mg QD, golimumab, and infliximab) as well as ustekinumab, ozanimod, and vedolizumab, no statistically significant difference was found between upadacitinib and adalimumab 80/40 mg QD.
Of the nine studies comparing upadacitinib with placebo (Fig. 6), four (two in UC [27, 29], one in PsA [31], and one in CD [32]) found no statistically significant difference in any AE rates between groups. Although two studies in AD [26, 33] reported statistically significantly higher event rates with upadacitinib 30 mg QD than with placebo, there was no statistically significant difference in the event rates between upadacitinib 15 mg QD and placebo. Three studies (one each in RA [34], AD [35], and UC [30]) found that the rate of any AEs was statistically significantly higher with upadacitinib than with placebo.
SAEs
SAEs were reported in nine studies that compared upadacitinib with active treatments during week 4–26. SAEs were reported in 12 studies comparing upadacitinib with placebo during week 4–24 (N = 12) and week 44–54 (N = 1), with one study reporting SAEs during both induction phase and maintenance phase.
Of the nine studies of upadacitinib vs. active treatments (Fig. 7), eight (four in RA [28, 36,37,38], two in UC [29, 30], and one each in AD [39] and AS[40]) found no statistically significant differences in SAE rates between upadacitinib and TNF blockers (adalimumab, golimumab, and infliximab), IL-4/13 receptor antagonist (dupilumab), IL-17A receptor antagonist (secukinumab), IL-12/23 receptor antagonist (ustekinumab), IL-13 receptor antagonist (tralokinumab), sphingosine 1-phosphate receptor modulator (ozanimod), and integrin receptor antagonist (vedolizumab). One study in CD [32] suggested that event rates were statistically significantly higher with upadacitinib than with risankizumab; however, there were no statistically significant differences between upadacitinib and TNF blockers (adalimumab, certolizumab pegol), IL-12/23 receptor antagonist (ustekinumab), or integrin receptor antagonist (vedolizumab).
Of the 12 studies comparing upadacitinib with placebo (Fig. 8), 11 (two in RA [34, 41], three in UC [29, 30, 42], three in AD [33, 35, 39], and one each in PsA [31], CD [32], and AS [40]) showed no statistically significant differences between groups. One study in RA [43] reported a statistically significantly higher event rate with upadacitinib than with placebo.
AEs Leading to Discontinuation
AEs leading to discontinuation were reported in six studies comparing upadacitinib with active treatments during week 4–54 and in nine studies comparing upadacitinib with placebo during week 4–54.
Of the six studies comparing upadacitinib with active treatments (Fig. 9), four (three in RA [28, 44, 45] and one in AD [39]) found no statistically significant difference in the rates of AEs leading to discontinuation between upadacitinib and TNF blockers (adalimumab, golimumab, infliximab, etanercept, and certolizumab pegol), IL-4/13 receptor antagonist (dupilumab), IL-6 receptor antagonist (tocilizumab), IL-13 receptor antagonist (tralokinumab), T cell co-stimulation modulator (abatacept), and CD20-directed cytolytic antibody (rituximab). One study in UC [30] reported significantly lower event rates with upadacitinib than with two TNF blockers (adalimumab and infliximab) and integrin receptor antagonist (vedolizumab), whereas no statistically significant difference was detected in the event rates between upadacitinib and another TNF blocker (golimumab) or sphingosine 1-phosphate receptor modulator (ozanimod). Although upadacitinib was associated with statistically significantly higher event rates than risankizumab and vedolizumab in one study in CD [32], there were no statistically significant differences in the rates of AEs leading to discontinuation observed between upadacitinib and TNF blockers (adalimumab, certolizumab pegol) or IL-12/23 receptor antagonist (ustekinumab).
Of the nine studies comparing upadacitinib with placebo (Fig. 10), seven (two each in RA [41, 45] and AD [35, 39], and one each in UC [27], CD [32], and PsA [46]) found no statistically significant difference in the event rats between groups. Two studies in UC that reported results for different upadacitinib dosages [30, 42] showed that there was no statistically significant difference in event rate between upadacitinib 15 or 30 mg QD and placebo; the rate was statistically significantly lower with an upadacitinib dosage of 45 mg QD.
MACE
MACE was reported in one study that compared upadacitinib with active treatments or placebo (time point of outcome assessment was not reported). In this study in RA [47], there was no statistically significant difference in MACE rate between upadacitinib and TNF blocker (adalimumab) or T cell co-stimulation modulator (abatacept). Similarly, this study [47] found no statistically significant difference in MACE rate between upadacitinib and placebo.
