Abstract
Introduction
Lazertinib is an irreversible, mutant-selective epidermal growth factor receptor (EGFR) tyrosine kinase inhibitor (TKI). Co-administration of TKIs with acid-reducing agents (ARAs) can lead to potential drug–drug interactions, which decreases solubility and absorption of TKIs and is ultimately associated with reduced efficacy of TKIs. This retrospective analysis evaluated the effect of ARAs on the pharmacokinetics of lazertinib using data obtained from patients with advanced EGFR mutation-positive non-small-cell lung cancer.
Methods
In a total of 234 patients with lazertinib pharmacokinetics observed at steady state, dose-normalized (DN) area under the concentration–time curve (AUCss), maximum concentration (Cmax,ss), and/or trough concentration on day 15 (CD15) were compared between a group receiving ARA concomitantly for at least 4 days (ARA group) and another group not receiving ARA (non-ARA group) in a dose-proportional range. Additionally, a comparison of pharmacokinetic parameters at a therapeutic dose of 240 mg once daily was evaluated.
Results
Geometric mean ratios (GMRs) with 90% confidence intervals (CIs) of ARA group to non-ARA group for DNAUCss, DNCmax,ss, and DNCD15 at 40 mg to 320 mg once daily showing the dose proportionality were 0.8743 (0.7285–1.0493), 0.9035 (0.7482–1.0910), and 0.9126 (0.7364–1.1311), respectively. GMRs with 90% CIs for AUCss, Cmax,ss, and CD15 at 240 mg were 0.9136 (0.6637–1.2576), 0.9012 (0.6703–1.2116), and 0.8850 (0.6463–1.2118), respectively.
Conclusion
All pharmacokinetic parameters were not significantly different between the two groups (p values > 0.05), indicating that co-administered ARAs did not significantly affect the steady state pharmacokinetics of lazertinib. Therefore, no dose adjustment of lazertinib is required in patients receiving concomitant ARAs.
ClinicalTrials.gov identifiers
NCT03046992, NCT04075396.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Lazertinib is an irreversible, mutant-selective epidermal growth factor receptor (EGFR) tyrosine kinase inhibitor (TKI). |
Co-administration of TKIs with acid-reducing agents (ARAs) can lead to potential drug–drug interactions, which decreases solubility and absorption of TKIs and is ultimately associated with reduced efficacy of TKIs. |
ARAs did not significantly affect the pharmacokinetics of lazertinib at the steady state when administered together. |
Concomitant use of ARAs is not expected to affect the antitumor efficacy of lazertinib. |
No separate dose adjustment is required for both ARAs and lazertinib in patients receiving both drugs concomitantly. |
Introduction
Lazertinib (YH25448, JNJ-73841937) is a potent, irreversible, brain-penetrant, mutant-selective, and wild-type-sparing third-generation epidermal growth factor receptor (EGFR) tyrosine kinase inhibitor (TKI) [1]. Lazertinib 240 mg was approved for oral administration once-daily in January 2021 by the Ministry of Food and Drug Safety (MFDS) in South Korea as monotherapy for patients with locally advanced or metastatic EGFR T790M mutation-positive non-small cell lung cancer (NSCLC) who have progressed on or after EGFR TKI therapy [2]. Most patients with EGFR mutant NSCLC who receive EGFR TKIs are resistant to first or second-generation EGFR TKIs [3,4,5], so third-generation EGFR TKIs, such as lazertinib, against T790M+ tumors are currently needed. In addition, lazertinib is expected to be effective in treating patients with NSCLC and brain metastasis owing to good blood–brain barrier penetration, as well as for the treatment of primary lung lesions and extracranial lesions [6, 7]. Lazertinib has shown well-tolerated safety and promising clinical activity in a first-in-human phase 1/2 study (LASER201 study) [8].
Acid-reducing agents (ARAs) neutralize stomach acid and relieve stomach pain, indigestion, gastritis, and stomach ulcers. ARAs may also be prescribed for prevention if the patient has other medical conditions that can cause gastrointestinal problems or is taking medications related to gastrointestinal irritation. As such, ARAs are one of the most prescribed drugs worldwide. ARAs mainly include proton pump inhibitors (PPIs), which reduce acid production by inhibiting the hydrogen-potassium adenosine-triphosphatase enzyme system, and H2 receptor antagonists (H2RAs), which reduce acid secretion by interfering with H2 receptors [9]. Taking ARAs can alter the solubility of other drugs by suppressing gastric acid secretion and raising the body’s pH, thereby changing pharmacokinetics such as drug bioavailability.
