Abstract
Introduction
Erosive esophagitis (EE) is a severe form of gastroesophageal reflux disease commonly treated with proton pump inhibitors (PPIs). The aim of this retrospective, observational cohort study was to describe the characteristics and healthcare burden of patients with EE.
Methods
We identified adults in the USA with an EE diagnosis between January 1, 2016 and February 28, 2019 in a linked dataset containing electronic health records (EHR) from the Veradigm Network EHR and claims data from Komodo Health. Patients were required to have 1 year of baseline data and 3 years of follow-up data. Patients were stratified by the number of PPI lines of therapy (LOT) during the 4-year study period. We descriptively captured patient characteristics and treatment patterns, along with all-cause and EE-related healthcare utilization and costs.
Results
Among the 158,347 qualifying adults with EE, 71,958 (45.4%) had 1 PPI LOT, 14,985 (9.5%) had 2 LOTs, 15,129 (9.6%) had 3+ LOTs, and 56,275 (35.5%) did not fill a PPI prescription. Omeprazole and pantoprazole comprised more than 70% of any LOT, with patients commonly switching between the two. Mean (standard deviation) annualized all-cause and EE-related healthcare costs in the follow-up period were $16,853 ($70,507) and $523 ($3659), respectively. Both all-cause and EE-related healthcare costs increased with LOTs.
Conclusions
Patients with EE are commonly treated with prescription PPIs; however, 19.0% of patients cycled through multiple PPIs. Higher PPI use was associated with a higher comorbidity burden and higher healthcare costs compared to 0 PPI use.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Erosive esophagitis (EE) is a complication of gastroesophageal reflux disease that is commonly treated with proton pump inhibitors (PPI). |
This study examined the real-world prescription PPI treatment patterns, healthcare resource utilization, and costs of patients with a clinical diagnosis of EE in the USA. |
What was learned from this study? |
During a 4-year observation period, we observed low persistence with PPI therapy and frequent cycling between omeprazole and pantoprazole. |
Patients who had more lines of PPI therapy had a higher burden of gastrointestinal-related comorbidities and higher healthcare costs. |
Introduction
Gastroesophageal reflux disease (GERD) impacts roughly 20–30% of the US population and is marked by recurrent reflux of gastric contents into the esophagus [1]. Persistent exposure to gastric acid leads to damage of the esophageal epithelium resulting in erosive esophagitis (EE) in approximately 30–40% of patients with GERD [2, 3]. Patients with EE are at increased risk of complications, such as Barrett’s esophagus/esophageal adenocarcinoma and gastrointestinal (GI) bleeding [4]. In 2015, US healthcare expenditures for esophageal disorders exceeded $18 billion [5].
Proton pump inhibitors (PPIs) are widely used medications that suppress gastric acid secretion and can lead to esophageal mucosal healing, as in the case of GERD complicated by EE [6]. In fact, PPI therapy is the recommended first step in the healing of EE, according to American College of Gastroenterology (ACG) guidelines [7]. ACG further recommends maintenance PPI therapy for patients with severe EE (Los Angeles [LA] grade C–D [8]) or Barrett’s esophagus and in patients with LA grade A–B EE whose symptoms recur when PPI treatment is stopped.
Up to half of the patients with GERD report persistent symptoms while on PPI therapy [9], and clinicians will commonly increase PPI dose, switch PPI, or augment with a different medication within 6 months [10]. The odds of having a partial response to therapy versus resolution of symptoms are three times higher among patients being treated for EE or Barrett’s esophagus. The real-world use of PPIs among patients with EE in the USA has not been studied. This descriptive analysis presents the real-world treatment patterns, healthcare resource utilization, and costs for patients with a diagnosis of EE between 2015 and 2022.
Methods
Data Sources
This retrospective, observational cohort study of individuals in the USA used electronic health records (EHR) from the Veradigm Network EHR-linked with insurance claims data from the Komodo Health Healthcare Map from January 1, 2015 to February 28, 2022 (hereafter, “the linked dataset”). The data types have been previously described in Shah et al. [11].
