Abstract
Introduction
Intravenous (IV) administration of iron is considered a safe and efficacious treatment for iron deficiency anemia (IDA), recommended in patients requiring rapid replenishment of iron, or intolerant or unresponsive to oral administration of iron. Recent randomized controlled trials (RCTs) have shown high incidence of hypophosphatemia after administration of two IV iron preparations: saccharated ferric oxide (SFO) and ferric carboxymaltose (FCM). The present study aimed to conduct matching-adjusted indirect comparison (MAIC) of hypophosphatemia incidence with these iron formulations and ferric derisomaltose (FDI) based on data from head-to-head RCTs conducted in Japan.
Methods
A MAIC of hypophosphatemia incidence was conducted on the basis of data from two head-to-head RCTs. The relative odds of hypophosphatemia with FDI versus SFO were obtained from patient-level data from a recent RCT and adjusted for cumulative iron dose, while parametric models of serum phosphate levels from a separate RCT were used to estimate the relative odds of hypophosphatemia with FCM with SFO. An anchored MAIC was then conducted comparing FDI with FCM.
Results
The adjusted odds of experiencing hypophosphatemia were significantly lower with FDI than SFO [odds ratio (OR) of 0.02; 95% confidence interval (CI) 0.01–0.05]. The parametric models of serum phosphate from the RCT comparing FCM with SFO provided an estimated OR of 1.17 for the incidence of hypophosphatemia with FCM versus SFO. Combining the two estimates in the MAIC showed that the odds of experiencing hypophosphatemia would be 52.5 (95% CI 27.7–99.4) times higher with FCM than FDI in patients with IDA associated with heavy menstrual bleeding in Japan.
Conclusions
Direct comparison of patient-level data and a MAIC from two RCTs in Japanese patients with heavy menstrual bleeding indicated that hypophosphatemia is less frequent in patients treated with FDI than those with FCM or SFO. Results are in agreement with RCTs comparing FDI and FCM in patients with various etiologies conducted in the USA and Europe.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Recent randomized controlled trials (RCTs) have demonstrated that certain intravenous iron formulations—notably saccharated ferric oxide (SFO) and ferric carboxymaltose (FCM)—are associated with high incidence of hypophosphatemia, typically defined as serum phosphate levels < 2.0 mg/dL for moderate hypophosphatemia or serum phosphate levels ≤ 1.0 mg/dL for severe hypophosphatemia. |
The present study quantified the relative odds of experiencing hypophosphatemia after administration of SFO, FCM, and ferric derisomaltose (FDI), the last of which has previously been shown to result in significantly lower incidence of hypophosphatemia than FCM in multiple RCTs. |
A matching-adjusted indirect comparison of FDI and FCM was conducted on the basis of two RCTs of FCM versus SFO, and FDI versus SFO in patients with heavy menstrual bleeding in Japan. |
The analysis showed that there was no significant difference in the incidence of hypophosphatemia between SFO and FCM, while FDI was associated with significantly lower incidence of hypophosphatemia than both SFO (based on head-to-head RCT data) and FCM (based on a matching-adjusted indirect comparison). |
The present analysis corroborated the findings of previous head-to-head RCTs demonstrating the significantly higher incidence of hypophosphatemia with FCM versus FDI, using data specific to the Japanese population with heavy menstrual bleeding. |
Introduction
Hypophosphatemia after administration of saccharated ferric oxide (SFO) was first documented in 1982 by Okada et al. in which two cases of osteomalacia were identified in patients with chronic anemia due to persistent intestinal bleeding; osteomalacia resolved with a reduction in the dose of SFO [1]. A subsequent series of nine patients with moderate-to-severe anemia treated with SFO reported a stepwise reduction in serum inorganic phosphate levels, resulting in hypophosphatemia within 4 weeks in all patients [2]. These findings were further corroborated by Imamura [3] who conducted a head-to-head study of SFO and ferric gluconate.