VTE
VTE was reported in one study comparing upadacitinib with active treatments (time point of outcome assessment was not reported), and in three studies comparing upadacitinib with placebo (two studies assessed VTE during week 12–26 while one study did not report time point). In one study in RA [47], there was no statistically significant difference in VTE rate between upadacitinib and TNF blockers (adalimumab, etanercept), T cell co-stimulation modulator (abatacept), or placebo; and in the other two studies in RA [34, 48], there was no statistically significant difference in VTE rate between upadacitinib and placebo.
Malignancy
In the only study in RA that reported malignancy as an outcome at week 12 [34], there was no statistically significant difference in the rate between upadacitinib and placebo.
Infections/Serious Infections
Infections/serious infections were reported in one study comparing upadacitinib with active treatments during week 12–52, and in four studies comparing upadacitinib with placebo during week 6–104. In the study in RA [49], there was no statistically significant difference in the rate of infections or serious infections between upadacitinib and TNF blockers (adalimumab, etanercept). Of the four studies comparing upadacitinib with placebo, one study in RA [50] and one study in UC [42] reported no statistically significant difference in the rates of serious infections between upadacitinib and placebo. The other two studies [34, 49] reported that upadacitinib was associated with a statistically significantly higher rate of infections compared with placebo, although there was no statistically significant difference between groups in the rate in serious infections.
Discussion
We systematically summarized 25 studies that compared seven safety outcomes of upadacitinib with active treatments or placebo for seven distinct IMID conditions. Overall AEs (any AEs, SAEs, and AEs leading to discontinuation) were more frequently reported than AESIs (MACE, VTE, malignancy, and infections/serious infections). Among the seven conditions, rheumatologic conditions (RA, PsA, and AS) were the most studied, followed by gastrointestinal (UC and CD) and then dermatologic (AD) conditions. There was no study reporting any studied outcomes for patients with nr-axSpA or death.
Overall, the study findings indicate that upadacitinib has a comparable safety profile to active treatments with other mechanisms of action (e.g., TNF blockers, IL receptor antagonists, and integrin receptor antagonist) and placebo across RA, PsA, AS, AD, UC, and CD within the treatment durations as reported in the studies.
Twenty-one of the studies reported the four overall AEs during the treatment periods as specified in these studies. Specifically, 11 studies compared upadacitinib and other active treatments, and 16 studies compared upadacitinib to placebo. Among the 11 studies comparing upadacitinib and other active treatments, eight studies (73%) reported no statistically significant differences in these overall AEs across RA, AD, and AS [28, 36,37,38,39,40, 44, 45]; one study (9%) reported that upadacitinib subjects had better safety outcomes in AEs leading to discontinuation in UC [30]; two studies (18%) reported mixed results (no statistically significant difference and statistically significantly worse outcomes) in the rates of any AEs in UC [29, 30]; and one study (9%) reported mixed results (no statistically significant difference and significantly worse outcomes) in the rates of SAE and AEs leading to discontinuation in CD [32]. Among the 16 studies comparing upadacitinib to placebo, nine studies (56%) reported no statistically significant differences across RA, PsA, AS, AD, UC, and CD [27, 29, 31, 32, 39,40,41, 45, 46]; one study (6%) reported no statistically significant difference in the rates of SAEs, and significantly better outcomes for AEs leading to discontinuation in UC [42]; one study (6%) reported mixed results (no statistically significant difference, statistically significantly worse, or significantly better outcomes) for different outcomes in UC [30]; and five studies (31%) reported statistically significantly worse outcomes in RA and AD [26, 33,34,35, 43].
Out of the four specific AESIs (MACE, VTE, malignancy, and infection/serious infections), results suggested comparable rates between patients receiving upadacitinib and patients receiving other active treatments or placebo. On the basis of one study synthesizing evidence from 42 phase II and III RCTs, our review suggested that upadacitinib has no statistically significant difference in the rates of MACE or VTE in RA compared to TNF blockers, T cell co-stimulation modulator, and placebo [13]. While there was no study assessing upadacitinib vs. active treatment for malignancy, one study in RA (which was based on two phase III RCTs) suggested comparable safety rates between upadacitinib and placebo within the short-term treatment period [34]. Similarly, one RA study suggested that upadacitinib has similar rates in both infections and serious infections compared to TNF blockers [49]. All four of the studies (100%) comparing upadacitinib vs. placebo suggested that upadacitinib has no significant differences in the rates of serious infections [34, 42, 49, 50], while 2/4 (50%) reported statistically higher infection rates on upadacitinib [34, 49].