The linked dataset only contains de-identified data as per the de-identification standard defined in Section §164.514(a) of the Health Insurance Portability and Accountability Act of 1996 (HIPAA) Privacy Rule. The process by which the data is de-identified is attested to through a formal determination by a qualified expert as defined in Section §164.514(b) (1) of the HIPAA Privacy Rule. Because this study used only de-identified patient records, it is therefore no longer subject to the HIPAA Privacy Rule and is therefore exempt from institutional review board approval and for obtaining informed consent according to US law. This study was conducted in compliance with the Declaration of Helsinki and used only de-identified data.
Diagnoses and procedure codes used in this study are listed in Table S1 in the supplementary material. The coding systems used for this analysis included International Classification of Diseases, 9th and 10th Edition, Clinical Modification (ICD-9-CM and ICD-10-CM) diagnosis codes and Clinical Procedure Terminology procedure codes (CPT).
Patient Selection
We identified all patients with a clinical diagnosis of GERD with esophagitis, i.e., those with at least one ICD-10-CM diagnostic code for GERD with esophagitis (K21.0, K21.00, or K21.01), between January 1, 2016 and February 28, 2022. The K21.0 code was used in reimbursement claims prior to October 1, 2020 to code for any GERD with esophagitis. After October 1, 2020 the K21.00 code was used to code for GERD with esophagitis without bleeding, whereas the K21.01 code was used to code for GERD with esophagitis with bleeding, such as blood in vomit or tarry stool. In this analysis, patients with any of these three codes were considered to have a clinical diagnosis of EE.
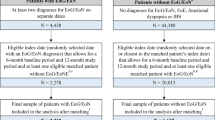
The earliest date of an EE code within this time frame was defined as the index date. We required that all patients were at least 18 years old on the index date and had at least 12 months of EHR data and claims enrollment before the index date and 36 months of EHR data and claims enrollment after the index date. On the basis of these inclusion criteria, patients could only qualify for the study if their index date of EE diagnosis was before February 28, 2019. Patient selection is summarized in Fig. 1.
Study Periods
For this study, we used a 12-month baseline period, a 36-month follow-up period, and a combined 4-year observation period. The study design is described in Fig. 2.
Study Variables
The primary outcome of interest was the prescription PPI treatment patterns during the 4-year observation period. The six PPIs included in the study were pantoprazole, lansoprazole, omeprazole, esomeprazole, rabeprazole, and dexlansoprazole. Only claims data were used to identify medications.
We captured PPI lines of therapy (LOT) for all patients with at least one PPI prescription during their 4-year observation period. A LOT started on the fill date and continued until the earliest of the following: PPI switch, a gap in PPI therapy of at least 45 days, or the end of their 4-year observation period. Patients who switched or had a gap in therapy of at least 45 days were considered non-persistent, while those who did not switch or had a gap in therapy of less than 45 days between the start of their LOT and the end of the observation period were considered persistent. A 45-day gap in therapy was chosen because it gives patients a grace period to refill their prescription and has been used in previous literature [12].
For persistent patients, we captured whether their therapy was augmented with a dose increase of at least 90% or they filled at least one prescription for an H2 receptor antagonist during the LOT. For non-persistent patients, we identified the subset who switched to a new PPI with or without a gap in PPI therapy of at least 45 days (switch), those who restarted their medication after a gap in therapy of at least 45 days (restart), and those with a gap in therapy who had no further evidence of prescription PPI use (discontinuation). For patients who restarted their medication and then switched to a new medication, only the switch was included in the analysis. For this analysis, only PPI switches were considered a new LOT.
For the first three LOTs, we captured the duration of the LOT, the time to the next LOT, and other medications prescribed during the LOT (antidepressants, baclofen, Carafate, H2 receptor antagonists, and other antacids).
Patient Characteristics
Demographic characteristics were recorded as of the index date. We recorded body mass index (BMI) and general clinical conditions in the 12-month baseline period. GI-related comorbidities and symptoms that occurred during the 36-month follow-up period were recorded. We also recorded the occurrence of any diagnostic esophagogastroduodenoscopy (EGD) on the index date or during the 12-month baseline period.
