Abstract
Introduction
Intravenous (IV) iron is the preferred treatment for patients with iron deficiency anemia (IDA) who require rapid replenishment of iron stores or in whom oral iron is not tolerated or effective. Data from two large-scale randomized controlled trials (RCTs) have recently been published reporting the incidence of adjudicated cardiovascular events after ferric derisomaltose (FDI) and iron sucrose (IS). The objective was to calculate the relative incidence of cardiovascular events with FDI and IS, and to conduct an indirect comparison with ferric carboxymaltose (FCM) based on previously published studies of cardiovascular risk.
Methods
RCTs reporting the incidence of blindly adjudicated cardiovascular events in IDA patients treated with IV iron were identified by systematic literature review (SLR). Pairwise random effects meta-analyses of FDI versus IS, and FCM versus IS were conducted for the pre-specified adjudicated composite cardiovascular endpoint of: death due to any cause, nonfatal myocardial infarction, nonfatal stroke, unstable angina requiring hospitalization, congestive heart failure, arrhythmia, and protocol-defined hypertensive and hypotensive events. Analyses were also conducted for the composite endpoint excluding blood pressure events. Meta-analysis results were combined in an adjusted indirect comparison to provide an indirect estimate of cardiovascular risk with FDI versus FCM.
Results
The SLR retrieved 694 unique articles, of which four were RCTs reporting the incidence of the composite cardiovascular endpoint; two studies comparing FCM (N = 1529) with IS (N = 1505), and two studies comparing FDI (N = 2008) with IS (N = 1000). The odds ratios of the composite CV endpoint were 0.59 (95% confidence interval: 0.39–0.90) for FDI versus IS, 1.12 (95% CI 0.90–1.40) for FCM versus IS, and the indirect OR for FDI versus FCM was 0.53 (95% CI 0.33–0.85).
Conclusions
Pooling data from four large-scale RCTs suggested that FDI was associated with significantly lower incidence of cardiovascular adverse events compared to both FCM and IS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Different intravenous iron formulations are associated with different amounts of labile and free iron, which catalyzes the generation of reactive oxygen species; hydroxyl radicals in particular can cause oxidative stress and cell damage, and play a key role in the mechanisms underpinning cardiovascular (CV) diseases. |
A PROSPERO-registered systematic literature review identified four randomized controlled trials (RCTs) of intravenous irons reporting a composite CV endpoint of death due to any cause, nonfatal myocardial infarction, nonfatal stroke, unstable angina requiring hospitalization, congestive heart failure, arrhythmia, and protocol-defined hypertensive and hypotensive events. |
Meta-analyses showed that the pooled odds ratios of the composite CV endpoint were 0.59 (95% confidence interval [CI]: 0.39–0.90) for ferric derisomaltose versus iron sucrose and 1.12 (95% CI 0.90–1.40) for ferric carboxymaltose versus iron sucrose; indirect comparison showed that the odds ratio of the composite CV endpoint was 0.53 (95% CI 0.33–0.85) with ferric derisomaltose versus ferric carboxymaltose. |
The present analysis showed significantly lower incidence of cardiovascular events with ferric derisomaltose versus iron sucrose and ferric carboxymaltose, based on four RCTs conducted in over 6000 patients with iron deficiency anemia of various etiologies, representing the largest and most robust effort to synthesize evidence on the cardiovascular safety of different IV iron formulations to date. |
Further research in the form of a head-to-head RCT of adjudicated cardiovascular event incidence with FCM and FDI should ideally be conducted to confirm the findings of the present study. |
Introduction
Intravenous (IV) iron is widely used to correct iron deficiency in patients with iron deficiency anemia (IDA) of various etiologies, especially in those patients requiring rapid iron replenishment, and in those either intolerant of or unable to absorb oral iron [1, 2]. IV iron has been shown to be superior to oral iron in achieving a sustained hematological response in patients with IDA associated with inflammatory bowel disease, chronic heart failure (CHF), chronic kidney disease (CKD), hemodialysis, heavy uterine bleeding, pregnancy, and when administered prior to surgery for a wide range of indications [3,4,5,6,7,8].
