Abstract
Aim
To evaluate the differences in the continuous glucose monitoring system (CGMS) profiles of women in early pregnancy stratified based on different HbA1c levels known to be predictive of gestational diabetes mellitus (GDM) at 24–28 weeks of gestation (≥ 5.2%) and adverse pregnancy outcomes (≥ 5.5%) in Indian women.
Methods
We enrolled women at 8+ 0 to 19+ 6 weeks of gestation (early pregnancy), evaluated the glycaemic parameters of clinical interest using CGMS, and reported them per standard methodology proposed by Hernandez et al. WHO 2013 criteria were used for diagnosis of early GDM.
Results
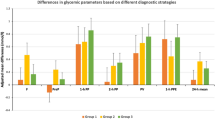
Ninety-six women were enrolled at 14.0 ± 3.2 weeks of gestation. Of these, 38 were found to have early GDM (diagnosed before 20 weeks of gestation) on evaluation. Of 96 women, 33 (34.4%) had HbA1c value ≥ 5.5% [11 (19.0%) with normoglycaemia and 22 (57.9%) with GDM]. The women with elevated HbA1c differed significantly from those with HbA1c < 5.5% for all evaluated parameters. The differences for overall women were > 10 mg/dl (0.56 mmol/l) for 1-h postprandial glucose (difference of 0.78 mmol/l), 2-h postprandial glucose (difference of 0.59 mmol/l), peak postprandial glucose (difference of 0.75 mmol/l), and 1-h postprandial glucose excursion (difference of 0.59 mmol/l). Of 58 women with normoglycaemia, 29 (50.0%) had an HbA1c value ≥ 5.2%. In comparison, in the normoglycaemic group of women with and without HbA1c ≥ 5.2% (known to be predictive of future GDM), the results were significant for 1-h (difference of 0.44 mmol/l), 2-h (difference of 0.278 mmol/l), and peak postprandial glucose (difference of 0.35 mmol/l).
Conclusions
The results suggest that women with elevated HbA1c (≥ 5.5%) in early pregnancy significantly differ from those with HbA1c < 5.5% in all glycaemic parameters evaluated in this study, suggesting that HbA1c at this cut-off has a role to play in early pregnancy.
Similar content being viewed by others
References
Sweeting A, Wong J, Murphy HR, Ross GP. A clinical update on gestational diabetes mellitus. Endocr Rev. 2022;43:763–93. https://doi.org/10.1210/endrev/bnac003.
Vince K, Perković P, Matijević R. What is known and what remains unresolved regarding gestational diabetes mellitus (GDM). J Perinat Med. 2020;48:757–63. https://doi.org/10.1515/jpm-2020-0254.
International Association of Diabetes and Pregnancy Study Groups Consensus Panel, Metzger BE, Gabbe SG, Persson B, Buchanan TA, Catalano PA, et al. International association of diabetes and pregnancy study groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care. 2010;33:676–82. https://doi.org/10.2337/dc09-1848.
HAPO Study Cooperative Research Group, Metzger BE, Lowe LP, Dyer AR, Trimble ER, Chaovarindr U, et al. Hyperglycemia and adverse pregnancy outcomes. N Engl J Med. 2008;358:1991–2002. https://doi.org/10.1056/NEJMoa0707943.
Diagnostic criteria and classification of hyperglycaemia first detected in pregnancy: a World Health Organization guideline. Diabetes Res Clin Pract 2014; 103: 341–363. https://doi.org/10.1016/j.diabres.2013.10.012
Zhu WW, Yang HX, Wei YM, Yan J, Wang ZL, Li XL, et al. Evaluation of the value of fasting plasma glucose in the first prenatal visit to diagnose gestational diabetes mellitus in china. Diabetes Care. 2013;36:586–90. https://doi.org/10.2337/dc12-1157.