Although the majority of these studies (16/25, 64%) reported no overall statistically significant differences in rates of all examined safety outcomes associated with upadacitinib vs. active treatment or placebo, a few studies reported statistically significantly higher (8/25, 32%) or statistically significantly lower (1/25, 4%) event rates on certain safety outcomes. For example, one study in CD reported inconsistent trends when comparing upadacitinib to IL receptor antagonists. Specifically, this paper reported that upadacitinib was associated with statistically significantly higher rates of AEs leading to discontinuation compared with risankizumab (IL-23 receptor antagonist) but was not statistically significantly different from ustekinumab (IL-12/23 receptor antagonist) [32]. Future research studies are warranted to investigate the rates of AEs leading to discontinuations between upadacitinib and IL receptor antagonists. Similarly inconsistent trends were also found in two studies in RA [34, 49] that reported both risks of infection and serious infection. Specifically, statistically significantly higher risk of infections was reported among patients who received upadacitinib compared to placebo; however, there were no reported differences between upadacitinib and placebo in the risks of serious infections. We recommend to interpret such studies with caution [34].
Moreover, the heterogeneity across clinical trials needs to be considered when interpreting the statistically significantly higher rates in “any AEs” of upadacitinib compared to placebo in five studies [26, 30, 33,34,35]. Specifically, “any AE” often contains an overly broad and heterogeneous group of events, many of which may not be relevant to the condition of interest. As a result of differences in the characteristics of trials and patients, the proportion of patients experiencing “any AE” or the incidence rates of “any AE” may not be comparable across trials and across conditions. To examine whether any individual AE could explain the higher rate for “any AE”, we reviewed the reported safety data for individual clinical trials [14,15,16, 51,52,53,54] included in these studies [26, 30, 33,34,35]. On the basis of these individual clinical trials, the incidences of infection and acne were numerically higher in patients receiving upadacitinib than patients receiving placebo, although no test results of statistical significance were reported between arms. In addition, the majority of the acne cases in AD were mild or moderate and did not require medical intervention [55]. Future studies with sufficient statistical power are warranted to further assess the impact of these itemized AEs.
Compared to efficacy outcomes which are usually standardized and well powered across RCTs, safety outcomes need to be assessed with additional considerations in the context of indirect and direct treatment comparison because of the heterogeneity in clinical trial designs. First, in each clinical trial, the length of the placebo-controlled or active controlled period determines up to what time points safety outcomes can be compared using randomized controlled evidence. However, this length can differ across trials. Also, safety profile may not be fully characterized during the short time periods studied in the clinical trials. Second, although SAEs, AEs leading to treatment discontinuation, and AESIs have been commonly reported in clinical trials, the incidence of each of these AE types was typically low during the randomization period, which might lead to a poorer model fit or unstable estimates in indirect or direct treatment comparisons compared to those of efficacy outcomes. Third, the definitions of safety outcomes can differ across trials (e.g., adjudicated and unadjudicated AEs) and different drugs might have unique safety profiles that are not necessarily comparable. Fourth, patient characteristics that may modify the risk of developing safety events might be different across trials, e.g., the underlying comorbidities or medication use. In addition, trials may apply different methodologies for the collection, assessment, and analysis of AEs. These heterogeneities combined indicate the challenges of assessing safety outcomes across treatments and should be carefully examined when assessing the feasibility of indirect and direct treatment comparison for safety outcomes or when interpreting the findings.
The current SLR focused on indirect and direct treatment comparisons that reported licensed dosage of upadacitinib. As a validation, we also reviewed the indirect and direct treatment comparisons that did not specify dosage or included unlicensed dosages. Overall, our findings were supported by these studies. For example, one study in CD included patients treated with unlicensed dosages of upadacitinib (i.e., 3, 6, 12, or 24 mg two times a day and 24 mg QD), and reported that there were no statistically significant differences in the rates of any AE between upadacitinib and TNF blockers (adalimumab, certolizumab pegol, and infliximab), IL-12/23 receptor antagonist (ustekinumab), and integrin receptor antagonist (vedolizumab) [56]. Similarly, we reviewed one study in PsA [57] and one study in AD [58] which did not specify upadacitinib dosage and concluded that upadacitinib has comparable risk of MACE compared to TNF blockers (adalimumab, certolizumab pegol, etanercept, golimumab), IL-17A receptor antagonist (secukinumab), IL-23 receptor antagonist (guselkumab), and phosphodiesterase 4 inhibitor (apremilast). The same two studies also reported that upadacitinib has comparable risks of VTE relative to placebo. Finally, one study in RA included patients treated with unlicensed dosage of upadacitinib and reported that upadacitinib has comparable risk of deaths compared to placebo [59].