Intravenous administration of iron polymaltose has also been reported to result in hypophosphatemic osteomalacia [4]. Hypophosphatemia after administration of SFO was first considered to be caused by renal tubular damage [5]; however, SFO and iron polymaltose were later shown to cause hypophosphatemia by increasing fibroblast growth factor 23 (FGF23) levels [6]. FGF23 is a bone-derived hormone responsible for regulation of phosphate and vitamin D homeostasis, lowering serum phosphate levels by inhibiting both proximal tubular phosphate reabsorption and intestinal phosphate absorption [7]. This mechanism was initially elucidated in a small prospective study of phosphate homeostasis, in which all eight patients with iron deficiency anemia (IDA) treated with iron polymaltose experienced increased FGF23 and decreased serum phosphate levels [8].
Hypophosphatemia has also been reported after administration of ferric carboxymaltose (FCM; Ferinject®, Vifor France, Paris, France). The PHOSPHARE trial program consists of three randomized controlled trials (RCTs) comparing FCM with ferric derisomaltose (FDI; Monofer®, Pharmacosmos A/S, Holbæk, Denmark) in patients with IDA of various etiologies [9, 10]. The trials found that FCM resulted in significantly higher incidence of hypophosphatemia than FDI. Of the two high-dose iron preparations (FDI and FCM), the effect on serum phosphate levels appears to be mediated by the carbohydrate moiety in FCM rather than being a class effect of all intravenous iron preparations [11]. Specifically, FCM appears to increase levels of intact FGF23 (iFGF23), a phenomenon that has not yet been observed with FDI [9]. This effect has led to the addition of hypophosphatemia to the FCM summary of product characteristics in several territories, including the European Union, UK, Brazil, Switzerland, Australia, and the USA [12,13,14,15,16,17].
Recently, the JapicCTI-194573 RCT has been conducted in Japan comparing the safety and efficacy of FDI with SFO in patients with gynecological etiologies of IDA, finding that hypophosphatemia (defined as serum phosphate levels < 2.0 mg/dL) occurred in 8.4% (20/237) of patients treated with FDI versus 83.2% (99/119) of patients treated with SFO [18]. Severe hypophosphatemia (defined as serum phosphate levels ≤ 1.0 mg/dL) occurred in 6.7% (8/119) patients treated with SFO versus no patients treated with FDI (0/237). Decreases in blood phosphorus (as defined in version 22.0 of the Medical Dictionary for Regulatory Activities, MeDRA) were also recorded in 1.3% of patients treated with FDI versus 25.2% of patients treated with SFO.
The objectives of the present study were twofold: firstly to present more detailed results on the incidence of moderate and severe hypophosphatemia after administration of SFO and FDI in patients with heavy menstrual bleeding in the JapicCTI-194573 RCT. The second objective was to indirectly compare the incidence of hypophosphatemia with FCM versus FDI in Japan using data from JapicCTI-194573 RCT and a previous RCT comparing FCM with SFO in a similar patient population in Japan [18, 19]. Because patient-level data of serum phosphate were not available from the previous RCT, an anchored matching-adjusted indirect treatment comparison (MAIC) was conducted using patient-level data from the JapicCTI-104573 RCT (comparing FDI with SFO) and models of serum phosphate based on the summary, arm-level data from the previous RCT comparing FCM with SFO [18, 19].
Note that this article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Methods
Analysis of Hypophosphatemia Incidence in the JapicCTI-194573 RCT
Serum phosphate data from the JapicCTI-194573 RCT were analyzed to characterize changes in serum phosphate levels over time after administration of FDI and SFO. In JapicCTI-194573, the total iron need was determined on the basis of body weight and hemoglobin levels in both the FDI and SFO groups; a simplified table of iron need was used for patients weighing ≥ 40 kg while the Uchida formula was used for patients weighing < 40 kg [20]. Because of differences in the maximum daily dose of FDI and SFO (1000 mg versus 120 mg, respectively), the dosing schedules and the period over which iron was administered differed. Both formulations increased hemoglobin similarly and serum phosphate was measured at baseline, weekly for 8 weeks after the start of the treatment, and then at weeks 10 and 12. The normality of the serum phosphate distributions at each time point was visually assessed using Q–Q plots and formally tested using the Shapiro–Wilk test [21]. The significance of differences in serum phosphate levels at each time point was tested using the Mann–Whitney U test.
