Abstract
Introduction
To evaluate factors associated with severe coronavirus disease 2019 (COVID-19) among patients with rheumatoid arthritis (RA) in the US.
Methods
Adults with RA who had a severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection, based on molecular or antigen test or clinical diagnosis, were identified from the Optum® COVID-19 Electronic Health Record dataset (March 1, 2020–April 28, 2021). The primary outcome was the occurrence of severe COVID-19 (hospitalization or death) within 30 days from SARS-CoV-2 infection. Adjusted odds ratios (aOR) and 95% confidence intervals (CI) were estimated using multivariable logistic regression models to assess the association between severe COVID-19 and patient characteristics, including demographics, baseline comorbidities, and recent RA treatments.
Results
During the study period, 6769 SARS-CoV-2 infections were identified in patients with RA, among whom 1460 (22%) developed severe COVID-19. Multivariable logistic regression analysis showed that being older, male, and non-White and having diabetes and cardiovascular conditions are associated with greater odds of severe COVID-19. In addition, compared with no use, the adjusted odds of severe COVID-19 were lower with recent use of tumor necrosis factor inhibitors (aOR 0.60, 95% CI 0.41–0.86) and higher with recent use of corticosteroids (aOR 1.38, 95% CI 1.13–1.69) or rituximab (aOR 2.87, 95% CI 1.60–5.14), respectively.
Conclusion
Nearly one in five patients with RA developed severe COVID-19 disease within 30 days after SARS-CoV-2 infection. In patients with RA, recent use of corticosteroids and rituximab were two factors associated with a greater risk of severe COVID-19 in addition to the risk factors among demographics and comorbidities previously identified in the general population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Rheumatoid arthritis (RA) studies evaluating the association between severe coronavirus disease 2019 (COVID-19) outcomes and patient characteristics have been limited because of their use of broader, heterogeneous groups, such as rheumatic diseases, and study registries or institution-based cohorts, which come with unmeasurable sampling bias. |
To confirm previous findings, this study used a large, US-based electronic health record database to evaluate the association between severe COVID-19 and patient characteristics in RA. |
What was learned from this study? |
This study found that older age, certain comorbidities, and recent use of corticosteroids and rituximab are strong risk factors for severe COVID-19 in patients with RA; recent tumor necrosis factor inhibitor use was associated with lower risk for severe COVID-19 in patients with RA. |
Patients with RA, particularly those with certain characteristics, including age, comorbidities, and treatments, are more susceptible to developing severe COVID-19. Consequently, individualized risk assessment and minimization, such as vaccinations, and increased monitoring of those patients who develop COVID-19, should be encouraged. |
Introduction
The ongoing coronavirus disease 2019 (COVID-19) pandemic has resulted in over 668 million cases and 6.7 million deaths worldwide as of January 2023 [1]. Those in the general population who are particularly susceptible to severe illness from COVID-19 are elderly individuals and those who have certain comorbid conditions, such as cardiovascular diseases and diabetes. Likewise, those with compromised immune systems, such as patients with cancer and recipients of immunosuppressive therapies for solid organ transplants, and immune-mediated inflammatory diseases (IMIDs), such as rheumatoid arthritis (RA), are also at high risk for severe illness from COVID-19 [2,3,4].