In both regulatory review and clinical practice, balancing benefits and risks of interventions is of vital importance. In the consideration of the comparable safety profiles between upadacitinib and other active treatments, it is suggested to incorporate the comparative efficacy of these drugs to assist therapeutic decision-making.
Strengths
To our knowledge, this is the first SLR study of indirect and direct treatment comparisons of RCTs evaluating the safety outcomes of upadacitinib vs. other active treatments or placebo across seven IMID conditions. Unlike a typical SLR of clinical trials, the current SLR reviewed evidence from 25 indirect and direct treatment comparisons of RCTs across a broad range of conditions that included rheumatologic (RA, PsA, and AS), dermatologic (AD), and gastrointestinal (UC and CD) therapeutic areas. As the literature search was restricted to 2018 and later, most recently approved treatments for these conditions were included, providing a comprehensive view of the current treatment landscape for IMIDs. Moreover, only studies reporting a licensed dosage of upadacitinib were included in an effort to evaluate the safety of upadacitinib more accurately. The safety outcomes analyzed in the study included overall AEs as well as AESIs. Lastly, a high degree of granularity was achieved by separately summarizing results by outcome, condition, and drug class.
Limitations
As with all SLRs, this study had certain limitations. Although the aim of this study was to comprehensively evaluate the safety profile of upadacitinib based on eight outcomes, none of the included studies evaluated death and only a few studies reported results for MACE, VTE, and malignancy. Similarly, there were no indirect or direct treatment comparison studies in nr-axSpA. Since the current SLR was conducted with the search date of August 3, 2022, future SLRs (such as an update of the current SLR) can be considered when more evidence becomes available. Moreover, the underlying clinical trials included in these indirect and direct treatment comparison studies were heterogeneous. For example, patients may have heterogenous baseline characteristics across different trials, which may modify the risk of developing safety events. Furthermore, many clinical trials assessed safety outcomes within a short period of time (e.g., 4, 6, or 12 weeks). Although the AEs were reported during the randomization period, the incidence rates were too low to conclude any well-powered statistical comparisons. Future real-world studies with longer follow-up time were warranted to further assess the safety profile of upadacitinib. Because this study assessed the overall safety profile of upadacitinib across seven conditions, only qualitative results of statistical difference were extracted; however, a detailed quantitative analysis of specific outcomes or conditions can also yield important information regarding the safety outcome of upadacitinib. Given these limitations, the study findings were validated against existing literature and similar findings were reported.
Conclusion
This SLR evaluated the safety outcomes of upadacitinib vs. other active treatment or placebo through indirect and direct treatment comparisons of RCTs. Most studies showed that upadacitinib has no statistically significant difference rates of studied safety outcomes compared to other active treatments (including TNF blockers, IL receptor antagonists, and integrin receptor antagonist) and placebo across RA, PsA, AS, AD, UC, and CD. In a minority of studies, higher rates of some safety outcomes were reported on upadacitinib, but findings were inconsistent with limited interpretation.
Data Availability
The datasets generated during and/or analyzed in this study are publicly available.
References
McInnes IB, Gravallese EM. Immune-mediated inflammatory disease therapeutics: past, present and future. Nat Rev Immunol. 2021;21(10):680–6.
El-Gabalawy H, Guenther LC, Bernstein CN. Epidemiology of immune-mediated inflammatory diseases: incidence, prevalence, natural history, and comorbidities. J Rheumatol Suppl. 2010;85:2–10.
Nash P, Kerschbaumer A, Dörner T, et al. Points to consider for the treatment of immune-mediated inflammatory diseases with Janus kinase inhibitors: a consensus statement. Ann Rheum Dis. 2021;80(1):71–87.
Therapeutic Goods Administration. RINVOQ [Package Insert], Australia. 2023. https://www.ebs.tga.gov.au/ebs/picmi/picmirepository.nsf/pdf?OpenAgent&id=CP-2020-PI-01075-1. Accessed June 9, 2023.
European Medicines Agency. RINVOQ [Package Insert]. 2023. https://www.ema.europa.eu/en/documents/product-information/rinvoq-epar-product-information_en.pdf. Accessed June 9, 2023.