Given that 2–30% of all patients with cancer are taking ARAs (especially PPIs, which account for about 70% of ARA prescriptions) [10], clinically relevant drug–drug interactions (DDIs) with ARAs should be considered when prescribing TKIs because ARAs may alter the pharmacokinetic (PK) properties of TKIs [11, 12]. In the case of gefitinib and erlotinib, which are classified as first-generation EGFR-targeted therapeutics, TKI exposure tends to decrease when the body’s pH rises as a result of concomitant ARAs [13]. When gefitinib was co-administered with ranitidine (an H2RA), the area under the plasma concentration–time curve (AUC) and maximum plasma concentration (Cmax) of gefitinib decreased to 45% and 70%, respectively [14, 15]. The AUC and Cmax of erlotinib decreased by 30–45% and 50–60%, respectively, when co-administered with omeprazole (one of the PPIs) or ranitidine [16, 17]. Prescribing information for gefitinib and erlotinib indicates that concomitant use of ARAs should be avoided [14, 16].
The solubility of lazertinib in aqueous media is pH-dependent, defined as soluble at pH 1.2–4.0 but practically insoluble at pH 7.0–8.0, with the solubility decreasing between pH 5.0 and 6.0 [18]. Accordingly, it was necessary to investigate whether ARAs would alter the pharmacokinetics of lazertinib, exploring the potential to affect the antitumor effects of lazertinib. In this retrospective PK analysis, the impact of ARAs on the pharmacokinetics of lazertinib was evaluated to examine the potential for DDIs, using data obtained from patients with EGFR mutation-positive advanced NSCLC.
Methods
Compliance with Ethics Guidelines
Since this study is a post hoc analysis of the LASER201 study, the ethics compliance of this study is the same as that of the LASER201 study. The clinical protocol of the LASER201 study was approved by the institutional review boards or ethics committees of all participating centers. The LASER201 study was conducted according to the protocol and the principles expressed in the Helsinki Declaration. All patients or legally permitted representatives provided written consent to LASER201 study participation and related publications prior to any study-related procedures being conducted. The clinical protocol and informed consent form specified overall potential exploratory research of pharmacokinetics, pharmacodynamics, and safety of lazertinib.
Clinical Study Design and Data Collection
PK data of lazertinib and co-administration information with ARAs from the LASER201 study were used in this analysis. Detailed information about the methods and results of the LASER201 study has been described previously [8, 19]. In brief, the study was an open-label, multicenter, phase 1/2 study to evaluate the efficacy, pharmacokinetics, and safety of lazertinib in patients with EGFR mutation-positive advanced NSCLC. All patients in the study received 20, 40, 80, 120, 160, 240, or 320 mg of lazertinib once daily under fasting conditions on a 21-day cycle.
For each PK evaluable patient, AUC during the dosing interval at steady state (AUCss), Cmax at steady state (Cmax,ss), and/or trough plasma concentration of lazertinib on day 15 of cycle 1 (CD15) of lazertinib were obtained. The AUCss and Cmax,ss were calculated by non-compartmental methods with actual sampling times based on the plasma concentrations over the dosing interval after the 22nd multiple dosing of 20 to 320 mg once daily (day 1 of cycle 2), and the CD15 was the trough plasma concentration measured immediately before the 15th multiple dosing.
Patients with concomitant PPIs and/or H2RAs for at least 4 days immediately before evaluation of PK parameters of lazertinib were classified into an ARA group in this analysis. The remaining patients, who did not receive concomitant PPIs and/or H2RAs for at least 4 days, were classified into a non-ARA group.
Assessments of Dose Proportionality
Dose range showing the dose proportionality was explored to compare the dose-normalized (DN) PK parameters between the ARA group and non-ARA group in the range. The dose proportionality of lazertinib was assessed using a power model with natural log-transformed AUCss, Cmax,ss, and CD15 values as dependent variables and the natural log-transformed dose as an independent variable:
This is, PK parameter = eα × (dose)β where α is the intercept, and β is the slope, measuring the extent of dose proportionality [20]. Dose proportionality implied that β = 1 and was assessed by estimating β along with its 90% confidence interval (CI). If the AUCss, Cmax,ss, and CD15 were not dose proportional over the dose range of 20 to 320 mg, the dose proportionality was reassessed by sequentially excluding one dose level farthest from 240 mg (i.e., in the order of 20 → 40 → 80 → 120 mg). The 160 mg and 320 mg doses were not excluded to ensure the range of three or more dose levels around the therapeutic dose of 240 mg in the dose proportionality assessment. However, to prevent data loss in the ARA group, the sequential dose exclusion was discontinued if the dose level with at least one patient who had co-administration of ARAs was met. If any of the 90% CIs of the slope for the AUCss, Cmax,ss, and CD15 did not include 1, the dose range with the slopes closest to 1 was explored.