For reference, prior to conducting the MAIC, the unadjusted odds ratio of experiencing moderate hypophosphatemia (serum phosphate levels < 2.0 mg/dL) with FDI versus SFO was calculated on the basis of a contingency table. Odds ratios were not calculated for severe hypophosphatemia (serum phosphate levels ≤ 1.0 mg/dL) as no patients experienced severe hypophosphatemia in the FDI arm of the trial; log-rank tests were instead used to establish if the incidence of severe hypophosphatemia was significantly different in the groups of patients treated with FDI versus SFO.
Modeling of Hypophosphatemia Incidence in Ikuta et al.
No data on the absolute or relative incidence of hypophosphatemia (defined as serum phosphate levels either ≤ 1.0 mg/dL or < 2.0 mg/dL) after administration of SFO or FCM were presented in the Ikuta et al. 2019 RCT manuscript and data were therefore requested from the corresponding author on May 24, 2022 [19]. In the absence of these data, parametric distributional models of serum phosphate levels were first developed on the basis of patient-level data from the JapicCTI-194573 RCT, using maximum-likelihood estimation to derive shape and scale parameters for generalized gamma distributions of serum phosphate in the SFO arm (Supplementary Fig. 1). Specifically, generalized gamma distribution parameters were estimated from the distribution of serum phosphate concentrations in the SFO arm of the JapicCTI-194573 RCT at the time point at which the lowest mean serum phosphate values were observed. This distributional model was then adjusted to match the publicly available aggregate serum phosphate data from the 2019 Ikuta et al. RCT manuscript. The proportion of the serum phosphate distribution falling < 2.0 mg/dL was then calculated and used to estimate the proportion of patients treated with SFO and FCM with lowest serum phosphate levels < 2.0 mg/dL. Proportions of patients with serum phosphate levels ≤ 1.0 mg/dL were not evaluated because an indirect comparison of severe hypophosphatemia incidence with FCM versus FDI was not viable owing to the aforementioned lack of events occurring after administration of FDI in the JapicCTI-194573 RCT. Note that, as with the JapicCTI-194573 RCT, the same method of calculating the total iron need—based on body weight and hemoglobin level—was used for patients in the FCM and SFO groups in the Ikuta et al. trial, with maximum daily doses for FCM and SFO of 500 mg and 120 mg, respectively.
Matching-Adjusted Indirect Comparison of Hypophosphatemia (Serum Phosphate < 2.0 mg/dL)
The anchored MAIC of the relative odds of experiencing hypophosphatemia (defined as serum phosphate levels < 2.0 mg/dL) was conducted using the outputs of the parametric models of serum phosphate from the Ikuta et al. 2019 RCT combined with patient-level data from the JapicCTI-194573 RCT. A multivariable Cox proportional hazards model was fitted to the patient-level data from the JapicCTI-194573 RCT, including treatment, baseline serum phosphate concentration, cumulative iron dose, baseline hemoglobin, and body weight (and treatment–covariate interactions) as covariates, to identify prognostic factors and effect modifiers. Cumulative iron dose (p < 0.001), baseline serum phosphate (p = 0.03), and baseline weight (p = 0.01) were identified as significant effect modifiers and an anchored MAIC was therefore justified (Supplementary Table 1).