Electronic Medicines Compendium. RINVOQ [Package Insert], United Kingdom. 2023. https://www.medicines.org.uk/emc/files/pil.10972.pdf. Accessed June 9, 2023.
Drug and Health Product Register. RINVOQ [Package Insert], Canada. 2023. https://pdf.hres.ca/dpd_pm/00070449.PDF. Accessed June 9, 2023.
US Food and Drug Administration. RINVOQ [Package Insert], United States. 2023. https://www.accessdata.fda.gov/drugsatfda_docs/label/2023/211675s015lbl.pdf. Accessed June 9, 2023.
Conaghan PG, Mysler E, Tanaka Y, et al. Upadacitinib in rheumatoid arthritis: a benefit-risk assessment across a phase III program. Drug Saf. 2021;44(5):515–30.
McInnes IB, Anderson JK, Magrey M, et al. Trial of upadacitinib and adalimumab for psoriatic arthritis. N Engl J Med. 2021;384(13):1227–39.
Mease PJ, Lertratanakul A, Anderson JK, et al. Upadacitinib for psoriatic arthritis refractory to biologics: SELECT-PsA 2. Ann Rheum Dis. 2021;80(3):312–20.
van der Heijde D, Song IH, Pangan AL, et al. Efficacy and safety of upadacitinib in patients with active ankylosing spondylitis (SELECT-AXIS 1): a multicentre, randomised, double-blind, placebo-controlled, phase 2/3 trial. Lancet. 2019;394(10214):2108–17.
van der Heijde D, Baraliakos X, Sieper J, et al. Efficacy and safety of upadacitinib for active ankylosing spondylitis refractory to biological therapy: a double-blind, randomised, placebo-controlled phase 3 trial. Ann Rheum Dis. 2022;81(11):1515–23.
Guttman-Yassky E, Teixeira HD, Simpson EL, et al. Once-daily upadacitinib versus placebo in adolescents and adults with moderate-to-severe atopic dermatitis (Measure Up 1 and Measure Up 2): results from two replicate double-blind, randomised controlled phase 3 trials. Lancet. 2021;397(10290):2151–68.
Reich K, Teixeira HD, de Bruin-Weller M, et al. Safety and efficacy of upadacitinib in combination with topical corticosteroids in adolescents and adults with moderate-to-severe atopic dermatitis (AD Up): results from a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2021;397(10290):2169–81.
Danese S, Vermeire S, Zhou W, et al. Upadacitinib as induction and maintenance therapy for moderately to severely active ulcerative colitis: results from three phase 3, multicentre, double-blind, randomised trials. Lancet. 2022;399(10341):2113–28.
ClinicalTrials.gov. A study of the efficacy and safety of upadacitinib (ABT-494) in participants with moderately to severely active Crohn's disease who have inadequately responded to or are intolerant to biologic therapy. 2022. https://clinicaltrials.gov/ct2/show/NCT03345836?term=NCT03345836&draw=2&rank=1. Accessed June 9, 2023.
ClinicalTrials.gov. A study of the efficacy and safety of upadacitinib in participants with moderately to severely active Crohn's disease who have inadequately responded to or are intolerant to conventional and/or biologic therapies (U-EXCEL). 2022. https://clinicaltrials.gov/ct2/show/NCT03345849?term=NCT03345849&draw=2&rank=1. Accessed June 9, 2023.
ClinicalTrials.gov. A maintenance and long-term extension study of the efficacy and safety of upadacitinib (ABT-494) in participants with Crohn's disease who completed the studies M14-431 or M14-433. https://clinicaltrials.gov/ct2/show/NCT03345823?term=NCT03345823&draw=2&rank=1. Accessed June 9, 2023.
Burmester GR, Cohen SB, Winthrop KL, et al. Safety profile of upadacitinib over 15 000 patient-years across rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis and atopic dermatitis. RMD Open. 2023;9(1):e002735.
Panes J, Loftus EJ, Lacerda A, et al. S37 efficacy and safety of upadacitinib maintenance therapy in patients with moderately to severely active Crohn’s disease: U-ENDURE phase 3 results. Am J Gastroenterol. 2022;117:S10.
van Vollenhoven R, Takeuchi T, Pangan AL, et al. Efficacy and safety of upadacitinib monotherapy in methotrexate-naive patients with moderately-to-severely active rheumatoid arthritis (SELECT-EARLY): a multicenter, multi-country, randomized, double-blind, active comparator-controlled trial. Arthritis Rheumatol. 2020;72(10):1607–20.