Assessments of the Effect of Acid-Reducing Agents
In the dose range with the dose proportionality or closest to the dose proportionality, the dose-normalized AUCss (DNAUCss), dose-normalized Cmax,ss (DNCmax,ss), and dose-normalized CD15 (DNCD15) values were summarized according to the ARA group and non-ARA group. An analysis of variance was performed on natural log-transformed values for the dose-normalized PK parameters, with the group (ARA group or non-ARA group) as a fixed effect. In addition, the point estimate and 90% CI of geometric mean ratio of ARA group to non-ARA group were calculated to compare the pharmacokinetics of lazertinib between the two groups. The AUCss, Cmax,ss, and CD15 values at 240 mg were further analyzed in the same method.
Analysis Software
Calculation of PK parameters and all statistical analyses were performed using Phoenix WinNonlin (Certara, LP, Princeton, NJ, USA; version 8.3).
Results
Patient Disposition
A total of 234 patients included in the study had PK parameters of at least one of AUCss, Cmax,ss, or CD15 (Table 1). A total of 127 patients had AUCss and Cmax,ss values, of which 19 patients were classified into the ARA group and 108 patients into the non-ARA group. A total of 229 patients had CD15 values, of which 23 patients were classified into the ARA group and 206 patients into the non-ARA group. The dose level not classified as ARA group in any patient was only 20 mg. Demographics and baseline characteristics of liver and renal function of the patients between the ARA group and non-ARA group are shown in Table S1 in the supplementary material. There were no baseline differences between the two groups that could significantly affect the interpretation of the effect of ARAs on the pharmacokinetics of lazertinib. The ARA administration information for the ARA group is summarized in Table S2 in the supplementary material.
Dose Proportionality
The Cmax,ss increased in a dose-proportional manner over the dose range of 20 to 320 mg (90% CI of slope in the power model, Cmax,ss 0.9790–1.1633) (Table 2). However, the AUCss and CD15 increased in a slightly more than dose-proportional manner over the dose range of 20 to 320 mg (90% CI of slope in the power model, AUCss 1.0042–1.1827, CD15 1.0731–1.2671). As no patient at 20 mg was classified into the ARA group (Table 1), the dose proportionality was reassessed by excluding 20 mg. In the dose range of 40 to 320 mg, the AUCss and Cmax,ss increased in a dose-proportional manner, but the CD15 increased in the slightly more than dose-proportional manner (90% CI of slope in the power model, AUCss 0.9706–1.1617, Cmax,ss 0.9533–1.1507, CD15 1.0470–1.2557) (Table 2 and Fig. 1). The sequential dose exclusion for the dose proportionality assessment was discontinued because at least one patient at 40 mg and higher doses was classified into the ARA group.
Dose proportionality of lazertinib in the dose range of 40 to 320 mg. The circles represent the observed values, the black straight line represents the linear regression line, and the red and blue dashed lines represent the 90% confidence limits and 90% prediction limits, respectively: a ln(AUCss) versus ln(dose); b ln(Cmax,ss) versus ln(dose); c ln(CD15) versus ln(dose)
In the dose range of 40 to 320 mg, the AUCss and Cmax,ss increased in a dose-proportional manner, and the slope values of the AUCss, Cmax,ss, and CD15 were closest to 1. Therefore, the use of the dose-normalized PK parameters in the dose range of 40 to 320 mg was judged to be appropriate to explore the effect of the ARAs on the pharmacokinetics of lazertinib.
Effect of Acid-Reducing Agents in Dose Range of 40 to 320 mg
For the AUCss and Cmax,ss analysis, a total of 124 patients who had administered 40 to 320 mg of lazertinib with the dose proportionality were included, of which 19 patients were classified into the ARA group and 105 patients into the non-ARA group (Tables 1 and 2). For the CD15 analysis, a total of 226 patients who had administered 40 to 320 mg of lazertinib closest to the dose proportionality were included, of which 23 patients were classified into the ARA group and 203 patients into the non-ARA group.
In the dose range of 40 to 320 mg of lazertinib, the arithmetic means (arithmetic coefficient of variation %, CV%) for the DNAUCss were 25.51 (59.9%) and 27.61 (42.9%) h·ng/mL/mg in the ARA group and non-ARA group, respectively (Table 3). The arithmetic means (arithmetic CV%) for the DNCmax,ss were 1.97 (50.1%) and 2.14 (44.3%) ng/mL/mg in the ARA group and non-ARA group, respectively. The arithmetic means (arithmetic CV%) for the DNCD15 were 0.66 (62.1%) and 0.72 (63.4%) ng/mL/mg in the ARA group and non-ARA group, respectively. There were no noticeable differences in the distribution of lazertinib exposure between the two groups at both 40 to 320 mg dose range (Fig. 2).