Several studies have examined the association between severe COVID-19 outcomes and demographics, clinical characteristics, and anti-inflammatory treatments in patients with rheumatic diseases or the broader group of IMIDs using disease registries or institutional-based cohorts [5,6,7,8,9]. Limitations of grouping patients of highly heterogeneous conditions, disease severities, and immunomodulating therapy use were well acknowledged by the authors, who also called for further understanding of factors driving adverse outcomes. One recent study using the COVID-19 Global Rheumatology Alliance physician registry assessed the relative risk for severe COVID-19 in RA between tumor necrosis factor (TNF) inhibitors and other RA treatments [10]. In this global convenience sample of 2869 patients, the use of rituximab and Janus kinase (JAK) inhibitor was associated with worse COVID-19 severity compared with TNF inhibitors [10]. However, it is difficult to generalize these findings outside the study registries or institution-based cohorts as these convenience samples come with unmeasurable sampling bias. Therefore, findings from registry-based studies should be further validated in population-based studies before extrapolating the findings to broader populations. Although global registries can achieve meaningful large sample sizes in a shorter period of time, the study subjects were also enrolled from heterogenous healthcare systems with substantial differences in access to medicine, disease status, understanding of COVID-19, local public health strategy and policy, and other intangible factors that can have effects on COVID-19 outcomes. Consequently, there is a need for using population-based data sourced from routine medical practice to mitigate sampling bias and to improve precision with larger sample size. In this retrospective cohort study, a large, national electronic health record (EHR) database from routine clinical care in the USA was utilized to evaluate the association between severe COVID-19 and patient characteristics, including demographics, baseline comorbidities, and recent RA treatments.
Methods
Study Design and Data Sources
This retrospective cohort study was conducted using the Optum® de-identified COVID-19 EHR dataset, utilizing data from an integrated network of ambulatory and hospital care providers for the period from March 1, 2020 to April 28, 2021. The database contains administrative and clinical information for 4.7 million unique patients as recorded during routine clinical practice from a large network of providers and hospitals across all 50 states in the US, including medical records, laboratory results, prescription orders, and administrative data [11,12,13]. Additionally, this database contains longitudinal care data for patients with COVID-19-related encounters, including receiving a test, qualitative results of testing, and diagnoses for COVID-19.
Compliance with Ethics Guidelines
Through a paid contract with Optum®, authors were granted permission to use and provided access to the database. The authors affirm that this retrospective database analysis did not collect, use, or transmit patient-identifiable data. Based on US Department of Health and Human Services code 45CFR46.104(d)(4) (Existing Data and Specimens—No Identifiers), this study is exempt from the requirement for institutional review board approval. The study is compliant with data security requirements of the Health Insurance Portability and Accountability Act of 1996 [14].
Study Population
Patients aged ≥ 18 years were included in the study. The index date was the date of the earliest positive test for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection that was confirmed with molecular polymerase chain reaction (PCR) or antigen test or the date of diagnosis of COVID-19 (International Classification of Diseases [ICD]-10 diagnosis code: U07.1 or U07.2). Patients were also required to have at least one diagnosis for RA (ICD-9: 714; ICD-10: M05 or M06) during the 15-month baseline period prior to the index date and remain active through the baseline period (Supplementary Material Fig. 1). Patients were excluded if their age or sex was missing. A sensitivity analysis was conducted in patients with actively treated RA defined as having at least one diagnosis of RA and being treated with any of the conventional synthetic disease-modifying antirheumatic drugs (csDMARDs), biologic disease-modifying antirheumatic drugs (bDMARDs), or JAK inhibitors at any time prior to the index date.
All database records were de-identified and compliant with US patient confidentiality requirements, including the Health Insurance Portability and Accountability Act of 1996 [14]. No institutional review board approval was required.
Study Variables
Patient characteristics, including demographics (age, sex, US geographic region, race and ethnicity, month and year of SARS-CoV-2 infection, smoking status, body mass index [BMI], and type of insurance) and comorbid conditions (cardiovascular diseases, chronic kidney diseases, chronic liver diseases, chronic lung diseases, diabetes mellitus, systemic inflammatory disease, and immunocompromised state) were assessed during the 15-month baseline period prior to index date. Further, Charlson Comorbidity Index (CCI) was calculated for a quantitative evaluation of the overall disease burden (Table 1, Supplementary Material Table S1). Based on written prescriptions and administration records, recent exposure to the following RA medications at the time of SARS-CoV-2 infection was determined using various time frames to account for variability in pharmacology and dosing schedule: bDMARDs were identified within 6 months before the index date because of their prolonged effect; orally administered csDMARDs and JAK inhibitors were identified within the 3 months before the index date; the administration of intravenous (IV) or oral systemic corticosteroids was identified within 30 days before the index date (Table 1, Supplementary Material Fig. 1).