Healthcare Utilization and Costs
Utilization and cost outcomes were measured using medical and drug claims data. All-cause healthcare resource utilization included all office visits, lab services, radiology services, and outpatient prescriptions captured in the claims data. EE-related costs included inpatient medical claims with an EE diagnosis as the admitting diagnosis, outpatient medical claims with an EE diagnosis in any position, and pharmacy claims for a PPI. Costs were captured for the full 3-year follow-up period, reported as per person per year (annualized), and were adjusted to February 2022 US dollars using the medical care component of the Consumer Price Index [13].
Data Analysis
This analysis was descriptive in nature. We presented categorical measures as number (N) and percentages, while we presented continuous measures as mean and standard deviation (SD). For cost measures, when 50% or more of the individuals used a service category, we also reported the median and interquartile range. Descriptive statistics were generated using SAS V9.4.
Sensitivity Analysis
To increase the confidence our results were representative of true EE cases, we conducted a sensitivity analysis of patients with documentation of an EGD on the index date or within the 12-month baseline period (in addition to the ICD-10 diagnostic codes K21.0, K21.00, or K21.01). For these patients, we similarly recorded age, sex, number of LOTs, and all-cause healthcare utilization and costs in the follow-up period. It should be noted that EGD results were not available in the structured data source for this analysis; therefore, we can only confirm that an EGD was performed not that the EGD confirmed a diagnosis of EE.
Results
We identified 158,347 adults with EE who qualified for study inclusion and comprised the main analytic cohort. Of these, 72,658 (45.9%) had a diagnostic EGD either on the index date or in the 12-month baseline period. Patients were, on average, 56.9 (SD 14.3) years old, 61.1% were female, 60.9% were White, 6.9% were Black, and 7.2% were Hispanic (Table 1). They carried a high comorbidity burden, including 50.9% with hypertension, 46.6% with obesity, and 43.4% with hyperlipidemia based on baseline period data (Table S2 in the supplementary material). In the 36-month follow-up period, 31.9% had a diagnosis of hiatal hernia, 12.6% had a diagnosis of peptic ulcer, and 12.1% had a diagnosis of Barrett’s esophagus. GI-related symptoms were also common in the follow-up period and included 24.7% with dyspepsia, 23.4% with dysphagia, and 12.4% with heartburn.
Overall, 45.4% (N = 71,958) had evidence of 1 PPI LOT, 9.5% (N = 14,985) had evidence of 2 PPI LOTs, and 9.6% (N = 15,129) had evidence of 3+ PPI LOTs during the 4-year observation period. By comparison, 35.5% of patients (N = 56,275) did not fill a prescription for a PPI during the 4-year observation period (Fig. 1).
In the baseline period, many general comorbidities, including cardiovascular disease (55.4% vs. 71.6%) and diabetes (19.9% vs. 31.0%), were less common among patients with 0 PPI LOTs than those with 3+ PPI LOTs. We also observed large differences in baseline rates of opioid use (19.0% vs. 55.9%), abdominal pain (27.0% vs. 53.3%), and chest pain (23.1% vs. 37.5%) between patients with 0 PPI LOTs vs. those with 3+ PPI LOTs.
During the 36-month follow-up period, the most common GI-related comorbidities among all cohorts were hiatal hernia, peptic ulcer, and Barrett’s esophagus. The most common GI-related symptoms in the follow-up period were dyspepsia and dysphagia. The percentage of patients with these GI-related comorbidities and symptoms increased with an increase in the number of PPI LOTs (Fig. 3).
Treatment Characteristics
During the 4-year observation period, 102,072 (64.5%) patients with EE diagnosis were prescribed at least one prescription PPI, and 81.9% of these patients received either omeprazole (48.6%) or pantoprazole (33.2%) as their first LOT (Table 2). Use of the other PPIs increased slightly across LOTs, but more than 70% of patients in the second and third LOT received either omeprazole or pantoprazole. Among those with omeprazole as a first LOT, 73.7% had pantoprazole as a second LOT, whereas among those with pantoprazole as a first LOT, 61.9% had omeprazole as a second LOT (Fig. S1 in the supplementary material).