The MAIC was conducted using a logistic propensity score model, capturing cumulative iron dose, baseline hemoglobin, and body weight as effect modifiers, and using the method of moments to match the parameter distributions between the JapicCTI-194573 and Ikuta et al. 2019 RCT. Where \(\alpha\) is the vector of parameters for minimization and \(\mathrm{\rm X}\) is the matrix of centered effect-modifying parameters, the objective function was defined as follows:
The Broyden–Fletcher–Goldfarb–Shanno iterative method was used to minimize the objective function, using the derivative of the objective function as the gradient function. The contrast-based estimate was then calculated on the basis of adjusted odds ratios calculated directly from the incidence of hypophosphatemia in the JapicCTI-194573 RCT, and from the modeled incidence of hypophosphatemia from the Ikuta et al. 2019 RCT. The indirect comparison of FDI versus FCM was then conducted on the basis of the following consistency relation, relying on the adjusted odds ratio from the JapicCTI-194573 RCT [22]:
where \({d}_{\mathrm{SM}}\) is the adjusted odds ratio of experiencing hypophosphatemia with FDI versus SFO, and \({d}_{\mathrm{SF}}\) is the odds ratio of experiencing hypophosphatemia with FCM versus SFO based on the generalized gamma distribution models of serum phosphate.
All data used in the analyses were obtained from previously conducted studies and the analyses are not reliant on data from studies of human or animal participants conducted by any of the authors. Both the JapicCTI-194573 and Ikuta et al. 2019 RCTs, on which the present analysis is based, were approved by the institutional review boards (IRBs) at each participating site [18, 19]. Written informed consent for participation in the studies was obtained from all subjects and both studies were conducted in accordance with the Declaration of Helsinki and Good Clinical Practice (GCP) guidelines [18, 19].
Results
Analysis of Hypophosphatemia Incidence in the JapicCTI-194573 RCT
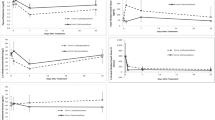
In the FDI arm of the JapicCTI-194573 RCT, the lowest average serum phosphate level occurred at visit 2, having dropped an average of 0.51 mg/dL from baseline [standard deviation (SD) 0.65 mg/dL; Fig. 1] to an average of 2.94 mg/dL (SD 0.61 mg/dL). The corresponding low in the SFO arm occurred at visit 4, having dropped an average of 1.52 mg/dL (SD 0.85 mg/dL; Fig. 1) from baseline to an average of 1.91 mg/dL (SD 0.74 mg/dL). Analysis of the normality of serum phosphate distributions over time in the JapicCTI-194573 trial showed significant non-normality at weeks 3, 4, 5, 6, 7, and 10 in the SFO arm, and at week 3 in the FDI arm (Supplementary Fig. 2); the significance of differences in moderate hypophosphatemia (serum phosphate < 2.0 mg/dL) at each timepoint was therefore tested using the non-parametric Mann–Whitney U test, which showed that there were significant differences in serum phosphate levels from week 2 to week 12 of the study (Fig. 2 and Table 1). Kaplan–Meier curves were plotted to illustrate the probabilities of patients experiencing hypophosphatemia over time (Fig. 3).
Over the trial period, the unadjusted ratio of the odds of experiencing hypophosphatemia (serum phosphate < 2.0 mg/dL) was 0.019 for FDI versus SFO. As no patients in the FDI arm of the JapicCTI-194573 RCT experienced severe hypophosphatemia (serum phosphate ≤ 1.0 mg/dL), odds ratios were not calculated and the analysis of the incidence of severe hypophosphatemia was restricted to a log-rank test. The common hazard function, H0, predicted that an expected 5.37 patients would experience severe hypophosphatemia in the FDI arm, compared with 0 patients actually observed in the RCT, versus an expected 2.63 patients experiencing severe hypophosphatemia in the SFO arm, compared with 8 that were observed in the RCT (log-rank p < 0.001; Table 2).
Modeling of Hypophosphatemia Incidence in Ikuta et al.
Based on the adjusted generalized gamma distribution models of serum phosphate levels, the modeled incidence of hypophosphatemia (serum phosphate < 2.0 mg/dL) was 94 of 119 patients (79.0%) treated with SFO versus 97 of 119 (81.5%) patients treated with FCM. Using these parametric models of serum phosphate distributions adjusted to match the data from the RCT comparing FCM with SFO yielded an estimated odds ratio of 1.17 (95% confidence interval (CI) 0.62–2.22) for the incidence of hypophosphatemia with FCM versus SFO.