Cosson E, Carbillon L, Valensi P. High fasting plasma glucose during early pregnancy: a review about early gestational diabetes mellitus. J Diabetes Res. 2017;2017:8921712. https://doi.org/10.1155/2017/8921712.
van Leeuwen M, Opmeer BC, Yilmaz Y, Limpens J, Serlie MJ, Mol BW. Accuracy of the random glucose test as screening test for gestational diabetes mellitus: a systematic review. Eur J Obstet Gynecol Reprod Biol. 2011;154:130–5. https://doi.org/10.1016/j.ejogrb.2010.11.002.
Draznin B, Aroda VR, Bakris G, Benson G, American Diabetes Association Professional Practice Committee; American Diabetes Association Professional Practice Committee, et al. Management of diabetes in pregnancy: standards of medical care in diabetes-2022. Diabetes Care. 2022;45(Suppl 1):S232–43. https://doi.org/10.2337/dc22-S015.
McIntyre HD, Sacks DA, Barbour LA, Feig DS, Catalano PM, Damm P, McElduff A. Issues with the diagnosis and classification of hyperglycemia in early pregnancy. Diabetes Care. 2016;39:53–4. https://doi.org/10.2337/dc15-1887.
Kattini R, Hummelen R, Kelly L. Early gestational diabetes mellitus screening with glycated hemoglobin: a systematic review. J Obstet Gynaecol Can. 2020;42:1379–84. https://doi.org/10.1016/j.jogc.2019.12.015.
Sweeting AN, Ross GP, Hyett J, Molyneaux L, Tan K, Constantino M, Harding AJ, Wong J. Baseline HbA1c to identify high-risk gestational diabetes: utility in early vs standard gestational diabetes. J Clin Endocrinol Metab. 2017;102:150–6. https://doi.org/10.1210/jc.2016-2951.
Bender WR, McCarthy C, Elovitz M, Parry S, Durnwald C. Adverse pregnancy outcomes in nondiabetic patients with an elevated early pregnancy HbA1c. Am J Perinatol. 2022;29:1496–502. https://doi.org/10.1055/a-1877-8696.
Polsky S, Garcetti R. CGM, pregnancy, and remote monitoring. Diabetes Technol Ther. 2017;19(S3):S49–59. https://doi.org/10.1089/dia.2017.0023.
Singh C, Gupta Y, Goyal A, Kalaivani M, Garg V, Bharti J, Singhal S, Kachhawa G, Kulshrestha V, Kumari R, Mahey R, Sharma JB, Bhatla N, Khadgawat R, Gupta N, Tandon N. Glycemic profile of women with normoglycemia and gestational diabetes mellitus during early pregnancy using continuous glucose monitoring system. Diabetes Res Clin Pract. 2020;169: 108409. https://doi.org/10.1016/j.diabres.2020.108409.
Gupta Y, Singh C, Goyal A, Mani K, Bharti J, Singhal S, et al. Continuous glucose monitoring system profile of women diagnosed as gestational diabetes mellitus by International Association of Diabetes and Pregnancy Study Groups criteria and labeled as normoglycemic by alternate criteria in early pregnancy. J Diabetes Investig. 2022;13:1753–60. https://doi.org/10.1111/jdi.13865.
Gupta Y, Singh C, Goyal A, Kalaivani M, Bharti J, Singhal S, et al. Continuous glucose monitoring system profile of women with gestational diabetes mellitus missed using isolated fasting plasma glucose-based strategies alternative to WHO 2013 criteria: a cross-sectional study. Diabetes Ther. 2022. https://doi.org/10.1007/s13300-022-01317-w.
Hernandez TL, Barbour LA. A standard approach to continuous glucose monitor data in pregnancy for the study of fetal growth and infant outcomes. Diabetes Technol Ther. 2013;15:172–9. https://doi.org/10.1089/dia.2012.0223.
Punnose J, Malhotra RK, Sukhija K, Rijhwani RM, Choudhary N, Sharma A, Vij P, Bahl P. Is HbA1c in the first trimester associated with adverse outcomes among pregnant Asian Indian women without gestational diabetes? J Diabetes Complic. 2022;36: 108187. https://doi.org/10.1016/j.jdiacomp.2022.108187.