Deodhar A, Van den Bosch F, Poddubnyy D, et al. Upadacitinib for the treatment of active non-radiographic axial spondyloarthritis (SELECT-AXIS 2): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2022;400(10349):369–79.
Hutton B, Salanti G, Caldwell DM, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162(11):777–84.
Amir-Behghadami M, Janati A. Population, intervention, comparison, outcomes and study (PICOS) design as a framework to formulate eligibility criteria in systematic reviews. Emerg Med J. 2020;37(6):387.
Wan H, Jia H, Xia T, Zhang D. Comparative efficacy and safety of abrocitinib, baricitinib, and upadacitinib for moderate-to-severe atopic dermatitis: a network meta-analysis. Dermatol Ther. 2022;35(9):e15636.
Li Y, Yao C, Xiong Q, et al. Network meta-analysis on efficacy and safety of different Janus kinase inhibitors for ulcerative colitis. J Clin Pharm Ther. 2022;47(7):851–9.
Sung YK, Lee YH. Comparative study of the efficacy and safety of tofacitinib, baricitinib, upadacitinib, and filgotinib versus methotrexate for disease-modifying antirheumatic drug-naïve patients with rheumatoid arthritis. Z Rheumatol. 2021;80(9):889–98.
Lasa JS, Olivera PA, Danese S, Peyrin-Biroulet L. Efficacy and safety of biologics and small molecule drugs for patients with moderate-to-severe ulcerative colitis: a systematic review and network meta-analysis. Lancet Gastroenterol Hepatol. 2022;7(2):161–70.
Burr NE, Gracie DJ, Black CJ, Ford AC. Efficacy of biological therapies and small molecules in moderate to severe ulcerative colitis: systematic review and network meta-analysis. Gut. 2022;71(10):1976–87.
Lee YH, Song GG. Relative efficacy and safety of Janus kinase inhibitors for the treatment of active psoriatic arthritis: a network meta-analysis. Z Rheumatol. 2021;82(5):408–16.
Barberio B, Gracie DJ, Black CJ, Ford AC. Efficacy of biological therapies and small molecules in induction and maintenance of remission in luminal Crohn’s disease: systematic review and network meta-analysis. Gut. 2023;72(2):264–74.
Pereyra-Rodriguez J-J, Alcantara-Luna S, Domínguez-Cruz J, et al. Short-term effectiveness and safety of biologics and small molecule drugs for moderate to severe atopic dermatitis: a systematic review and network meta-analysis. Life. 2021;11(9):927.
Wang F, Sun L, Wang S, et al. Efficacy and safety of tofacitinib, baricitinib, and upadacitinib for rheumatoid arthritis: a systematic review and meta-analysis. Mayo Clin Proc. 2020;95(7):1404–19.
Qiu M, Duan XY, Yin DG. Network meta-analysis on the efficacy and safety of upadacitinib in adolescents and adults with moderate-to-severe atopic dermatitis. Int J Dermatol. 2022;61(1):e24–6.
Lee YH, Song GG. Relative efficacy and safety of tofacitinib, baricitinib, upadacitinib, and filgotinib in comparison to adalimumab in patients with active rheumatoid arthritis. Z Rheumatol. 2020;79(8):785–96.
Song GG, Choi SJ, Lee YH. Comparison of the efficacy and safety of tofacitinib and upadacitinib in patients with active rheumatoid arthritis: a Bayesian network meta-analysis of randomized controlled trials. Int J Rheum Dis. 2019;22(8):1563–71.
Song GG, Lee YH. Comparative efficacy and safety of 15 and 30 mg upadacitinib administered to patients with active rheumatoid arthritis: a Bayesian network meta-analysis of randomized controlled trials. Z Rheumatol. 2020;79(1):103–11.
Drucker AM, Morra DE, Prieto-Merino D, et al. Systemic immunomodulatory treatments for atopic dermatitis: update of a living systematic review and network meta-analysis. JAMA Dermatol. 2022;158(5):523–32.
Lee YH. Comparative efficacy and safety of Janus kinase inhibitors and secukinumab in patients with active ankylosing spondylitis: a systematic review and meta-analysis. Pharmacology. 2022;107(11–12):537–44.
Lee YH, Song GG. Comparative efficacy and safety of tofacitinib, baricitinib, upadacitinib, filgotinib and peficitinib as monotherapy for active rheumatoid arthritis. J Clin Pharm Ther. 2020;45(4):674–81.
Panaccione R, Collins E, Melmed G, et al. OP34 Efficacy and safety of advanced induction and maintenance therapies in patients with moderately to severely active ulcerative colitis: an indirect treatment comparison using Bayesian network meta-analysis. J Crohns Colitis. 2022;16(Supplement_1):i037–41.