Matching-Adjusted Indirect Comparison
The baseline characteristics common to the publications of the JapicCTI-194573 and Ikuta et al. RCTs are presented in Supplementary Table 2. After adjustment, the effective sample size (ESS) from the JapicCTI-194573 trial was 231, versus 356 patients in the full analysis set of the original RCT, corresponding to a 35.1% reduction. The rescaled patient-level weights had a median of 0.81 and a range spanning from 0.002 to 4.402 and, after adjustment, the cohort was well matched to that in the Ikuta et al. 2019 RCT with regard to cumulative iron dose, baseline hemoglobin, and baseline body weight (Supplementary Table 3). A histogram of the rescaled weight distribution is presented in Supplementary Fig. 3. Based on the adjusted analysis of head-to-head data from an RCT comparing FDI with SFO, the odds of experiencing hypophosphatemia were significantly lower with FDI than SFO, with an odds ratio of 0.02 (95% CI 0.01–0.05).
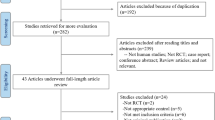
Combining the two estimates using a contrast-based approach showed that the odds of experiencing hypophosphatemia would be 52.46 (95% CI 27.68–99.42) times higher with FCM than FDI in patients with IDA associated with heavy menstrual bleeding in Japan (Fig. 4).
Outcomes of the anchored matching adjusted indirect comparison of the incidence of hypophosphatemia after administration FDI versus ferric carboxymaltose. FCM ferric carboxymaltose, FDI ferric derisomaltose, MAIC matching-adjusted indirect comparison, SFO saccharated ferric oxide, OR odds ratio, CI confidence interval
Discussion
The Ikuta et al. 2019 RCT showed that many summary phosphate parameters were similar after administration of FCM and SFO, including the proportion of patients experiencing the “blood phosphorous decreased” adverse event (18.5% versus 20.2%), the proportions of patients with phosphorous levels < 1.0 mg/dL at week 4 (9.3% versus 10.9%), and the lowest mean phosphate concentrations (1.45 ± 0.50 vs 1.54 ± 0.65 mgdL) [19].
Based on the findings of the JapicCTI-194573 and Ikuta et al. 2019 RCTs, the present MAIC showed that FDI would result in significantly lower rates of post-infusion hypophosphatemia than FCM in patients with IDA associated with heavy menstrual bleeding in Japan. The majority of the modeled effect was driven by the adjusted odds ratios from the JapicCTI-194573 trial, which showed that the odds ratio of experiencing hypophosphatemia in patients treated with FDI versus SFO was 0.02 (95% CI 0.01–0.05).
A key strength of the MAIC was the close alignment of the patient population, with all patients being female and Japanese, and with the same underlying etiology of IDA, a mean age across all four trial arms falling between 40 and 45 years, and mean baseline hemoglobin falling in the range 9.0 ± 0.25 g/dL; however, the anchored MAIC has a number of limitations that should be acknowledged when interpreting the results. While the MAIC controlled for cumulative iron dose, baseline hemoglobin, and body weight, adjustments for the timing of the iron dosing were not practicable. A comparison of the dose schedules of FDI and SFO is presented in Supplementary Fig. 4 and this may have affected the incidence of hypophosphatemia beyond the effect captured through the adjustment for cumulative iron dose. FDI and FCM can deliver more iron than SFO via a single administration, allowing for less frequent dosing, potentially resulting in fewer adverse events, particularly considering those directly related to the iron infusion. However, the Ikuta et al. RCT indicated that FCM and SFO cause hypophosphatemia with similar frequency. Despite the potential limitations, the findings of the present MAIC are comparable with previous findings from head-to-head RCTs comparing FDI and FCM in other settings and across multiple etiologies of IDA [9]. These results indicate that FDI causes less frequent hypophosphatemia than SFO and FCM.