Comparison of the dose-normalized pharmacokinetic parameters of lazertinib between the ARA and non-ARA groups in the dose range of 40 to 320 mg. The dashed and solid lines across each box represent the median and arithmetic mean of the dose-normalized pharmacokinetic parameters, respectively. The upper and lower whiskers represent the maximum and minimum values within 1.5-fold interquartile range: a dose-normalized AUCss; b dose-normalized Cmax,ss; c dose-normalized CD15
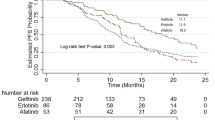
The geometric mean ratios (90% CIs) of ARA group to non-ARA group for the DNAUCss, DNCmax,ss, and DNCD15 were 0.8743 (0.7285–1.0493), 0.9035 (0.7482–1.0910), and 0.9126 (0.7364–1.1311), respectively (Table 4 and Fig. 4). On the basis of the results of the analysis of variance (Table 5), the DNAUCss, DNCmax,ss, and DNCD15 were not significantly different between the two groups (all p values > 0.05).
Effect of Acid-Reducing Agents at 240 mg
A total of 115 patients received 240 mg of lazertinib among all 234 patients who had at least one of the PK parameters in the study (Table 1). Of these, for the AUCss and Cmax,ss analysis at 240 mg, a total of 33 patients were included, of which 9 patients were classified into the ARA group and 24 patients into the non-ARA group. For the CD15 analysis at 240 mg, a total of 125 patients were included, of which 10 patients were classified into the ARA group and 115 patients into the non-ARA group.
In the lazertinib 240 mg group, the arithmetic means (arithmetic CV%) for the AUCss were 6673.26 (66.8%) and 6754.43 (48.9%) h·ng/mL in the ARA group and non-ARA group, respectively (Table 3). The arithmetic means (arithmetic CV%) for the Cmax,ss at 240 mg were 492.73 (54.7%) and 522.39 (40.4%) ng/mL in the ARA group and non-ARA group, respectively. The arithmetic means (arithmetic CV%) for the CD15 at 240 mg were 159.01 (62.4%) and 175.70 (59.4%) ng/mL in the ARA group and non-ARA group, respectively. There were no noticeable differences in the distribution of lazertinib exposure between the two groups at 240 mg (Fig. 3).
Comparison of the pharmacokinetic parameters of lazertinib between the ARA and non-ARA groups at 240 mg. The dashed and solid lines across each box represent the median and arithmetic mean of the pharmacokinetic parameters, respectively. The upper and lower whiskers represent the maximum and minimum values within 1.5-fold interquartile range: a AUCss; b Cmax,ss; c CD15
The geometric mean ratios (90% CIs) of ARA group to non-ARA group for the AUCss, Cmax,ss and CD15 were 0.9136 (0.6637–1.2576), 0.9012 (0.6703–1.2116), and 0.8850 (0.6463–1.2118), respectively (Table 4 and Fig. 4). According to the analysis of variance (Table 5), the AUCss, Cmax,ss, and CD15 at 240 mg did not show any significant difference between the two groups (all p values > 0.05).
Geometric mean ratios of ARA group to non-ARA group with 90% confidence intervals of pharmacokinetic parameters of lazertinib: empty circle, square, and triangle represent the geometric mean ratio of the dose-normalized AUCss, Cmax,ss, and CD15 of ARA group to non-ARA group, respectively, in the dose range of 40 to 320 mg. Filled circle, square, and triangle represent the geometric mean ratio of the dose-normalized AUCss, Cmax,ss, and CD15 of ARA group to non-ARA group, respectively, at 240 mg. The line extending from the point represents the 90% confidence interval for each geometric mean ratio
Discussion
In 2020, lung cancer had the highest mortality rate compared to other cancers according to GLOBOCAN, which provides global cancer statistics including cancer incidence and mortality [21]. Therefore, lung cancer is the leading cause of cancer death worldwide, with NSCLC accounting for approximately 85% of patients with lung cancer [22]. Treatment of advanced NSCLC is initially decided by the molecular subtypes of the tumor, and EGFR TKIs are recommended as first-line therapy in the presence of EGFR mutations. Considering that ARAs are widely used as adjuvant therapy for patients with cancer because of gastroesophageal reflux diseases or gastritis, many studies have been conducted on how the pH change in the body caused by the use of ARAs changes the blood concentration of anticancer drugs [10, 23]. Pharmacokinetics of TKIs may vary significantly as a result of these drug interactions, which may increase the interpatient variability and lead to subsequent risks of decreased therapeutic outcomes [24]. Considering that the solubility of lazertinib decreased with increasing pH in an in vitro study [18], it was necessary to evaluate the effect of ARAs on the pharmacokinetics of lazertinib with clinical data. In vitro study showed that lazertinib was predominantly metabolized by cytochrome P450 (CYP) 3A4, and all patients were prohibited concomitant use of medications, herbal supplements, and/or ingestion of foods with known potent inducer/inhibitory effects on CYP3A4 activity throughout the clinical study. Therefore, we could rule out a confounding effect between ARAs and CYP3A4 inhibitors or inducers on the pharmacokinetics of lazertinib [8].