Outcomes
The primary outcome was the occurrence of severe COVID-19, defined as either hospitalization or death, within 30 days from the index date. Secondary outcomes were all-cause hospitalization and all-cause death within 30 days from index date, examined separately.
Statistical Analyses
Patient demographics and clinical characteristics and recent RA treatment of the study population were summarized with descriptive statistics. Mean and standard deviation (SD) for continuous variables and count (N) and proportion (%) for categorical variables were reported for descriptive statistics. Standardized mean differences were used to evaluate the differences in baseline variables between RA patients with and without severe COVID-19.
Multivariable logistic regression was performed to examine the association between patient characteristics, individual comorbidities, and recent RA treatments, and the primary and the secondary outcomes, separately. Adjusted odds ratios (aOR) with 95% confidence intervals (95% CI) were reported for each demographic, clinical characteristic, and recent RA treatment variable included in the final model. For the sensitivity analysis, similar multivariable logistic regression was conducted for all primary and secondary outcomes in a subgroup of patients with actively treated RA as described above. All analyses were conducted using SAS Studio 3.81 (SAS Institute Inc., Cary, NC, USA).
Results
Study Population
A total of 6769 SARS-CoV-2 infections were identified in patients with RA over the period of March 1, 2020, through April 28, 2021 (Fig. 1). Of the 6769 patients, 22% (n = 1460) developed severe COVID-19 within 30 days after SARS-CoV-2 infection, including 1399 hospitalizations (among which 137 [9.8%] deaths occurred) and 61 deaths outside the hospital. The majority (64%) of the SARS-CoV-2 infections were confirmed with laboratory tests (4162 with positive PCR and an additional 190 with positive antigen test), while the remaining ones (36%) identified solely based on recorded clinical diagnosis (Supplementary Material Fig. 2). The average age of the study cohort was 61 (SD: 14.9) years, with 77% female and 70% non-Hispanic White individuals (Table 1). Patients who developed severe COVID-19 outcomes tended to be older (mean age 68.3 vs. 59.1 years), be male (29% vs. 21%), and have more comorbidities compared with those who did not develop severe COVID-19 (Supplementary Material Table S1).
Factors Associated with Severe COVID-19
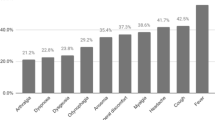
The multivariable analysis controlling for all covariates listed in Table 2 confirmed the association between several demographic factors and comorbidities previously observed in the general populations and in those with other rheumatic diseases and severe COVID-19 in patients with RA. Among demographic variables, aged ≥ 65 years versus aged < 65 years had the strongest association with severe COVID-19 (aOR 2.32, 95% CI 2.01–2.68). Moderate association with severe COVID-19 was observed for the early phase of the COVID-19 pandemic from March to September 2020 versus the subsequent time from October 2020 to March 2021 (aOR 1.80, 95% CI 1.58–2.06), racial and ethnic minority versus non-Hispanic White (aOR 1.50, 95% CI 1.30–1.72), Southern US census region versus other regions (aOR 1.45, 95% CI 1.24–1.69), male sex (aOR 1.31, 95% CI 1.13–1.51), and current or former smoker versus never smoked (aOR 1.22, 95% CI 1.07–1.39). With every five units of increment in BMI, odds of developing severe COVID-19 were 4% higher, but the association failed to reach statistical significance (aOR 1.04, 95% CI 0.99–1.09) (Table 2, Fig. 2). The same multivariable model also observed moderate association between severe COVID-19 and the following comorbidities: pulmonary hypertension (aOR 1.52, 95% CI 1.17–1.96), heart failure (aOR 1.51, 95% CI 1.26–1.81), hypertension (aOR 1.47, 95% CI 1.26–1.71), diabetes (aOR 1.44, 95 CI 1.25–1.66), chronic kidney disease (aOR 1.38, 95% CI 1.16–1.64), immunocompromised state (aOR 1.29, 95% CI 1.08–1.54), and chronic lung disease (aOR 1.17, 95% CI 1.02–1.33). The same model also found that the recent use of rituximab (aOR 2.87, 95% CI 1.60–5.14) and systemic corticosteroid (aOR 1.38, 95% CI 1.13–1.69) at the time of SARS-CoV-2 infection were positively associated with severe COVID-19, while the recent use of TNF inhibitor biologics (aOR 0.60, 95% CI 0.41–0.86) was negatively associated with the outcome. No significant association was seen between recent use of JAK inhibitors (aOR 1.17, 95% CI 0.65–2.10) and non-TNF bDMARDs excluding rituximab (aOR 0.77, 95% CI 0.43–1.40).