It has been proposed that iron deficiency is associated with higher levels of C-terminal or cleaved FGF23 (cFGF23), arising from increased transcription of FGF23 [23]. The increased transcription is accompanied by increased proteolytic cleavage of iFGF23 resulting in maintenance of normal phosphate levels [11, 24]. As had been observed previously in patients with autosomal dominant hypophosphatemic rickets, phosphaturia and hypophosphatemia occur when iFGF23 levels are high, with phosphaturia mediated by iFGF23-associated reductions in expression of the sodium-dependent phosphate cotransporter 2A (NPT2A) and 2C (NPT2C) in the proximal tubule in the kidney [25, 26]. The current hypothesis regarding the mechanism underpinning the incidence of iatrogenic hypophosphatemia after administration of FCM posits that iFGF23 protein cleavage is inhibited causing high levels of iFGF23 and hypophosphatemia. While the working hypothesis implicates the FCM carbohydrate moiety in FGF23 cleavage inhibition [27], it is not known definitively why different intravenous iron formulations affect FGF23 protein processing to different extents. On the basis of the present study and the PHOSPHARE trials, SFO and FCM appear to be associated with elevated risk of hypophosphatemia relative to FDI, but further studies would be necessary to clarify the mechanism driving the different frequencies of hypophosphatemia associated with different intravenous iron preparations.
The results of the present study should be considered in the context of the patient population enrolled in the JapicCTI-194573 and Ikuta et al. RCTs, specifically Japanese women with heavy menstrual bleeding. IDA is the most common form of anemia and menorrhagia is one of the major causes; heavy menstrual bleeding imposes a variety of burdens on women’s health, impairing quality of life and, in severe cases, requiring hospitalization due to severe anemia. Without treatment with exogenous iron, common symptoms of anemia are likely to manifest, including dyspnea, fatigue, headache, cognitive dysfunction, and restless leg syndrome [28]. Hemoglobin levels lower than 70 g/L may bring about more serious symptoms such as worsening of pre-existing anginal pain, ankle edema, or dyspnea at rest [28]. Oral iron supplementation is the first-line therapy for iron restoration; however, a significant proportion of patients experience gastrointestinal side effects and some patients are refractory to oral iron preparations due to severe menorrhagia or poor drug adherence. In these cases, intravenous iron supplementation should be considered.
Finally, it is worth considering the implications of hypophosphatemia beyond the measured levels of serum phosphate. Transient, mild hypophosphatemia does not appear to cause significant clinical problems, but patients who need regular intravenous administration of iron have conditions associated with chronic blood loss such as heavy menstrual bleeding or gastrointestinal bleeding. With these conditions, repeated intravenous administration of iron may be necessary, potentially resulting in chronic hypophosphatemia. While transient hypophosphatemia may go undiagnosed—especially where serum phosphate is not being measured in routine clinical practice—chronic hypophosphatemia after administration of SFO and FCM has been reported to result in hypophosphatemic osteomalacia, which causes significant morbidity [29].
Conclusion
The MAIC conducted as part of the present study showed that FDI is associated with significantly lower rates of post-infusion hypophosphatemia than FCM in patients with IDA associated with heavy menstrual bleeding in Japan. This builds on the direct head-to-head RCT evidence from the JapicCTI-194573 RCT showing significantly lower rates of hypophosphatemia with FDI versus SFO. Clinicians should be aware that hypophosphatemia is associated with administration of certain intravenous iron formulations, and serum phosphate levels should be monitored after administration of FCM and SFO, especially in patients who receiving repeated administrations of iron.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Okada M, Imamura K, Fuchigami T, et al. Osteomalacia caused by intravenous administration saccharated ferric oxide for treatment of iron deficiency anemia associated with nonspecific multiple ulcers of the small intestine: report of two cases. Jpn J Intern Med. 1982;71:1566–72.
Okada M, Imamura K, Iida M, Omae T. Hypophosphatemia induced by intravenous administration of saccharated iron oxide. Klin Wochenshr. 1983;61:99–102.
Imamura K. Effects of intravenous administration of iron preparations on the metabolism of phosphorus. Comparative study on 3 iron preparations. Fukuoka Igaku Zasshi. 1984;75(6):316–26.
Schouten BJ, Doogue MP, Soule SG, Hunt PJ. Iron polymaltose-induced FGF23 elevation complicated by hypophosphataemic osteomalacia. Ann Clin Biochem. 2009;46(Pt 2):167–9.