There is no standard criterion for the duration of ARAs administration to evaluate DDI with ARAs. A review by Hussaarts et al. reported that ARAs may affect the pharmacokinetics of multikinase inhibitors, including the tyrosine kinase inhibitors, and the duration of ARA administration to evaluate DDI regarding gastric acid suppression varied from 1 to 7 consecutive days [24]. Ideally, changes in exposure to TKIs should be observed after the repeated administrations of ARAs for a period that can ensure the maximal intragastric pH-elevating effect of ARAs. PPIs are slow to reach steady-state inhibition of gastric acid secretion, typically taking approximately 4 days by continuous multiple dosing [25,26,27]. For H2RAs, they act quickly with a peak effect of gastric pH elevation at 1–3 h after first dosing [26, 28, 29]. However, other clinical studies have shown that the effect of H2RAs on gastric pH elevation reaches a plateau in 3–4 days after continuous multiple dosing [30, 31]. Therefore, this analysis was performed assuming that the elevation of gastric pH was sufficiently expressed after about 4 days of multiple dosing of H2RA and PPI, which were the criteria for classifying the ARA group and non-ARA group [8, 19]. In the non-ARA group, no one took ARAs for 1, 2, or 3 days during the 4 days immediately before evaluation of the PK parameters of lazertinib.
This study is a retrospective PK analysis that analyzed the PK data obtained from the LASER201 study to understand the effect of ARAs on the pharmacokinetics of lazertinib. Since the steady state was reached within 15 days of once-daily administration of lazertinib [8], the obtained AUCss, Cmax,ss, and CD15 were considered indicative of the steady-state pharmacokinetics of lazertinib. To investigate the effects of ARAs at the therapeutic dose of lazertinib 240 mg as well as a larger sample size, a dose range with dose proportionality was explored, and the effect was assessed using dose-normalized PK parameters of the dose range. ARAs had minimal effect in reducing exposure of lazertinib by approximately 10% at the steady state. Exposure variability of lazertinib with ARAs co-administration was similar to or slightly higher than without ARAs. This difference is likely because the number of subjects classified into the ARA group accounted for approximately 10% of the total subjects, much lower than that of the non-ARA group, indicating relatively high variability within the ARA group. Also, since the exposure variability did not show statistically significant differences between groups, it is difficult to argue that ARAs significantly affected lazertinib exposure. The slight decrease in the systemic exposure of lazertinib observed at a steady state is not clinically relevant on the basis of the results of the LASER201 study, which demonstrated a relatively flat dose–response relationship with a durable response to antitumor effects at doses of lazertinib ranging from 120 to 240 mg, even though the systemic exposure increased dose proportionally. Considering these results, it was recognized that ARAs had little effect on the bioavailability of lazertinib, so the MFDS approved the co-administration of lazertinib and ARAs without changing the dosage regimen of both drugs [2]. In addition, consistent with the findings of this study, a high-fat meal that could increase intragastric pH did not significantly affect the pharmacokinetics of lazertinib in healthy subjects [32, 33].
Since most TKIs are weak bases with pH-dependent solubility, ARAs may decrease their bioavailability [34]. However, other studies have shown that about half of TKIs with pH-dependent solubility did not have a clinically significant effect on their pharmacokinetics caused by ARAs [11, 35]. The solubility of crizotinib decreased at higher pH (> 10 mg/mL at pH 1.6 and 0.1 mg/mL at pH 7.7), but esomeprazole had no clinically significant effect on crizotinib pharmacokinetics [36]. Although nintedanib exhibited a pH-dependent solubility profile with increased solubility at acidic pH < 3, neither PPI nor H2RA affected nintedanib exposure [37]. The solubility of ponatinib at pH 1.7, 2.7, and 7.5 was 7790, 3.44, and 0.16 μg/mL, respectively, but lansoprazole did not have a clinically significant effect on ponatinib exposure [38]. Although cobimetinib exhibited 100-fold less solubility at pH 6.4 compared to pH 1.9, rabeprazole under fed and fasted conditions did not result in a statistically significant effect in cobimetinib exposure [39, 40]. Together, these studies, as well as this analysis for lazertinib, suggest that, even for drugs that exhibit pH-dependent solubility in in vitro, ARAs may not necessarily have a significant effect on their pharmacokinetics in the body.