Factors associated with primary and secondary COVID-19 outcomes in patients with RA. Multivariable analyses of study outcomes within 30 days of SARS-CoV-2 infection among patients with RA and COVID-19 for: A severe COVID-19, defined as hospitalization or death, B hospitalizations, and C death. aOR adjusted odds ratio, bDMARD biologic DMARD, BMI body mass index, CI confidence interval, COVID-19 coronavirus disease 2019, DMARD disease-modifying anti-rheumatic drugs, IV intravenous, JAKi Janus kinase inhibitor, RA rheumatoid arthritis, ref reference, TNFi tumor necrosis factor inhibitor
Factors Associated with COVID-19-Related Hospitalization and Death
Separate multivariable analyses were conducted for COVID-19-related hospitalization and death within 30 days of SARS-CoV-2 infection, with both models controlling for all covariates listed in Table 2 and Fig. 2. Factors associated with hospitalization within 30 days of SARS-CoV-2 infection were similar to those associated with the primary outcome, with the exception of a statistically significant effect for every five units of increment in BMI (aOR 1.05, 95% CI 1.01–1.10).
After controlling for covariates listed in Table 2 and Fig. 2, the strongest association between death within 30 days after SARS-CoV-2 infection was observed for patients aged ≥ 65 years versus aged < 65 years (aOR 5.89, 95% CI 3.72–9.32), while male sex (aOR 1.10, 95% CI 0.79–1.54), racial and ethnic minority versus non-Hispanic White (aOR 1.03, 95% CI 0.72–1.48), and the early phase of the COVID-19 pandemic from March to September 2020 versus October 2020 to April 2021 (aOR 1.05, 95% CI 0.76–1.45) were not associated with death. Heart failure (aOR 2.32, 95% CI 1.63–3.31) was strongly associated with death in the same multivariable model, while modest and not statistically significant associations were observed for other comorbidities: hypertension (aOR 1.24, 95% CI 0.82–1.87), diabetes (aOR 1.34, 95 CI 0.96–1.88), chronic kidney disease (aOR 1.32, 95% CI 0.93–1.87), and immunocompromised state (aOR 1.29, 95% CI 0.89–1.86). Like severe COVID-19 and COVID-19-related hospitalization, COVID-19-related death was also positively associated with use of rituximab (aOR 2.14, 95% CI 0.62–7.40) and systemic corticosteroid (aOR 1.47, 95% CI 0.95–2.26), although the associations were not significant likely because of the small number of deaths captured in the database. Neither use of JAK inhibitors (aOR 0.85, 95% CI 0.11–6.36) nor non-TNF bDMARDs excluding rituximab (aOR 1.12, 95% CI 0.27–4.74) was associated with COVID-19-related death within 30 days.
Sensitivity Analysis in Patients with Actively Treated RA
The sensitivity analyses carried out in 5441 COVID-19 patients (Supplementary Material Table S2) with actively treated RA during the same study period reported consistent findings with the primary analyses (Table 3). In each separately created multivariable model, similar aORs were reported for the association between COVID-19 outcomes and the demographic, comorbid, and RA medication variables (Table 3).