Treatment patterns were measured for the first three lines of therapy (Table 2). Only 11.4% (N = 11,613) of treated patients were persistent with their first LOT. Among the 11,613 patients who were persistent with their first LOT, 12.7% augmented with a dose increase of at least 90%, and 16.8% augmented with an H2 receptor agonist. Among the 88.6% (N = 90,459) of patients who were non-persistent with their first LOT, roughly one-third switched to a different PPI, one-third restarted their index PPI without evidence of subsequent switching, and one-third discontinued without any subsequent prescription PPI use.
The proportion of patients who were persistent increased slightly in the second (12.6%) and third (15.6%) LOT, but more than 80% of patients were non-persistent (Table 2). However, the reason for non-persistence shifted as patients became more likely to switch medications rather than restart or fully discontinue prescription PPIs. In addition, the percentage of switchers who did so without a gap in therapy of at least 45 days increased from 45.1% in the first LOT to 67.2% and 74.6% in the second and third LOT, respectively.
With respect to the timing of the LOTs, among all patients with at least one PPI prescription during the observation period, the mean (SD) time from the start of the observation period to the start of the first LOT was 9.9 (11.1) months. The mean (SD) gap in therapy between the first and second LOT was 7.8 (10.5) months, and the mean (SD) gap in therapy between the second and third LOT was 3.5 (6.8) months. The mean (SD) duration of LOT among persistent patients in the first, second, and third LOT was 2.67 (1.46) years, 1.29 (1.16) years, and 1.22 (1.09) years, respectively. By comparison, the mean duration of LOT among non-persistent patients in the first, second, and third LOT was 0.56 (0.73) years, 0.32 (0.47) years, and 0.32 (0.46) years, respectively.
Among those with a first LOT, 33.1% received at least one prescription for antidepressants, 15.0% for an H2 receptor antagonist, 9.2% for Carafate, and 3.3% for baclofen (Table 2). As the number of LOTs increased, there were slight increases in the proportion of patients who received prescriptions for these medications during the respective LOTs.
Healthcare Utilization and Costs
Mean (SD) annualized healthcare costs for all patients with EE in the 36-month follow-up period were $16,853 ($70,507) (Fig. 4a). In all service categories, healthcare costs were higher in patients with more PPI LOTs (Table S3 in the supplementary material). Consequently, annualized all-cause healthcare costs were $16,713 higher in patients with 3+ LOTs than among patients with 0 LOTs. This was driven by greater utilization of inpatient and pharmacy services.
On average, 3.1% ($523 [$3659]) of mean annualized all-cause healthcare costs could be directly attributed to EE (Table S3 in the supplementary material). Despite large differences in total healthcare costs, the percentage attributable to EE varied only slightly between LOT cohorts, ranging from 2.9% for patients with 2 LOTs to 3.3% for patients with either 0 or 3+ LOTs. EE-related utilization increased with increasing numbers of PPI LOTs. In each service category, annualized EE-related costs in the follow-up period increased with increasing numbers of PPI LOTs. Mean (SD) annualized EE-related costs were 2.4 times higher in patients with 3+ PPI LOTs ($924 [$6609]) than in patients with 0 PPI LOTs ($380 [$4233]) (Fig. 4b).
Diagnostic EGD Sensitivity Analysis
We conducted a sensitivity analysis of the subset of the 72,658 patients with documentation of a diagnostic EGD on the index date or in the baseline period, in addition to the diagnostic codes for erosive esophagitis. Patients in the EGD subset were, on average, 56.2 (13.8) years old at index, and 60.8% were female, which is consistent with the overall EE cohort (Table S4 in the supplementary material). Overall, 32.1% of patients in the EGD subset did not fill a prescription for a PPI during the 4-year observation period. In the EGD subset, 46.1% had evidence of 1 PPI LOT, 10.7% had evidence of 2 PPI LOTs, and 11.2% had evidence of 3+ PPI LOTs during the 4-year observation period. Mean (SD) annualized all-cause healthcare costs in the 3-year follow-up period were similar between the overall EE and EGD subset ($16,853 [$70,507] vs. $17,565 [$69,889]).