Different IV iron formulations are associated with different amounts of labile and free iron, which is prone to catalyze the generation of reactive oxygen species (ROS), which could potentially overwhelm cellular antioxidant defenses [9,10,11]. Hydroxyl radicals in particular are extremely reactive and therefore toxic, causing oxidative stress and cell damage, and playing a key role in the mechanisms underpinning cardiovascular diseases [12, 13]. IV iron formulations with tighter iron binding result in slower iron release, and thereby allow much higher dosing. In theory this might mitigate, at least in part, the proliferation of labile and free iron and hence also the generation of potentially toxic ROS. Furthermore, IV irons that can be administered at higher doses, and thereby require fewer infusions, will reduce the number of discrete exposures to labile and free iron.
Cardiovascular risk with IV irons has been studied previously, but is not well characterized, particularly when considering the modern, high-dose, rapid-infusion IV iron formulations such as ferric derisomaltose/iron isomaltoside 1000 (Monofer®; Pharmacosmos A/S, Holbæk, Denmark; FDI) and ferric carboxymaltose (Ferinject®; Vifor France, Paris, France; FCM) [14,15,16]. To date, only two large-scale head-to-head randomized controlled trials (RCTs) of the high-dose, rapid infusion IV iron formulations FDI and FCM have been published. The trials, collectively named PHOSPHARE, had identical study designs and showed a better safety profile of FDI versus FCM with regard to hypophosphatemia, and a similar low risk of serious hypersensitivity reactions [17]. The risk of specific cardiovascular events was not examined in PHOSPHARE, however, as the primary endpoints all pertained to incidence of hypophosphataemia [18].
While there is a paucity of data from studies of high methodological quality comparing FDI with FCM directly, there are data comparing the two IV iron formulations with the longer-established comparator of iron sucrose (Venofer®; Vifor France, Paris, France; IS). The results of the FERWONIDA and FERWONNEPHRO RCTs were recently published, comparing FDI with IS in subjects with IDA associated with multiple etiologies, and with non-dialysis dependent chronic kidney disease, respectively [19, 20]. The FERWON RCTs add to an evidence base including the large-scale REPAIR-IDA and 1VIT09031 RCTs comparing FCM with IS [21, 22]. All four RCTs report a common, adjudicated, cardiovascular endpoint of death due to any cause, nonfatal myocardial infarction, nonfatal stroke, unstable angina requiring hospitalization, congestive heart failure, arrhythmia, and protocol-defined hypertensive and hypotensive events.
The objective of the present study was to conduct a systematic literature review to identify any other RCTs of IV irons reporting the incidence of the same composite cardiovascular endpoint and, in the case where sufficient evidence were identified, to conduct random effects meta-analyses of the data and pool the results to obtain estimates of the relative incidence of cardiovascular outcomes with FDI, IS, and FCM.
Methods
Systematic Literature Review
A systematic literature review was conducted to identify RCTs of FDI or FCM versus any other IV iron comparator (including each other), reporting a composite, blindly-adjudicated cardiovascular endpoint of: death due to any cause, nonfatal myocardial infarction, nonfatal stroke, unstable angina requiring hospitalization, congestive heart failure, arrhythmia, and protocol-defined hypertensive and hypotensive events (Supplementary Materials Table 1). Blindly adjudicated in this context refers to the confirmation and classification of all clinical events specified in the trial protocol by a clinical events committee without knowledge of the trial arm in which the event occurred. The selection of the composite endpoint, and the requirement for it to be blindly adjudicated, was based on the endpoint as defined in the FCM pivotal trials as submitted to the US Food and Drug Administration (FDA).