Discussion
In this large, real-world cohort study, we identified 6769 patients with RA who contracted COVID-19 between March 2020 and April 2021 (a time period before the emergence of the Delta variant), among whom 22% developed severe COVID-19 (either hospitalization or death) within 30 days from SARS-CoV-2 infection. We confirmed previous reports for the general population and those with various rheumatic diseases that older age, male sex, racial and ethnic minority, history of smoking, higher BMI, being immunocompromised, and presence of comorbidities including diabetes, hypertension, pulmonary hypertension, heart failure, chronic lung disease, and chronic kidney disease were associated with severe COVID-19 [5, 7, 15,16,17]. Being in the Southern US census region and contracting COVID-19 during the early phase of the pandemic were also associated with poor COVID-19 outcomes. In addition, patients had greater odds of developing severe COVID-19 if they recently received systemic corticosteroids or rituximab at the time of SARS-CoV-2 infection, while those who had recently used TNF inhibitors were less likely to develop severe COVID-19. Recent use of other RA treatments, including JAK inhibitors and non-TNF bDMARDs excluding rituximab, had no association with severe COVID-19.
Our analyses for secondary outcomes examined COVID-19-related hospitalizations and deaths separately. We found that study variables contributed similarly to hospitalization compared to the primary outcome of severe COVID-19. However, a few study variables contributed to COVID-19-related death differently than severe COVID-19. Noticeably, aged ≥ 65 years was strongly associated with COVID-19-related death, increasing the odds by 489%. In contrast, the variable doubled the odds for severe COVID-19 and COVID-19-related hospitalization, showing a moderate effect.
Our findings agreed with previous studies that examined factors associated with COVID-19 outcomes in smaller samples of patients with rheumatic diseases and RA and found corticosteroid use was associated with COVID-19-related hospitalization [7, 18]. We also observed an even greater, but not statistically significant, increase in deaths (aOR 1.47, 95% CI 0.95–2.26) where lack of significance was likely the result of the sample size (n = 198 for COVID-19-related deaths in this study). A previous report from the COVID-19 Global Rheumatology Alliance physician registry of 2869 patients with RA assessed the relative effect between RA treatments and found rituximab users and JAK inhibitor users were more likely to develop severe COVID-19 outcomes than those using TNF inhibitors [10]. The US-based TriNetX study also observed an elevated risk of hospitalization for rituximab over TNF inhibitors, but JAK inhibitors showed no difference with TNF inhibitors in this study [19]. Our findings, using “no use” as reference for each RA treatment, were in line with the published literature on rituximab, which also suggests that rituximab use increases odds of severe COVID-19 outcomes. Although the association was not statistically significant in the analyses for COVID-19 death, this will also need to be confirmed by future studies that include larger sample sizes.
The different findings for JAK inhibitors between published literature and our analysis may be related to the heterogeneity of the various data sources, residual confounding, and the use of different references. We found that recent TNF inhibitor use was associated with reduced odds of developing severe COVID-19 outcomes when adjusting for demographics, comorbidities, and other RA treatments, similar to previous findings among patients with rheumatic diseases or IMIDs for COVID-19-related hospitalizations [7, 8]. The protective effect of TNF inhibitor use over severe COVID-19 may mask the true effect other RA treatments have over COVID-19 outcomes compared to TNF inhibitors with residual confounding present [8, 10, 19, 20]. We found no association between the recent use of other non-TNF bDMARDs, excluding rituximab, and increased odds of developing severe COVID-19 outcomes.