Punnose J, Malhotra RK, Sukhija K, Mathew A, Sharma A, Choudhary N. Glycated haemoglobin in the first trimester: a predictor of gestational diabetes mellitus in pregnant Asian Indian women. Diabetes Res Clin Pract. 2020;159: 107953. https://doi.org/10.1016/j.diabres.2019.107953.
Yin B, Hu L, Meng X, Wu K, Zhang L, Zhu Y, Zhu B. Association of higher HbA1c within the normal range with adverse pregnancy outcomes: a cross-sectional study. Acta Diabetol. 2021;58:1081–9. https://doi.org/10.1007/s00592-021-01691-0.
Bi J, Ji C, Wu Y, Wu M, Liu Y, Song L, et al. Association Between Maternal Normal Range HbA1c Values and Adverse Birth Outcomes. J Clin Endocrinol Metab. 2020;105(6):dgaa127. https://doi.org/10.1210/clinem/dgaa127.
Mañé L, Flores-Le Roux JA, Gómez N, Chillarón JJ, Llauradó G, Gortazar L, et al. Association of first-trimester HbA1c levels with adverse pregnancy outcomes in different ethnic groups. Diabetes Res Clin Pract. 2019;150:202–10. https://doi.org/10.1016/j.diabres.2019.03.017.
Immanuel J, Simmons D, Desoye G, Corcoy R, Adelantado JM, Devlieger R, et al. Performance of early pregnancy HbA1c for predicting gestational diabetes mellitus and adverse pregnancy outcomes in obese European women. Diabetes Res Clin Pract. 2020;168: 108378. https://doi.org/10.1016/j.diabres.2020.108378.
Battelino T, Danne T, Bergenstal RM, Amiel SA, Beck R, Biester T, et al. Clinical targets for continuous glucose monitoring data interpretation: recommendations from the international consensus on time in range. Diabetes Care. 2019;42:1593–603. https://doi.org/10.2337/dci19-0028.
Acknowledgements
The authors thank study participants for generously donating their time and information. The authors thank Yatender Singh, Ankit Rajput, Balram, Arun Kumar, and Sandhya Sharma for assistance in conducting the study. The authors also acknowledge the contributions of faculty and resident doctors of the Department of Obstetrics and Gynaecology and Department of Endocrinology and Metabolism, AIIMS, New Delhi, who were involved in care of these women and helped in recruitment of the participants.
Funding
No funding or sponsorship was received for this study or publication of this article.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authors’ Contributions
Yashdeep Gupta conceptualised this paper and wrote the first draft. Charandeep Singh and Yashdeep Gupta were involved in conceptualisation of research and its execution. Mani Kalaivani provided inputs in the statistical part. All authors contributed to manuscript editing and its final approval for publication of this work. Yashdeep Gupta is the guarantor of this work and has full access to the data.
Disclosures
Yashdeep Gupta, Charandeep Singh, Alpesh Goyal, Mani Kalaivani, Neerja Bhatla, and Nikhil Tandon have nothing to disclose.
Compliance with Ethics Guidelines
The study was approved by the institutional ethics committee of the All India Institute of Medical Sciences, New Delhi, India (reference no. IECPG-96/22.03.2017 dated 24.03.2017), and informed consent was obtained from all participants. The study was conducted in accordance with the International Conference on Harmonisation Guidelines for Good Clinical Practice and the Declaration of Helsinki.
Data Availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gupta, Y., Singh, C., Goyal, A. et al. Continuous Glucose Monitoring System Profile of Women Stratified Using Different Levels of Glycated Hemoglobin (HbA1c) in Early Pregnancy: A Cross-sectional Study. Adv Ther 40, 951–960 (2023). https://doi.org/10.1007/s12325-022-02405-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-022-02405-w