The systematic literature review search terms are documented in Supplementary Materials Table 2 and the review protocol was registered with PROSPERO with ID CRD42021190689. References were retrieved from PubMed, EMBASE, and the Cochrane Library using a combination of free-text terms and Medical Subject Heading (MeSH) terms, and imported into Sourcerer for duplicate removal followed by title and abstract screening against pre-specified inclusion/exclusion criteria (Supplementary Materials Table 3) by two independent researchers [23]. Full-text copies of studies still included after title and abstract screening were then retrieved and assessed against the same inclusion/exclusion criteria. Data were extracted from the studies (and related documentation) by two independent researchers and recorded in structured text files. For each study identified, key population characteristics were extracted, and the number of cardiovascular events was taken from the safety analysis set in each study. The risk of bias of the included studies was assessed using version 2 of the Cochrane Risk of Bias tool [24]. Note that, as a systematic review, meta-analysis, and indirect comparison, the present study is based on previously conducted studies and does not contain any data from studies of human or animal participants performed by any of the authors.
Statistical Analysis
Random effects meta-analyses of FDI versus IS and FCM versus IS were conducted to establish the pooled odds ratios and confidence intervals of the adjudicated composite cardiovascular event for FDI relative to IS, and FCM relative to IS. Analyses were performed using the netmeta package version 2.0-0 in version 4.1 of the R statistical programming language [25]. Meta-analyses were then also conducted for the composite endpoint excluding the hypertension and hypotension events, in line with analyses conducted by the FDA [26]. Random effects meta-analysis models were selected over fixed effects models on the grounds that the RCTs included patients with different IDA etiologies and that the true effect size would be likely to differ between the studies. The DerSimonian and Laird estimator was used to calculate inter-study variance with the Mantel–Haenszel method used to calculate study weights [27, 28]. Heterogeneity between the studies included in each meta-analysis was characterized using I2 and τ2, the former of which quantifies the proportion of the total variance across studies that can be attributed to heterogeneity, and the latter of which provides a point estimate of the among-study variance of true effects [29, 30]. I2 may therefore be interpreted as the proportion of variability in the point estimates that is due to τ2 as opposed to within-study error [30]. An indirect treatment comparison of FDI and FCM was then conducted using the Bucher et al. methodology, relying on the random effects meta-analyses to inform the comparisons of FDI and IS, and FCM and IS [31].
Given the differences in the number of infusions required with IS, FCM, and FDI, patient-level data were obtained from the FERWONNEPHRO study to ascertain if the relative risk of cardiovascular events varied over time, with a specific view to establishing if the number of iron infusions may be a significant effect modifier. A Cox proportional hazards regression model was fit to the time-to-event data and the proportional hazards assumption was validated by testing the time-independence of the Schoenfeld residuals from the Cox model [32].
Sensitivity Analyses
A series of sensitivity analyses were conducted to test the sensitivity of the results to changes in the modeled data and statistical methodology; the random effects models in the meta-analyses were substituted for fixed effects models (thereby assuming one true effect size common to all studies in the analysis), each individual trial was systematically dropped out of the meta-analyses, and the meta-analyses and ITC were re-run based on the data from N-1 trials. Two further analyses were then conducted, one in which the indirect comparison was based exclusively on studies in patients with IDA of any etiology, and one in which the indirect comparison was based exclusively on studies enrolling patients with IDA associated with CKD.
Results
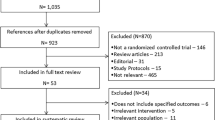
The systematic literature review resulted in the retrieval of 801 studies across PubMed, the Cochrane Library, and EMBASE, of which 107 were duplicates. From the remaining 694 unique studies, 639 were excluded on the basis of the titles and abstracts, leaving 55 RCTs remaining in which the reporting of the composite cardiovascular endpoint could not be definitively ascertained from the title and abstract (Supplementary Materials Fig. 1). After reviewing the full-text manuscripts of the 55 included studies, four large-scale RCTs were ultimately identified reporting the incidence of the blindly-adjudicated composite cardiovascular endpoint; two studies comparing FDI with IS (FERWONIDA and FERWONNEPHRO; Table 1), one study (1VIT09031) comparing FCM with IV standard of care (IVSC), 89.8% of whom were treated with IS, and one study comparing FCM with IS (REPAIR-IDA; Table 2) [19, 21, 22]. A total of 6042 patients were included in the safety analysis populations across the four trials: 2008 receiving treatment with FDI, 1529 receiving treatment with FCM, and 2505 receiving treatment with IS (1000 versus FDI, and 1505 versus FCM).