Several studies reported differential COVID-19 outcomes by demographic and socioeconomic status in the general population [21]. Large retrospective studies and systematic reviews showed higher risks of COVID-19 severity in racial and ethnic minorities [22,23,24]. In our RA population, we found that racial and ethnic minorities were associated with developing severe COVID-19 outcomes, but not death specifically, after adjusting for potential risk factors such as age, sex, comorbidities, and recent RA treatments. Regional variation in health and mortality has been shown among the US general population and reported for COVID-19 outcomes [21, 25,26,27]. Inspired by these findings, we investigated the regional differences in COVID-19 outcomes and found that patients with RA in the Southern region of the US were more likely to develop severe COVID-19 as well as COVID-19-related hospitalization and death. Temporal trends in COVID-19 outcomes remain an important parameter to understand for future preparedness. A previous study found patients with various rheumatic diseases had higher risk of severe COVID-19 during the first 90 days of the pandemic than the subsequent 90 days [6]. We also found a similar temporal trend for severe COVID-19 and COVID-19-related hospitalization in patients with RA between the first 7 months (March to September 2020) and subsequent 6 months (October 2020 to April 2021); however, such improvement over time was not observed for COVID-19 deaths. Although our study had limited information on other factors that may also have contributed to the outcomes, such as RA severity, social behaviors, and vaccination status, the characteristics we identified provided crucial information to inform COVID-19 management in patients with RA.
The strength of this current study is that it utilized a large US EHR dataset containing relevant clinical information from a large network of providers and hospitals and longitudinal care data for patients with COVID-19-related encounters. Another strength of the data source is that it is based on routine medical practice across all care, COVID-19 and non-COVID-19 related.
There are several limitations to this study. Despite adjusting for a series of covariates in the multivariable model, residual confounding may still be present, such as social behaviors, vaccination status, and, most importantly, RA severity. To minimize the potential residual confounding by RA disease severity, we have controlled for various lines of RA treatment as a proxy for disease severity [28]. COVID-19 vaccines were not broadly available to the general US population during the study period so vaccination data were not available, though various COVID-19 vaccines have since become available. Potentially, the introduction of vaccines towards the latter portion of the study period may have contributed to the observed severity decline. As the world continues to face disparities in global vaccination progress and surges of new variants of COVID-19, our study findings in a largely unvaccinated population can still contribute to COVID-19 care. Exposure to RA treatments was determined from records of both medication administration and written prescription. While written prescriptions capture the intended treatment, we have no proof that patients adhered to their treatment plan. Thus, this study assumed that patients filled and adhered to their prescribed medication. However, one previous study using the Optum EHR data among patients with inflammatory bowel disease found high agreement between EHR and claims data for infused biologics that could provide some clarity on accuracy of immuno-mediating therapies for IMIDs [29]. Despite the use of various half-life-based windows to measure exposure to various RA treatments, misclassification still can occur using recent therapy recorded in the EHR to reflect actual exposure to the DMARDs at time of COVID-19 onset.
Conclusions
This large, nationwide, population-based cohort study including 6769 SARS-CoV-2 infections among patients with RA found that in the RA population, similar to the general population, older age, male sex, racial and ethnic minority, higher BMI, and having diabetes, cardiovascular diseases, chronic kidney, and lung disease were associated with severe COVID-19 for patients with RA. We assessed the relationship between recent use of various RA treatments and severe COVID-19 outcomes and found that recent rituximab use and systemic corticosteroid use were both associated with significant increased odds of developing severe COVID-19. Recent TNF inhibitor use was associated with reduced odds of severe COVID-19, and recent use of JAK inhibitors and non-TNF bDMARDs excluding rituximab was not associated with severe COVID-19 in the RA population. The findings suggest that risk for severe COVID-19 outcomes should be individually assessed for patients with RA, particularly those with one or more risk factors.
References
Johns Hopkins University of Medicine Coronavirus Resource Center. Mortality analyses; 2021. https://coronavirus.jhu.edu/map.html.
Centers for Disease Control and Prevention. CDC updates, expands list of people at risk of severe COVID-19 illness; 2020. https://www.cdc.gov/media/releases/2020/p0625-update-expands-covid-19.html.
Williamson EJ, Walker AJ, Bhaskaran K, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020;584(7821):430–6.