Discussion
In this study of patients with EE in the USA, 19.0% of patients had more than 1 PPI LOT during a 4-year observation period encompassing a 12-month baseline period and 36 months of follow-up. We observed low persistence with PPI therapy and frequent cycling, most often between omeprazole and pantoprazole. As patients progressed through multiple lines of PPI therapy, the frequency of PPI discontinuations and restarts on the same medication became less common, and switching became more common. Patients who are cycling through multiple PPI LOTs had a higher healthcare burden, including GI-related comorbidities and symptoms, along with greater healthcare utilization and costs.
Notably, only 45.9% of patients had evidence of a diagnostic EGD on or before their index EE diagnosis, but we found many patients were starting PPI treatment before their index EE diagnosis. This treatment pattern is consistent with current GERD treatment guidelines, which recommend starting PPI treatment prior to EGD as part of the differential diagnosis; however, an EGD, with a pause in PPI therapy prior to the procedure, would then be required to confirm the EE diagnosis [7]. It is unclear why so many patients received an EE diagnosis without a diagnostic EGD, but it may reflect the necessity of coding in real-world clinical practice where patients may not consent to or have insurance coverage for the procedure. That said, the sensitivity analysis of the subset of patients with an EGD indeed still identified similar trends as the primary analytic cohort.
While there is no previously published data on PPI use in the USA by patients with EE, PPI treatment patterns have been previously examined in the US Veteran population with uncomplicated GERD between 2002 and 2007 [14, 15]. Similar to our study, omeprazole was the most commonly used first-line PPI [14, 15]. Among Veterans whose PPI therapy lasted at least 6 months, 31.7% switched to a different PPI, which is consistent with the switching rate of 29.5% observed in this EHR-claims-linked study.
For some patients, the numerous lines of PPIs may not have been a result of insufficient acid suppression but perhaps a result of side effects, comorbidities, dosing optimization, an enhanced brain–gut axis, hypersensitivity, or cognitive-affective disorders [16, 17]. In addition, a recent emphasis on the potential risks of PPIs has led to a decrease in the prescribing of these medications. This may all lead to cycling if physicians start treatment empirically, stop prescribing PPIs to assess severity, and reinitiate PPIs when symptoms return [18].
PPIs are effective at acid suppression and mucosal healing in patients, and there is little difference in effectiveness observed between PPIs when they are taken as directed, i.e., prior to meals on an empty stomach [19, 20]. However, some patients have persistent symptoms that may be attributed to an excess of acid exposure or insufficient gastric acid suppression. For example, a meta-analysis found that the rapid metabolizer genotype of cytochrome P450 2C19 was associated with being refractory to PPIs [21]. In these patients, more potent and durable acid-suppressive agents may provide superior results; however, insurance formularies often require failure with at least one first-generation PPI before covering newer formulations, even though the former are heavily metabolized by CYP2C19.
While LA grade is not documented in the structured EHR, the newer ICD-10 codes introduced in October 1, 2020 do differentiate between EE with and without bleeding. Future work could explore differences in costs between patients with and without bleeding using these newer codes. Other potential future directions include a deeper exploration of the diagnostic and therapeutic procedures used in this population or an investigation into the associated between specific comorbidities and frequent PPI cycling.
Limitations
This analysis is limited by the wide availability of over-the-counter PPIs. As over-the-counter medications are not captured in claims data, it is likely that the numbers reported in this study are an underestimate of both PPI use in the EE population and the cost burden of EE. A survey of patients with GERD reported that 32% of patients using PPIs were purchasing them over the counter [10]. Patients were not required to be newly diagnosed, so we may not be fully capturing PPI switching. Furthermore, patients with mild EE may be underestimated in this analysis if they are using only over-the-counter medication and not seeking medical care for their condition.