The Cochrane Risk of Bias 2 tool reported low risk of bias across all four trials, with only the 1VIT09031 trial having any concerns across any of the five domains of the bias analysis, specifically in the randomization domain (Supplementary Materials Fig. 2). All four trials were conducted as open label trials, primarily driven by the need for patients to return for more frequent infusions of iron sucrose; sham infusions were not employed. While randomization was conducted using interactive voice response systems across all four trials, 1VIT09031 was the only trial to report significant differences between any of the reported baseline characteristics; bodyweight was 79.5 kg in the FCM group versus 84.7 kg in the IVSC group.
The 1VIT09031 trial was a four-arm trial including two cohorts: cohort 1, including patients who had responded inadequately to oral iron and cohort 2 including patients for whom oral iron was not appropriate. Patients in cohort 1 were randomly assigned to continue on oral iron or receive FCM, while patients in cohort 2 were assigned to receive either FCM or IVSC. Only the cohort 2 comparison was therefore relevant for the present analysis, and specifically the sub-group of the IVSC arm of the trial that was prescribed IS (89.8% of all patients; n = 220/245). Event counts and the number of exposed patients from the trial were calculated in patients receiving IS in cohort 2 by utilizing a combination of the data published in the study manuscript and data published on the IS subgroup in a report from the Center for Drug Evaluation and Research (CDER; a division of the US FDA) [22, 26]. Event counts and patients exposed in the corresponding cohort 2 FCM arm were taken directly from the manuscript [22].
In each of the four individual trials, patient characteristics were comparable between the trial arms (Table 3). Across the trials, dosing regimens for IS were also comparable, with REPAIR-IDA, FERWONNEPHRO and FERWONIDA specifying either exactly five infusions of IS at 200 mg per infusion or up to five infusions with a total recommended dose of 1000 mg. In the IVSC arm of the 1VIT09031 trial, 93.9% of all IVSC patients received up to five doses of IV iron with a median dose of 800 mg and mean dose of 813 mg, suggesting that the prescribed IS regimens were in close alignment with the other studies. FCM was administered as two doses of 750 mg 1 week apart in both the REPAIR-IDA and 1VIT09031 studies, while FDI was administered in a single 1000-mg dose in both FERWON studies. Schoenfeld residuals from the Cox proportional hazards regression model fit to the patient-level time-to-event data from FERWONNEPHRO showed no significant time-dependency (p = 0.1936), indicating that the cardiovascular event incidence data were not inconsistent with a proportional hazards model and that the different number of infusions in the two trial arms was therefore unlikely to be an effect modifier, despite the differences in overall dosing of the formulations. The proportions of patients experiencing events in the trials, and the trial durations, are presented in Table 4.
The random effects meta-analysis of the studies comparing FDI with IS yielded an odds ratio of 0.59 (95% confidence interval [CI]: 0.39–0.90), corresponding to a 41% reduction in the odds of the composite cardiovascular endpoint with FDI relative to IS. The random effects meta-analysis of the studies comparing FCM with IS yielded an odds ratio of 1.12 (95% CI 0.90–1.40), corresponding to a 12% non-significant increase in the odds of the composite cardiovascular endpoint with FCM relative to IS. Combining the results of the two meta-analyses using the Bucher et al. methodology yielded an odds ratio of 0.53 (95% CI 0.33–0.84) with FDI relative to FCM, corresponding to 47% lower odds of the composite cardiovascular endpoints with FDI relative to FCM (Table 5; Fig. 1). Running the same indirect analysis for the composite endpoint without hypotension or hypertension yielded an odds ratio of 0.54 (95% CI 0.28–1.06) corresponding to a central estimate of 46% lower odds of the endpoint occurring with FDI versus FCM, but with the difference not reaching statistical significance.