Sato K, Shiraki M. Saccharated ferric oxide-induced osteomalacia in Japan: iron-induced osteopathy due to nephropathy. Endocr J. 1998;45(4):431–9.
Shimizu Y, Tada Y, Yamauchi M, et al. Hypophosphatemia induced by intravenous administration of saccharated ferric oxide: another form of FGF23-related hypophosphatemia. Bone. 2009;45(4):814–6.
Shimada T, Hasegawa H, Yamazaki Y, et al. FGF-23 is a potent regulator of vitamin D metabolism and phosphate homeostasis. J Bone Miner Res. 2004;19(3):429–35.
Schouten BJ, Hunt PJ, Livesey JH, Frampton CM, Soule SG. FGF23 elevation and hypophosphatemia after intravenous iron polymaltose: a prospective study. J Clin Endocrinol Metab. 2009;94(7):2332–7.
Wolf M, Rubin J, Achebe M, et al. Effects of iron isomaltoside vs ferric carboxymaltose on hypophosphatemia in iron-deficiency anemia: two randomized clinical trials. JAMA. 2020;323(5):432–43.
EU Clinical Trials Register. Clinical Trial Results: a randomized, double-blinded, comparative trial comparing the incidence of hypophosphatemia in relation to repeated treatment courses of iron isomaltoside and ferric carboxymaltose in subjects with iron deficiency anaemia due to inflammatory bowel disease. EudraCT number 2017-002452-87. https://www.clinicaltrialsregister.eu/ctr-search/trial/2017-002452-87/results. Accessed 21 Aug 2023.
Wolf M, Koch TA, Bregman DB. Effects of iron deficiency anemia and its treatment on fibroblast growth factor 23 and phosphate homeostasis in women. J Bone Miner Res. 2013;28:1793–803.
Vifor Pharma UK Limited. Ferinject (ferric carboxymaltose) Ireland Summary of Product Characteristics. 2023. Irish Pharmaceutical Healthcare Association, Dublin, Ireland. https://backend-prod.medicines.ie/uploads/files/648749902c1d4.pdf. Accessed 21 Aug 2023.
Vifor Pharma UK Limited. Ferinject (ferric carboxymaltose) UK Summary of Product Characteristics. 2023. Datapharm Ltd, Leatherhead, UK. https://www.medicines.org.uk/emc/product/5910/smpc. Accessed 21 Aug 2023.
Takeda Pharma Ltda. Ferinject® (carboximaltose férrica) bula para profissional da saúde. 2021. Consulta Remédios, Curitiba, Brazil. https://uploads.consultaremedios.com.br/drug_leaflet/pro/Bula-Ferinject-Profissional-Consulta-Remedios.pdf. Accessed 21 Aug 2023.
Vifor (International) Inc. Ferinject® (Eisencarboxymaltose) Fachinformationen. 2023. Refdata Foundation, Zug, Switzerland. https://www.swissmedicinfo.ch/. Accessed 21 Aug 2023.
Vifor Pharma Pty Ltd. Ferinject (ferric carboxymaltose) Australian Product Information. 2023. Therapeutic Goods Administration, Woden, Australia. https://www.ebs.tga.gov.au/ebs/picmi/picmirepository.nsf/pdf?OpenAgent&id=CP-2011-PI-02557-3. Accessed 21 Aug 2023.
American Regent, Inc. INJECTAFER® (ferric carboxymaltose injection) US prescribing information. 2020. U.S. Food and Drug Administration, Silver Spring, MD, USA. https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/203565s009lbl.pdf. Accessed 21 Aug 2023.
Kawabata H, Tamura T, Tamai S, Fujibayashi A, Sugimura M, Study Group. Intravenous ferric derisomaltose versus saccharated ferric oxide for iron deficiency anemia associated with menorrhagia: a randomized, open-label, active-controlled, noninferiority study. Int J Hematol. 2022;116:846–55.