Gold JAW, Wong KK, Szablewski CM, et al. Characteristics and clinical outcomes of adult patients hospitalized with COVID-19—Georgia, March 2020. MMWR Morb Mortal Wkly Rep. 2020;69(18):545–50.
Hyrich KL, Machado PM. Rheumatic disease and COVID-19: epidemiology and outcomes. Nat Rev Rheumatol. 2021;17(2):71–2.
Jorge A, D’Silva KM, Cohen A, et al. Temporal trends in severe COVID-19 outcomes in patients with rheumatic disease: a cohort study. Lancet Rheumatol. 2021;3(2):e131–7.
Gianfrancesco M, Hyrich KL, Al-Adely S, et al. Characteristics associated with hospitalisation for COVID-19 in people with rheumatic disease: data from the COVID-19 Global Rheumatology Alliance physician-reported registry. Ann Rheum Dis. 2020;79(7):859–66.
Izadi Z, Brenner EJ, Mahil SK, et al. Association between tumor necrosis factor inhibitors and the risk of hospitalization or death among patients with immune-mediated inflammatory disease and COVID-19. JAMA Netw Open. 2021;4(10): e2129639.
Strangfeld A, Schafer M, Gianfrancesco MA, et al. Factors associated with COVID-19-related death in people with rheumatic diseases: results from the COVID-19 Global Rheumatology Alliance physician-reported registry. Ann Rheum Dis. 2021;80(7):930–42.
Sparks JA, Wallace ZS, Seet AM, et al. Associations of baseline use of biologic or targeted synthetic DMARDs with COVID-19 severity in rheumatoid arthritis: results from the COVID-19 Global Rheumatology Alliance physician registry. Ann Rheum Dis. 2021;80(9):1137–46.
Optum, Inc. Optum COVID-19 data quality services; 2020. https://www.optum.com/content/dam/optum3/optum/en/resources/brochures/optum-covid-data-quality-vac-mgmt-brochure.pdf.
Optum, Inc. Ignite insights with Optum EHR data; 2020. https://www.optum.com/content/dam/optum3/optum/en/resources/sell-sheet/ehr-data-sell-sheet.pdf.
Optum, Inc. Optum EHR data; 2021. https://www.optum.com/business/solutions/life-sciences/real-world-data/ehr-data.html.
Optum, Inc. Clinformatics® data mart; 2017. https://www.optum.com/content/dam/optum3/optum/en/resources/white-papers/clinformatics-data-mart.pdf.
Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–62.
Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239–42.
Peckham H, de Gruijter NM, Raine C, et al. Male sex identified by global COVID-19 meta-analysis as a risk factor for death and ITU admission. Nat Commun. 2020;11(1):6317.
Mahdavi AM, Varshochi M, Hajialilo M, Dastgiri R, Khabbazi A. Factors associated with COVID-19 and its outcome in patients with rheumatoid arthritis. Clin Rheumatol. 2021;40:4527–31.
Raiker R, DeYoung C, Pakhchanian H, et al. Outcomes of COVID-19 in patients with rheumatoid arthritis: a multicenter research network study in the United States. Semin Arthritis Rheum. 2021;51(5):1057–66.
Liang W, Zhao Y, Lee AH. An investigation of the significance of residual confounding effect. Biomed Res Int. 2014;2014: 658056.
Ahmad K, Erqou S, Shah N, et al. Association of poor housing conditions with COVID-19 incidence and mortality across US counties. PLoS One. 2020;15(11): e0241327.
Magesh S, John D, Li WT, et al. Disparities in COVID-19 outcomes by race, ethnicity, and socioeconomic status: a systematic-review and meta-analysis. JAMA Netw Open. 2021;4(11): e2134147.
Azar KMJ, Shen Z, Romanelli RJ, et al. Disparities In outcomes among COVID-19 patients in a large health care system in California. Health Aff (Millwood). 2020;39(7):1253–62.