This study has design limitations in that it is an integrated analysis of the LASER201 study. This study was a post hoc analysis incorporating the four parts of the LASER201 study; thus, the endpoints were not pre-specified, and we did not observe the effect of a specific drug among the ARAs on the pharmacokinetics of lazertinib. In addition, the effect of ARAs was not derived from a within-subject comparison. However, this study is meaningful in that it is the first nationwide study of DDIs between the new EGFR TKI drug lazertinib and ARAs. For appropriate PK analyses within our limited data, we defined the ARA group by ensuring a duration of ARA multiple doses that could maintain the maximum pH of ARAs for each PK parameter most representative of lazertinib exposure. Although the sample size of the ARA group in this study was relatively small, we attempted to reflect the patient’s ARAs prescribed and taken information in the real world, and to consider the appropriate multiple-dose period of ARAs to identify potential DDIs with lazertinib.
In conclusion, ARAs did not significantly affect the pharmacokinetics of lazertinib at the steady state when administered together. Therefore, concomitant use of ARAs is not expected to affect the antitumor efficacy of lazertinib, and it is unlikely that additional consideration should be given to the co-administration of ARA when taking lazertinib. No separate dose adjustment is required for both ARAs and lazertinib in patients receiving both drugs concomitantly.
References
Hong MH, Lee IY, Koh JS, et al. P3.02b–119 YH25448, a highly selective 3rd generation EGFR TKI, exhibits superior survival over osimertinib in animal model with brain metastases from NSCLC: Topic: EGFR RES. J Thorac Oncol. 2017;12(1):S1265–6.
Ministry of Food and Drug Safety Republic of Korea, LECLAZA (lazertinib): prescribing information. 2022.
Westover D, Zugazagoitia J, Cho BC, Lovly CM, Paz-Ares L. Mechanisms of acquired resistance to first- and second-generation EGFR tyrosine kinase inhibitors. Ann Oncol. 2018;1(29):i10–9.
Gao J, Li HR, Jin C, Jiang JH, Ding JY. Strategies to overcome acquired resistance to EGFR TKI in the treatment of non-small cell lung cancer. Clin Transl Oncol. 2019;21(10):1287–301.
Karachaliou N, Fernandez-Bruno M, Paulina Bracht JW, Rosell R. EGFR first- and second-generation TKIs—there is still place for them in EGFR-mutant NSCLC patients. Transl Cancer Res. 2018;2:S23–47.
Yun J, Hong MH, Kim SY, et al. YH25448, an irreversible EGFR-TKI with potent intracranial activity in EGFR mutant non-small cell lung cancer. Clin Cancer Res. 2019;25(8):2575–87.
Kim S-W, Ahn M-J, Han J-Y, et al. Intracranial anti-tumor activity of lazertinib in patients with advanced NSCLC who progressed after prior EGFR TKI therapy: data from a phase I/II study. J Clin Oncol. 2020;38:9571.
Ahn M-J, Han J-Y, Lee KH, et al. Lazertinib in patients with EGFR mutation-positive advanced non-small-cell lung cancer: results from the dose escalation and dose expansion parts of a first-in-human, open-label, multicentre, phase 1–2 study. Lancet Oncol. 2019;20(12):1681–90.
Zhang Y-S, Li Q, He B-S, Liu R, Li Z-J. Proton pump inhibitors therapy vs H2 receptor antagonists therapy for upper gastrointestinal bleeding after endoscopy: a meta-analysis. World J Gastroenterol. 2015;21(20):6341–51.
Smelick GS, Heffron TP, Chu L, et al. Prevalence of acid-reducing agents (ARA) in cancer populations and ARA drug-drug interaction potential for molecular targeted agents in clinical development. Mol Pharm. 2013;10(11):4055–62.
van Leeuwen RWF, Jansman FGA, Hunfeld NG, et al. Tyrosine kinase inhibitors and proton pump inhibitors: an evaluation of treatment options. Clin Pharmacokinet. 2017;56(7):683–8.