As would be anticipated in meta-analyses based on two studies, sensitivity analysis showed that the analysis was insensitive to the use of a random effects versus a fixed effects model. The ITC was also directionally insensitive to the exclusion of individual studies from the meta-analyses (Table 5; Figs. 2, 3) with odds ratios ranging from 0.52 to 0.76; however, removal of the two largest studies by enrollment and event count resulted in odds ratios for FDI versus FCM that were not significant: 0.59 (95% confidence interval 0.20–1.74) when excluding FERWONNEPHRO, and 0.76 (95% confidence interval 0.29–1.99) when excluding REPAIR-IDA. Including only studies conducted in populations with IDA associated with CKD resulted in an odds ratio for the composite cardiovascular endpoint of 0.5 (95% confidence interval 0.30–0.85) with FDI relative to FCM, while including only studies conducted in populations with IDA of any etiology resulted in an odds ratio of 0.85 (95% confidence interval 0.22–3.34) with FDI relative to FCM.
Summary of odds ratios from the random effects meta-analyses of ferric derisomaltose and ferric carboxymaltose versus iron sucrose, and the indirect treatment comparison of ferric derisomaltose and ferric carboxymaltose for A the composite cardiovascular endpoint and B the composite cardiovascular endpoint excluding hypotension and hypertension. CI confidence interval, FCM ferric carboxymaltose, FDI ferric derisomaltose, IS iron sucrose, OR odds ratio
Discussion
The primary indirect treatment comparison showed a significant 47% reduction in the odds of the blindly-adjudicated composite cardiovascular endpoint with FDI versus FCM using IS as an anchor. A scenario analysis excluding hypotension and hypertension from the composite cardiovascular endpoint showed that the odds of experiencing an event with FDI versus FCM would reduce by 46%, but the difference did not reach statistical significance. The full composite endpoint including hypotension and hypertension was developed based on interactions with the FDA during the design of the included trials; however, blood pressure-related adverse events are likely to be acute, peri-infusional events and may not therefore be considered as clinically relevant as the other components of the endpoint.
While the mechanism driving differences in cardiovascular event incidence following administration of IV iron is not known, the catalysis of ROS generation by labile and free iron is one plausible underlying process, with ROS causing oxidative stress and cell damage, which are known mediators of cardiovascular disease [12, 13]. An alternative potential mechanism is the depletion of adenosine triphosphate and 2,3-diphosphoglycerate (both critical intermediate metabolites) arising from hypophosphatemia, which has been proposed specifically as a potential mechanism for cardiomyopathy and arrhythmia; FCM has been shown to result in significantly higher levels of intact fibroblast growth factor-23 and higher incidence of post-infusion hypophosphatemia versus FDI, but further research would be required to definitively demonstrate that this also drives differences in the incidence of cardiovascular events [17, 18].
Other differences between the iron formulations have recently been reported based on indirect comparison; for instance, recent evidence synthesized from prospective clinical trial data suggests that FDI is associated with a significantly lower incidence of serious or severe hypersensitivity reactions (HSRs) than FCM [33]. Collectively, these studies show that, beyond the cost and posological differences, multiple clinical differences may also exist between the high-dose, rapid-administration iron formulations including incidence of hypophosphatemia, HSRs and cardiovascular events.
The analysis had several key strengths, including the large number of patients enrolled in the included trials and the transparent statistical methodology employed to conduct the ITC. Based on data from RCTs enrolling over 6000 patients, the present study represents the largest and most robust comparison of cardiovascular risk in patients with IDA treated with FDI, FCM, and IS conducted to date. Owing to its exclusive reliance on odds ratios (as opposed to pooled individual treatment effect estimates), the Bucher et al. model used to conduct the ITC has the advantage of maintaining the benefits of randomization in each pairwise comparison, minimizing the risk that reported differences between treatments were due to differences in patient risk factors unrelated to the treatment.
