Abstract
Introduction
Research related to the result of patients with mild traumatic brain injury and the role of percutaneous oxygen saturation (SpO2) level is rarely reported. Our study investigated the relationship between SpO2 and the 30- and 90-day mortality among patients with mild TBI.
Methods
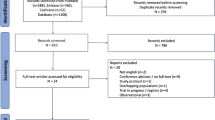
A total of 1027 patients with mild TBI [Glasgow Coma Scale (GCS) > 12] were enrolled from the Medical Information Mart for Intensive Care (MIMIC-III) database. The patients were classified into low-SpO2 (< 95%), moderate-SpO2 (95–98%), and high-SpO2 groups (> 98%). With 30- and 90-day mortality rates as the main outcomes, Cox regression and confined cubic spline models were adopted.
Results
There was a U-shaped curve in confined cubic splines for the relationship between SpO2 and mortality. Compared with the moderate-SpO2 group, the high-SpO2 group exhibited a much higher risk of mortality after modification, with hazard proportions of 2.108 (95% CI 1.211–3.670, P < 0.05) for the 30-day mortality and 1.760 (95% CI 1.140–2.720, P < 0.05) for the 90-day mortality, and the low-SpO2 group exhibited a much higher risk of mortality after modification, with hazard proportions of 2.215 (95% CI 1.194–4.110, P < 0.05) for the 90-day mortality.
Conclusion
Among patients with mild TBI, the correlation between SpO2 level and 30- and 90-day mortality followed a U-shaped curve. Both low and high SpO2 level exerted potential harmful effects on the outcomes of patients with mild TBI. The SpO2 range of 95–98% could be the optimal SpO2 level for mild patients with TBI.





Similar content being viewed by others
References
Brenner M, Stein D, Hu P, Kufera J, Wooford M, Scalea T. Association between early hyperoxia and worse outcomes after traumatic brain injury. Arch Surg. 2012;147:1042–6.
Carney N, Totten A, O’Reilly C, et al. Guidelines for the management of severe traumatic brain injury, fourth edition. Neurosurgery. 2017;80:6–15.
Cole T. Global road safety crisis remedy sought: 1.2 million killed, 50 million injured annually. JAMA. 2004;291:2531–2.
Davis DP, Meade W, Sise MJ, et al. Both hypoxemia and extreme hyperoxemia may be detrimental in patients with severe traumatic brain injury. J Neurotrauma. 2009;26:2217–23.
Ghajar J. Traumatic brain injury. Lancet. 2000;356:923–9.
Girardis M, Busani S, Damiani E, et al. Effect of conservative vs conventional oxygen therapy on mortality among patients in an intensive care unit: the oxygen-ICU randomized clinical trial. JAMA. 2016;316:1583–9.
Jubran A. Pulse oximetry. Crit Care. 2015;19:272.
Kallet RH, Branson RD. Should oxygen therapy be tightly regulated to minimize hyperoxia in critically ill patients? Respir Care. 2016;61:801–15.
Maas AIR, Stocchetti N, Bullock R. Moderate and severe traumatic brain injury in adults. Lancet Neurol. 2008;7:728–41.
Manning EP. Central nervous system oxygen toxicity and hyperbaric oxygen seizures. Aerosp Med Hum Perform. 2016;87:477–86.
Martin J, Mazer-Amirshahi M, Pourmand A. The impact of hyperoxia in the critically ill patient: a review of the literature. Respir Care. 2020;65:1202–10.
McHugh GS, Engel DC, Butcher I, et al. Prognostic value of secondary insults in traumatic brain injury: results from the IMPACT study. J Neurotrauma. 2007;24:287–93.
Miller JD, Sweet RC, Narayan R, Becker DP. Early insults to the injured brain. JAMA. 1978;240:439–42.
O’Driscoll BR, Howard LS, Davison AG, British Thoracic S. BTS guideline for emergency oxygen use in adult patients. Thorax. 2008;63(Suppl 6):vi1–68.
Pan P, Su L, Zhang Q, Long Y, Wang X, Liu D. Effects of quality control targets (SpO2 not equal100%, PaCO2/<40 mmHg, Pmean/>10 cmH2O) on outcomes in patients in the ICU. Front Med (Lausanne). 2020;7:111.