Sharma M, Holmes HM, Mehta HB, et al. The concomitant use of tyrosine kinase inhibitors and proton pump inhibitors: prevalence, predictors, and impact on survival and discontinuation of therapy in older adults with cancer. Cancer. 2019;125(7):1155–62.
Budha NR, Frymoyer A, Smelick GS, et al. Drug absorption interactions between oral targeted anticancer agents and PPIs: is pH-dependent solubility the Achilles heel of targeted therapy? Clin Pharmacol Ther. 2012;92(2):203–13.
Food and Drug Administration, IRESSA (gefitinib): prescribing information; 2018.
Tang W, Tomkinson H, Masson E. Effect of sustained elevated gastric pH levels on gefitinib exposure. Clin Pharmacol Drug Dev. 2017;6(5):517–23.
Food and Drug Administration, TARCEVA (erloitinib): prescribing information; 2010.
Chu MP, Ghosh S, Chambers CR, et al. Gastric acid suppression is associated with decreased erlotinib efficacy in non-small-cell lung cancer. Clin Lung Cancer. 2015;16(1):33–9.
Kim SK, LEE DK, Kim SW, et al. Pharmaceutical composition for oral administration comprising aminopyrimidine derivative or its salt. WIPO. 2020. International Publication Number: WO2020079637A1.
Cho BC, Han JY, Kim SW, et al. A phase 1/2 study of lazertinib 240 mg in patients with advanced EGFR T790M-positive NSCLC after previous EGFR tyrosine kinase inhibitors. J Thorac Oncol. 2022;17(4):558–67.
Shin KH, Jeon JY, Jang K, Kim TE, Kim MG. Dose-proportional pharmacokinetic properties of GLA5PR GLARS-NF1 controlled-release pregabalin in healthy Korean volunteers: a randomized, open, single-dose, parallel study. Drug Des Devel Ther. 2018;12:3449–57.
GLOBOCAN. Age-standardized (World) incidence and mortality rates, top 10 cancers. 2020. https://gco.iarc.fr/today/data/factsheets/populations/900-world-fact-sheets.pdf. Accessed Mar 2021.
Barta JA, Powell CA, Wisnivesky JP. Global epidemiology of lung cancer. Ann Glob Health. 2019;85(1):8.
Numico G, Fusco V, Franco P, Roila F. Proton pump inhibitors in cancer patients: how useful they are? A review of the most common indications for their use. Crit Rev Oncol Hematol. 2017;111:144–51.
Hussaarts K, Veerman GDM, Jansman FGA, et al. Clinically relevant drug interactions with multikinase inhibitors: a review. Ther Adv Med Oncol. 2019;11:1758835918818347.
Mori H, Suzuki H. Role of acid suppression in acid-related diseases: proton pump inhibitor and potassium-competitive acid blocker. J Neurogastroenterol Motil. 2019;25(1):6–14.
Patel D, Bertz R, Ren S, Boulton DW, Någård M. A systematic review of gastric acid-reducing agent-mediated drug–drug interactions with orally administered medications. Clin Pharmacokinet. 2020;59(4):447–62.
Shin JM, Sachs G. Pharmacology of proton pump inhibitors. Curr Gastroenterol Rep. 2008;10(6):528–34.
Netzer P, Brabetz-Höfliger A, Bründler R, et al. Comparison of the effect of the antacid Rennie versus low-dose H2-receptor antagonists (ranitidine, famotidine) on intragastric acidity. Aliment Pharmacol Ther. 1998;12(4):337–42.
Hedenström H, Alm C, Kraft M, Grahnén A. Intragastric pH after oral administration of single doses of ranitidine effervescent tablets, omeprazole capsules and famotidine fast-dissolving tablets to fasting healthy volunteers. Aliment Pharmacol Ther. 1997;11(6):1137–41.
McRorie JW, Kirby JA, Miner PB. Histamine2-receptor antagonists: rapid development of tachyphylaxis with repeat dosing. World J Gastrointest Pharmacol Ther. 2014;5(2):57–62.
Hsu TC, Su CF, Leu SC, et al. Omeprazole is more effective than a histamine H2-receptor blocker for maintaining a persistent elevation of gastric pH after colon resection for cancer. Am J Surg. 2004;187(1):20–3.
Simonian HP, Vo L, Doma S, Fisher RS, Parkman HP. Regional postprandial differences in pH within the stomach and gastroesophageal junction. Dig Dis Sci. 2005;50(12):2276–85.