Velasco F, Yang DM, Zhang M, et al. Association of healthcare access with intensive care unit utilization and mortality in patients of hispanic ethnicity hospitalized with COVID-19. J Hosp Med. 2021;16(11):659–66.
Zang E, West J, Kim N, Pao C. US regional differences in physical distancing: evaluating racial and socioeconomic divides during the COVID-19 pandemic. PLoS One. 2021;16(11): e0259665.
Dobis EA, Stephens HM, Skidmore M, Goetz SJ. Explaining the spatial variation in American life expectancy. Soc Sci Med. 2020;246: 112759.
Vierboom YC, Preston SH, Hendi AS. Rising geographic inequality in mortality in the United States. SSM Popul Health. 2019;9: 100478.
Sarri G, Bennett D, Debray T, et al. ISPE-endorsed guidance in using electronic health records for comparative effectiveness research in COVID-19: opportunities and trade-offs. Clin Pharmacol Ther. 2022;112:990–9.
Huisingh C, Wegrzyn L. Agreement between electronic health record and medical claims data for defining exposure to infused biologic treatments in inflammatory bowel disease. Pharmacoepidemiol Drug Saf. 2020;29:27–8.
Acknowledgements
Funding
Financial support for the study and its publication, including the journal’s Rapid Service Fee, was provided by AbbVie. AbbVie sponsored the study; contributed to the design; participated in the collection, analysis, and interpretation of data; and in writing, reviewing, and approving the final version. No honoraria or payments were made for authorship.
Medical Writing, Editorial, and Other Assistance
Medical writing assistance was provided by Alan Saltzman, PhD, CMPP, of Fishawack Facilitate Ltd., part of Fishawack Health, and was funded by AbbVie Inc., North Chicago, IL.
Author Contributions
All authors were involved in drafting the article or revising it critically for important intellectual content, and all authors approved the final version to be published. Dr. Ye had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Study conception and design: Yizhou Ye, Xiaomeng Yue, Whitney S. Krueger, Lani R. Wegrzyn, Anna W. Maniccia, Kevin L. Winthrop, and Seoyoung C. Kim. Acquisition of data: Yizhou Ye, Xiaomeng Yue, Whitney S. Krueger, and Lani R. Wegrzyn. Analysis and interpretation of data: Yizhou Ye, Xiaomeng Yue, Whitney S. Krueger, Lani R. Wegrzyn, Anna W. Maniccia, Kevin L. Winthrop, and Seoyoung C. Kim.
Disclosures
Yizhou Ye, Xiaomeng Yue, Whitney S. Krueger, Lani R. Wegrzyn, and Anna W. Maniccia are AbbVie employees and may own AbbVie stock or options. Kevin L. Winthrop has received consulting fees and research grants from AbbVie, Bristol-Myers Squibb, Eli Lilly, Galapagos, Gilead, Novartis, Pfizer, Regeneron, Roche, Sanofi, and UCB. Seoyoung C. Kim has received research grants to the Brigham and Women’s Hospital from Pfizer, AbbVie, Roche, and Bristol-Myers Squibb for unrelated studies.
Compliance with Ethics Guidelines
Through a paid contract with Optum, authors were granted permission to use and provided access to the database. The authors affirm that this retrospective database analysis did not collect, use, or transmit patient-identifiable data. Based on US Department of Health and Human Services code 45CFR46.104(d)(4) (Existing Data and Specimens—No Identifiers), this study is exempt from the requirement for institutional review board approval. The study is compliant with data security requirements of the Health Insurance Portability and Accountability Act of 1996 [14].
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Ye, Y., Yue, X., Krueger, W.S. et al. Factors Associated with Severe COVID-19 Among Patients with Rheumatoid Arthritis: A Large, Nationwide Electronic Health Record Cohort Study in the United States. Adv Ther 40, 3723–3738 (2023). https://doi.org/10.1007/s12325-023-02533-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-023-02533-x