Additionally, cohort construction is based on a claims-based diagnosis of EE, and our main study cohort likely includes an unknown proportion of patients with non-erosive reflux disease or LA grade A esophagitis. In the sensitivity analysis, we required that patients have evidence of a prior diagnostic EGD; however, this does not fully resolve the issue as the results were not available in the structured EHR data used in this study. Additionally, the optimal use of PPIs cannot be measured in this study [22].
Finally, this retrospective study used routinely collected claims and EHR data and is subject to the typical limitations of using data not gathered for specific research purposes. The dataset used in this analysis only included insured individuals and may not be representative of the uninsured population.
Conclusions
Prescription PPI use is common among patients with EE, but persistence with medication is low. A subset of patients tended to cycle through PPIs, and these patients had more comorbidities and higher all-cause and EE-related healthcare costs.
Data Availability
The data that support the findings of this study were used under license from Veradigm and Komodo Health. Due to data use agreements and its proprietary nature, restrictions apply regarding the availability of the data. Further information is available from the corresponding author.
References
El-Serag HB, Sweet S, Winchester CC, Dent J. Update on the epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut. 2014;63:871–80.
Pisegna J, Holtmann G, Howden CW, et al. Review article: oesophageal complications and consequences of persistent gastro-oesophageal reflux disease. Aliment Pharmacol Ther. 2004;20(Suppl 9):47–56.
Savarino E, de Bortoli N, De Cassan C, et al. The natural history of gastro-esophageal reflux disease: a comprehensive review. Dis Esophagus. 2017;30:1–9.
Ronkainen J, Talley NJ, Storskrubb T, et al. Erosive esophagitis is a risk factor for Barrett’s esophagus: a community-based endoscopic follow-up study. Am J Gastroenterol. 2011;106:1946.
Peery AF, Crockett SD, Murphy CC, et al. Burden and cost of gastrointestinal, liver, and pancreatic diseases in the United States: update 2018. Gastroenterology. 2019;156:254–272.e11.
Strand DS, Kim D, Peura DA. 25 years of proton pump inhibitors: a comprehensive review. Gut Liver. 2017;11:27–37.
Katz PO, Dunbar KB, Schnoll-Sussman FH, Greer KB, Yadlapati R, Spechler SJ. ACG clinical guideline for the diagnosis and management of gastroesophageal reflux disease. Am J Gastroenterol. 2022;117:27–56.
Armstrong D, Bennett JR, Blum AL, et al. The endoscopic assessment of esophagitis: a progress report on observer agreement. Gastroenterology. 1996;111:85–92.
Delshad SD, Almario CV, Chey WD, Spiegel BMR. Prevalence of gastroesophageal reflux disease and proton pump inhibitor-refractory symptoms. Gastroenterology. 2020;158:1250–1261.e2.
Ruigómez A, Johansson S, Wernersson B, Fernández Cantero O, García Rodríguez LA. Gastroesophageal reflux disease in primary care: using changes in proton pump inhibitor therapy as an indicator of partial response. Scand J Gastroenterol. 2012;47:751–61.
Shah S, Cappell K, Sedgley R, et al. Diagnosis and treatment patterns among patients with newly diagnosed Helicobacter pylori infection in the United States 2016–2019. Sci Rep. 2023;13:1375.
Birnbaum H, Greenberg PE, Tang J, et al. Antidepressant treatment patterns and costs among US employees. J Med Econ. 2009;12:36–45.
Measuring price change in the CPI: medical care. Consumer Price Index. 2022. https://www.bls.gov/cpi/factsheets/medical-care.htm. Accessed 2022 Sep 20.
Gawron AJ, Pandolfino JE, Miskevics S, Lavela SL. Proton pump inhibitor prescriptions and subsequent use in US veterans diagnosed with gastroesophageal reflux disease. J Gen Intern Med. 2013;28:930–7.
Gawron AJ, Pandolfino J, Miskevics S, LaVela SL. Initial proton pump inhibitor characteristics associated with long-term prescriptions in US veterans diagnosed with gastro-oesophageal reflux disease. J Pharm Health Serv Res. 2014;5:157–64.