Hawryluk G, Rubiano A, Totten A, et al. Guidelines for the management of severe traumatic brain injury: 2020 update of the decompressive craniectomy recommendations. Neurosurgery. 2020;87:427–34.
O’Driscoll BR, Howard LS, Earis J, Mak V. BTS guideline for oxygen use in adults in healthcare and emergency settings. Thorax. 2017;72:ii1–90.
Siemieniuk RAC, Chu DK, Kim LH, et al. Oxygen therapy for acutely ill medical patients: a clinical practice guideline. BMJ. 2018;363:k4169.
Yang J, Li Y, Liu Q, et al. Brief introduction of medical database and data mining technology in big data era. J Evid Based Med. 2020;13:57–69.
Yu Y, Wang J, Wang Q, et al. Admission oxygen saturation and all-cause in-hospital mortality in acute myocardial infarction patients: data from the MIMIC-III database. Ann Transl Med. 2020;8(21):1371.
Sjoberg F, Singer M. The medical use of oxygen: a time for critical reappraisal. J Intern Med. 2013;274:505–28.
Solberg R, Longini M, Proietti F, Vezzosi P, Saugstad OD, Buonocore G. Resuscitation with supplementary oxygen induces oxidative injury in the cerebral cortex. Free Radical Biol Med. 2012;53:1061–7.
Thomson L, Paton J. Oxygen toxicity. Paediatr Respir Rev. 2014;15:120–3.
Vincent J-L, Taccone FS, He X. Harmful effects of hyperoxia in postcardiac arrest, sepsis, traumatic brain injury, or stroke: the importance of individualized oxygen therapy in critically ill patients. Can Respir J. 2017;2017:2834956. https://doi.org/10.1155/2017/2834956.
Rincon F, Kang J, Vibbert M, Urtecho J, Athar MK, Jallo J. Significance of arterial hyperoxia and relationship with case fatality in traumatic brain injury: a multicentre cohort study. J Neurol Neurosurg Psychiatry. 2014;85:799–805.
Gennarelli T, Champion H, Sacco W, Copes W, Alves W. Mortality of patients with head injury and extracranial injury treated in trauma centers. J Trauma. 1989;29:1193–201 (discussion 1201–1192).
Acknowledgements
Funding
The Natural Science Foundation of Guangdong Province, China (Grant number 2020A1515011249) and the Fundamental Research Funds for the Central Universities of China (Grant number: 21620406) supported this research. The study and the journal’s Rapid Service Fee were funded by Angke Biotechnology Co., Ltd.
Author Contributions
Conception and design: Wei Sun, Yusheng Zhang, Jun Lyu. Acquisition of data: Wei Sun, Ling Wang, Shiqi Yuan, Pingping Song, Rongrong Liu. Statistical analysis: Wei Sun, Shiqi Yuan. Interpretation of data: Wei Sun, Ling Wang, Shiqi Yuan, Wenqiang Che. Drafting the article: Wei Sun. Critically revising the article: Yusheng Zhang, Jiamin Xu. Reviewed and approved the submitted version of manuscript: all authors.
Disclosures
Wei Sun, Yusheng Zhang, Jun Lyu. Ling Wang, Shiqi Yuan, Pingping Song, Rongrong Liu, Wenqiang Che, and Jiamin Xu have nothing to disclose.
Compliance with Ethics Guidelines
This article is based on the MIMIC-III database and does not contain any new studies with human participants or animals performed by any of the authors. Ethical approval and the demand for informed consent were waived for our research. The Massachusetts Institute of Technology (Cambridge, MA) and Beth Israel Deaconess Medical Center (Boston, MA) approved the construction of the MIMIC-III database, and approval was obtained for collecting original information.
Data Availability
All data generated in this study is provided in the results and/or in the supplementary material file.
Author information
Authors and Affiliations
Corresponding authors
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sun, W., Wang, L., Yuan, S. et al. Association Between Percutaneous Oxygen Saturation and Mortality of Patients with Mild Traumatic Brain Injury at ICU Admission: An Analysis of the MIMIC-III Database. Adv Ther 40, 2773–2783 (2023). https://doi.org/10.1007/s12325-023-02499-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-023-02499-w