Lee YH, Song GG. Comparative efficacy and safety of tofacitinib, baricitinib, upadacitinib, and filgotinib in active rheumatoid arthritis refractory to biologic disease-modifying antirheumatic drugs. Z Rheumatol. 2021;80(4):379–92.
Cacciapaglia F, Venerito V, Stano S, Fornaro M, Lopalco G, Iannone F. Comparison of adalimumab to other targeted therapies in rheumatoid arthritis: results from systematic literature review and meta-analysis. J Pers Med. 2022;12(3):353.
Weng C, Xue L, Wang Q, Lu W, Xu J, Liu Z. Comparative efficacy and safety of Janus kinase inhibitors and biological disease-modifying antirheumatic drugs in rheumatoid arthritis: a systematic review and network meta-analysis. Ther Adv Musculoskelet Dis. 2021;13:1759720X21999564.
McInnes IB, Sawyer LM, Markus K, LeReun C, Sabry-Grant C, Helliwell PS. Targeted systemic therapies for psoriatic arthritis: a systematic review and comparative synthesis of short-term articular, dermatological, enthesitis and dactylitis outcomes. RMD Open. 2022;8(1):e002074.
Alves C, Penedones A, Mendes D, Marques FB. Risk of cardiovascular and venous thromboembolic events associated with Janus kinase inhibitors in rheumatoid arthritis: a systematic review and network meta-analysis. J Clin Rheumatol. 2022;28(2):69–76.
Bilal J, Riaz IB, Naqvi SAA, et al. Janus kinase inhibitors and risk of venous thromboembolism: a systematic review and meta-analysis. Mayo Clin Proc. 2021;96(7):1861–73.
Alves C, Penedones A, Mendes D, Marques FB. The risk of infections associated with JAK inhibitors in rheumatoid arthritis: a systematic review and network meta-analysis. J Clin Rheumatol. 2022;28(2):e407–14.
Bechman K, Subesinghe S, Norton S, et al. A systematic review and meta-analysis of infection risk with small molecule JAK inhibitors in rheumatoid arthritis. Rheumatology. 2019;58(10):1755–66.
Burmester GR, Kremer JM, Van den Bosch F, et al. Safety and efficacy of upadacitinib in patients with rheumatoid arthritis and inadequate response to conventional synthetic disease-modifying anti-rheumatic drugs (SELECT-NEXT): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet. 2018;391(10139):2503–12.
Genovese MC, Fleischmann R, Combe B, et al. Safety and efficacy of upadacitinib in patients with active rheumatoid arthritis refractory to biologic disease-modifying anti-rheumatic drugs (SELECT-BEYOND): a double-blind, randomised controlled phase 3 trial. Lancet. 2018;391(10139):2513–24.
Guttman-Yassky E, Thaçi D, Pangan AL, et al. Upadacitinib in adults with moderate to severe atopic dermatitis: 16-week results from a randomized, placebo-controlled trial. J Allergy Clin Immunol. 2020;145(3):877–84.
Fleischmann R, Pangan AL, Song IH, et al. Upadacitinib versus placebo or adalimumab in patients with rheumatoid arthritis and an inadequate response to methotrexate: results of a phase III, double-blind, randomized controlled trial. Arthritis Rheumatol. 2019;71(11):1788–800.
Mendes-Bastos P, Ladizinski B, Guttman-Yassky E, et al. Characterization of acne associated with upadacitinib treatment in patients with moderate-to-severe atopic dermatitis: a post hoc integrated analysis of 3 phase 3 randomized, double-blind, placebo-controlled trials. J Am Acad Dermatol. 2022;87(4):784–91.
Wu G, Yang Y, Liu M, Wang Y, Guo Q. Systematic review and network meta-analysis: comparative efficacy and safety of biosimilars, biologics and JAK1 inhibitors for active Crohn disease. Front Pharmacol. 2021;12:655865.
Ajmal MBJ, Naqvi S, Riaz I, et al. Risk of major adverse cardiovascular events (MACE) with biologic and targeted synthetic antirheumatic agents in psoriatic arthritis: a systematic review and network meta-analysis. Arthritis Rheumatol. 2021;73(suppl 9).
Chen TL, Lee LL, Huang HK, Chen LY, Loh CH, Chi CC. Association of risk of incident venous thromboembolism with atopic dermatitis and treatment with Janus kinase inhibitors: a systematic review and meta-analysis. JAMA Dermatol. 2022;158(11):1254–61.