Ikuta K, Hanashi H, Hirai K, et al. Comparison of efficacy and safety between intravenous ferric carboxymaltose and saccharated ferric oxide in Japanese patients with iron-deficiency anemia due to hypermenorrhea: a multi-center, randomized, open-label noninferiority study. Int J Hematol. 2019;109(1):41–9.
Uchida T, Kawachi Y, Watanabe A, Nishihara T, Miyake T. Reevaluation of administration dosage in parenteral iron therapy. Rinsho Ketsueki. 1996;37:123–8.
Shapiro SS, Wilk MB. An analysis of variance test for normality (complete samples). Biometrika. 1965;52(3–4):591–611.
Bucher HC, Guyatt GH, Griffith LE, Walter SD. The results of direct and indirect treatment comparisons in meta-analysis of randomized controlled trials. J Clin Epidemiol. 1997;50(6):683–91.
Edmonston D, Wolf M. FGF23 at the crossroads of phosphate, iron economy and erythropoiesis. Nat Rev Nephrol. 2020;16(1):7–19.
Eisenga MF, van Londen M, Leaf DE, et al. C-terminal fibroblast growth factor 23, iron deficiency, and mortality in renal transplant recipients. J Am Soc Nephrol. 2017;28(12):3639–46.
Wolf M, White KE. Coupling fibroblast growth factor 23 production and cleavage: iron deficiency, rickets, and kidney disease. Curr Opin Nephrol Hypertens. 2014;23(4):411–9.
Boots JMM, Quax RAM. High-dose intravenous iron with either ferric carboxymaltose or ferric derisomaltose: a benefit-risk assessment. Drug Saf. 2022;45(10):1019–36.
Kassianides X, Bhandari S. Hypophosphataemia, fibroblast growth factor 23 and third-generation intravenous iron compounds: a narrative review. Drugs Context. 2021. https://doi.org/10.7573/dic.2020-11-3
National Institute for Health and Care Excellence. Clinical Knowledge Summary: Anaemia—iron deficiency. https://cks.nice.org.uk/topics/anaemia-iron-deficiency/. Accessed 19 Oct 2022.
Vilaca T, Velmurugan N, Smith C, Abrahamsen B, Eastell R. Osteomalacia as a complication of intravenous iron infusion: a systematic review of case reports. J Bone Miner Res. 2022;37(6):1188–99.
Funding
The study, Rapid Service Fee and Open Access fees were funded by Pharmacosmos A/S.
Author information
Authors and Affiliations
Contributions
Richard F Pollock, Yutaka Osuga, Tatsunori Murata, Seiji Fukumoto conceived of the analysis. Richard F Pollock conducted the initial analyses and drafted the manuscript. Yutaka Osuga, Tatsunori Murata, and Seiji Fukumoto provided clinical and statistical input and reviewed the draft manuscript for intellectual content. Richard F Pollock incorporated changes arising from the review and prepared the final manuscript for submission.
Corresponding author
Ethics declarations
Conflict of Interest
Richard F Pollock is a director of Covalence Research Ltd, which received consultancy fees from Pharmacosmos A/S to conduct the study and write the manuscript. Seiji Fukumoto received a fee from Pharmacosmos A/S for clinical consultancy work in 2021. Tatsunori Murata and Yutaka Osuga have no conflicts of interest to disclose.
Ethical Approval
All data used in the analyses were obtained from previously-conducted studies and the analyses are not reliant on data from studies of human or animal participants conducted by any of the authors. Both the JapicCTI-194573 and Ikuta et al. 2019 RCTs, on which the present analysis is based, were approved by the institutional review boards (IRBs) at each participating site. Written informed consent for participation in the studies was obtained from all subjects and both studies were conducted in accordance with the Declaration of Helsinki and Good Clinical Practice (GCP) guidelines.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Fukumoto, S., Murata, T., Osuga, Y. et al. Incidence of Hypophosphatemia After Intravenous Administration of Iron: A Matching-Adjusted Indirect Comparison of Data from Japanese Randomized Controlled Trials. Adv Ther 40, 4877–4888 (2023). https://doi.org/10.1007/s12325-023-02591-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-023-02591-1