Huh KY, Yu KS, Lee SH, et al. Effects of food and race on pharmacokinetics of lazertinib in healthy volunteers and patients with EGFR mutation positive advanced non-small cell lung cancer. Poster presentation at annual meeting of American Association of Pharmaceutical Scientists (AAPS) 2021 PharmSci 360. W1130–02–08. https://www.eventscribe.net/2021/PharmSci360/fsPopup.asp?efp=RUFBQ05LUEUxMzM0OA&PosterID=405976&rnd=0.2546019&mode=posterinfo. Accessed Oct 20, 2021.
Gay C, Toulet D, Le Corre P. Pharmacokinetic drug-drug interactions of tyrosine kinase inhibitors: a focus on cytochrome P450, transporters, and acid suppression therapy. Hematol Oncol. 2017;35(3):259–80.
Hussaarts KGAM, Veerman GDM, Jansman FGA, van Gelder T, Mathijssen RHJ, van Leeuwen RWF. Clinically relevant drug interactions with multikinase inhibitors: a review. Ther Adv Med Oncol. 2019;4(11):1–34.
Xu H, O’Gorman M, Matschke K, et al. Evaluation of proton pump inhibitor esomeprazole on crizotinib pharmacokinetics in healthy participants. Clin Pharmacol Drug Dev. 2022;11(1):34–42.
Food and Drug Administration, OFEV (nintedanib): Clinical pharmacology and biopharmaceutics reviews; 2014.
Narasimhan NI, Dorer DJ, Davis J, Turner CD, Sonnichsen D. Evaluation of the effect of multiple doses of lansoprazole on the pharmacokinetics and safety of ponatinib in healthy subjects. Clin Drug Investig. 2014;34(10):723–9.
Food and Drug Administration, COTELLIC (cobimetinib): Clinical pharmacology and biopharmaceutics reviews; 2015.
Food and Drug Administration, COTELLIC (cobimetinib): prescribing information; 2018.
Acknowledgements
Funding
LASER201 study Parts A, B, and C were sponsored by Yuhan Corporation and Korea Drug Development Fund funded by the Ministry of Science and ICT, Ministry of Trade, Industry and Energy, and Ministry of Health and Welfare (KDDF-201803-05, Republic of Korea). LASER201 study Part D was sponsored by Janssen Research & Development. No additional funding was received for this work. Yuhan Corporation paid the journal’s Rapid Service and Open Access fees.
Medical Writing, Editorial, and Other Assistance
Bomin Kim wrote the manuscript first, and the rest of the authors supported her.
Authorship
All named authors meet the International Council of Editors of Medical Journals (ICMJE) criteria for authorship for this article. All authors made substantial contributions to the conception or design of this study, contributed to analysis and drafting the work, and approved the version to be published.
Author Contributions
Bomin Kim: wrote the manuscript, performed the literature search, designed analysis and analyzed and interpreted the data; Jungwook Lee and Hyunwoo Jang: designed the LASER201 study and recruited patients; Nami Lee: designed the LASER201 study and collected the data; Jaydeep Mehta: interpreted the data and provided the concept for this analysis; Seong Bok Jang: interpreted the data, provided the concept for this analysis and designed and steered analysis; All authors read and approved the submitted manuscript.
Disclosures
Bomin Kim, Jungwook Lee, Hyunwoo Jang, Nami Lee, and Seong Bok Jang are employees of Yuhan Corporation, Seoul, Republic of Korea. Jaydeep Mehta is an employee of Janssen Research & Development LLC, Spring House, USA, who participated in this study under collaboration with Yuhan Corporation. In November 2018, Yuhan Corporation entered into a licensing and collaboration agreement with Janssen Biotech, Inc. to develop lazertinib for the treatment of patients with NSCLC.
Compliance with Ethics Guidelines
Since this study is a post hoc analysis of the LASER201 study, the ethics compliance of this study is the same as that of the LASER201 study. The clinical protocol of the LASER201 study was approved by the institutional review boards or ethics committees of all participating centers. The LASER201 study was conducted according to the protocol and the principles expressed in the Helsinki Declaration. All patients or legally permitted representatives provided written consent to LASER201 study participation and related publications prior to any study-related procedures being conducted. The clinical protocol and informed consent form specified overall potential exploratory research of pharmacokinetics, pharmacodynamics, and safety of lazertinib.
Data Availability
All data generated or analyzed during this study are included as supplementary information files.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Kim, B., Lee, J., Jang, H. et al. Effects of Acid-Reducing Agents on the Pharmacokinetics of Lazertinib in Patients with EGFR Mutation-Positive Advanced Non-Small-Cell Lung Cancer. Adv Ther 39, 4757–4771 (2022). https://doi.org/10.1007/s12325-022-02286-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-022-02286-z