Konturek PC, Brzozowski T, Konturek SJ. Stress and the gut: pathophysiology, clinical consequences, diagnostic approach and treatment options. J Physiol Pharmacol. 2011;62:591–9.
Sharma P, Yadlapati R. Pathophysiology and treatment options for gastroesophageal reflux disease: looking beyond acid. Ann N Y Acad Sci. 2021;1486:3–14.
Targownik LE, Fisher DA, Saini SD. AGA clinical practice update on de-prescribing of proton pump inhibitors: expert review. Gastroenterology. 2022;162:1334–42.
Li B-Z, Threapleton DE, Wang J-Y, et al. Comparative effectiveness and tolerance of treatments for Helicobacter pylori: systematic review and network meta-analysis. BMJ. 2015;351: h4052.
Graham DY, Tansel A. Interchangeable use of proton pump inhibitors based on relative potency. Clin Gastroenterol Hepatol. 2018;16:800–808.e7.
Ichikawa H, Sugimoto M, Sugimoto K, Andoh A, Furuta T. Rapid metabolizer genotype of CYP2C19 is a risk factor of being refractory to proton pump inhibitor therapy for reflux esophagitis. J Gastroenterol Hepatol. 2016;31(4):716–26.
Sheikh I, Waghray A, Waghray N, Dong C, Wolfe MM. Consumer use of over-the-counter proton pump inhibitors in patients with gastroesophageal reflux disease. Am J Gastroenterol. 2014;109:789–94.
Acknowledgements
Medical Writing/Editorial Assistance
Medical writing support was provided by Jessamine Winer-Jones, PhD an employee of Veradigm. This support was funded by Phathom Pharmaceuticals.
Funding
This study was funded by Phathom Pharmaceuticals. This funding included payment of fees for Rapid Service and Open Access.
Author information
Authors and Affiliations
Contributions
RY contributed to conceptualization, investigation, methodology, visualization, and lead development of the manuscript. SCS contributed to conceptualization, investigation, methodology, visualization, and writing of the manuscript. MB and KC contributed to conceptualization, formal analysis, funding acquisition, investigation, methodology, project administration, supervision, validation, data visualization and writing of the manuscript. RJ and CP contributed to conceptualization, funding acquisition, investigation, methodology, project administration, supervision, data visualization and writing of the manuscript. RS contributed to conceptualization, data curation, formal analysis, investigation, methodology, software, validation, visualization, and critical review and editing of the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
Shailja Shah is a consultant for Phathom Pharmaceuticals and RedHill Biopharma. Rena Yadlapati is a consultant for Phathom Pharmaceuticals and Reckitt Benckiser and owns stock in RJS Mediagnostix. Katherine Cappell, Robert Sedgley, and Machaon Bonafede are employees of Veradigm, which received funding from Phathom Pharmaceuticals to conduct this study. Corey Pelletier and Rinu Jacob are employees of Phathom Pharmaceuticals and own stock and stock options in Phathom Pharmaceuticals.
Ethical Approval
The linked dataset only contains de-identified data as per the de-identification standard defined in Section §164.514(a) of the Health Insurance Portability and Accountability Act of 1996 (HIPAA) Privacy Rule. The process by which the data is de-identified is attested to through a formal determination by a qualified expert as defined in Section §164.514(b) (1) of the HIPAA Privacy Rule. Because this study used only de-identified patient records, it is therefore no longer subject to the HIPAA Privacy Rule and is therefore exempt from institutional review board approval and for obtaining informed consent according to US law. This study was conducted in compliance with the Declaration of Helsinki and used only de-identified data.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Yadlapati, R., Cappell, K., Sedgley, R. et al. A Linked Electronic Medical Record-Claims Analysis of the Clinical and Economic Outcomes of Patients Coded for Erosive Esophagitis in the United States. Adv Ther 40, 5489–5501 (2023). https://doi.org/10.1007/s12325-023-02688-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-023-02688-7