Xie W, Zhang Z. SAT0159 Association between Janus kinase inhibitors and all-cause mortality in patients with rheumatoid arthritis. Ann Rheum Dis. 2020;79(Suppl 1):1020–1020.
Medical Writing, Editorial, and Other Assistance.
Medical writing was provided by Janice Imai, an employee of Analysis Group, Inc., and sponsored by AbbVie, Inc.
Authorship.
All authors agree to be accountable for all aspects of the work and have read and approved the final manuscript.
Funding
This research and the journal’s Rapid Service Fee were sponsored by AbbVie, Inc.
Author information
Authors and Affiliations
Contributions
All authors, i.e., Eduardo Mysler, Gerd R. Burmester, Christopher D. Saffore, John Liu, Lani Wegrzyn, Chelsey Yang, Keith A. Betts, Yan Wang, Alan D. Irvine, Remo Panaccione, contributed to study conception and design and drafting and critical revision of the article for important intellectual content and approved the final version. All authors agree to be accountable for all aspects of this study.
Corresponding author
Ethics declarations
Conflict of Interest
Christopher Saffore, John Liu, and Lani Wegrzyn are employees of AbbVie, Inc. Chelsey Yang, Keith A. Betts, and Yan Wang are employees of Analysis Group, Inc., which received research funding from AbbVie, Inc. Eduardo Mysler received grants and consulting fees from AbbVie, Amgen, AstraZeneca, Novartis, Lilly, Pfizer, Roche, BMS, Sandoz, GSK, Janssen, Sanofi, Hi Bio Inc., Gemmene and Gema Biotech. Gerd R. Burmester received honoraria for lectures and consulting fees from AbbVie, Amgen, BMS, Lilly, Galapagos, Janssen, Novartis, Pfizer, Sanofi, Roche, Celltrion, Chugai and MSD. Alan D. Irvine received grants or consulting fees or advisory board honoraria from AbbVie, Almirall, Arena, Benevolent AI, Connect Biopharma, Lilly, Janssen, LEO Pharma, Novartis, Pfizer, RAPT Therapeutics, Regeneron, UCB, Sanofi. He is on the board of directors of the International Eczema Council. Remo Panaccione received consulting fees from Abbott, AbbVie, Abbivax, Alimentiv (formerly Robarts), Amgen, Arena Pharmaceuticals, AstraZeneca, Biogen, Boehringer Ingelheim, Bristol-Myers Squibb, Celgene, Celltrion, Cosmos Pharmaceuticals, Eisai, Elan, Eli Lilly, Ferring, Galapagos, Fresenius Kabi, Genentech, Gilead Sciences, GlaxoSmithKline, JAMP Bio, Janssen, Merck, Mylan, Novartis, Oppilan Pharma, Organon, Pandion Pharma, Pendopharm, Pfizer, Progenity, Prometheus Biosciences, Protagonist Therapeutics, Roche, Sandoz, Satisfai Health, Shire, Sublimity Therapeutics, Takeda Pharmaceuticals, Theravance Biopharma, Trellus, Viatris, Ventyx, UCB; has received speaker’s fees from AbbVie, Amgen, Arena Pharmaceuticals, Bristol-Myers Squibb, Celgene, Eli Lilly, Ferring, Fresenius Kabi, Gilead Sciences, Janssen, Merck, Organon, Pfizer, Roche, Sandoz, Shire, Takeda Pharmaceuticals; and has served on advisory boards for AbbVie, Alimentiv (formerly Robarts), Amgen, Arena Pharmaceuticals, AstraZeneca, Biogen, Boehringer Ingelheim, Bristol-Myers Squibb, Celgene, Eli Lilly, Ferring, Fresenius Kabi, Genentech, Gilead Sciences, GlaxoSmithKline, JAMP Bio, Janssen, Merck, Mylan, Novartis, Oppilan Pharma, Organon, Pandion Pharma, Pfizer, Progenity, Protagonist Therapeutics, Roche, SandozShire, Sublimity Therapeutics, Takeda Pharmaceuticals, Ventyx.
Ethical Approval
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Mysler, E., Burmester, G.R., Saffore, C.D. et al. Safety of Upadacitinib in Immune-Mediated Inflammatory Diseases: Systematic Literature Review of Indirect and Direct Treatment Comparisons of Randomized Controlled Trials. Adv Ther 41, 567–597 (2024). https://doi.org/10.1007/s12325-023-02732-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-023-02732-6