The two head-to-head PHOSPHARE RCTs of FDI and FCM, represented the first direct comparisons of the two IV iron formulations in an RCT; however, while the studies showed a reduced incidence of hypophosphatemia and serious or severe HSRs with FDI relative to FCM, cardiovascular outcomes were not reported. Previous studies have shown numerically higher risk of cardiovascular events with FCM relative to ferumoxytol; in a trial that enrolled 1997 patients with IDA, six of 997 (0.6%) of patients treated with ferumoxytol experienced a serious cardiovascular event, none of which was treatment-related, compared with 13 of 1000 (1.3%) with FCM, three of which were considered to be treatment related [34]. While the significance of the difference in the serious cardiovascular event endpoint was not reported, it formed part of a composite secondary endpoint also capturing moderate and severe HSRs, anaphylaxis, and death, the incidence of which was significantly higher with FCM than ferumoxytol (2.0 vs. 1.3%, relative risk 0.7, 95% confidence interval 0.3–1.3. p = 0.0001).
The present study also has a number of limitations that should be acknowledged. The time over which the cardiovascular events were recorded differed between the included studies. Both FERWONIDA and FERWONNEPHRO reported cardiovascular event incidence at 8 weeks, while REPAIR-IDA and 1VIT09031 had a longer follow-up period of 120 days (approximately 17 weeks). Given the anchoring of the treatment comparisons via IS and the exclusive use of odds ratios throughout the analysis, the only scenario in which different follow-up periods would affect the overall odds ratio would be that in which the hazards were not proportional over time (and specifically only if they differed between weeks 0 and 8 and weeks 8 and 17) [35]. Had patient-level time of event data been available from all included trials, this assumption could have been validated by ensuring a constant difference, but evidence from other studies of IV iron formulations suggests that proportional hazards for cardiovascular events are indeed constant over time. For instance, proportional hazards were observed in a large-scale (N = 66,207) retrospective analysis of patients treated with IV iron while on hemodialysis, and there is a substantial body of published literature on the safety of IV iron that is based on statistical methodologies that assume constant proportional hazards over time [36].
Patients in 1VIT09031 treated with IS were not a pre-specified sub-group and the derivation of the event counts from the Onken et al. publication and the CDER report led to a small (0.1%) discrepancy in the calculated number of pooled patients at-risk in the present study (n = 1505) and the CDER report (n = 1503). The present derivation of 1505 is congruous with all of the published data (1285 patients in REPAIR-IDA plus 220 patients receiving IS in the 1VIT09031 study as reported in the CDER report, and 89.8% of 245 patients receiving IS in 1VIT09031 as per Onken et al.) [21, 22]. Ideally, the patients receiving IS would have been rebalanced to match the FCM arm using a technique such as propensity score matching, but the patient-level data from the study were not available. Given that the subgroup comprised 89.8% of the patients originally assigned to the IVSC arm and the absolute event rates were similar in the 89.8% (5%) and the 10.2% (4%), this limitation would have been unlikely to materially affect the findings of the analysis.
One final potential limitation, which may have a bearing on the observed incidence cardiovascular events, is the phenotype of the patients with IDA in the included studies; FERWONNEPHRO and REPAIR-IDA both enrolled patients with non-dialysis dependent (NDD) CKD, while FERWONIDA and 1VIT09031 enrolled patients with IDA of mixed etiologies [19, 21, 22]. In this regard, the two component meta-analyses were similar, each including one large-scale study of IDA in NDD-CKD and one study of IDA associated with multiple non-CKD etiologies. The patient populations of the included studies should be taken into consideration when interpreting the overall findings of the analysis, particularly the inclusion of the two NDD-CKD studies with mean ages across the four trial arms of between 67.2 and 69.3 years. These populations would be expected to have a higher incidence of cardiovascular events than the average IDA population, but the exclusive use of odds ratios (as opposed to absolute event rates) in the Bucher et al. model goes some way to mitigating concerns of the analysis being overly specific to patients with NDD-CKD; if the relative incidence of CV events between treatments would be anticipated to be the same across patients with IDA of differing etiologies, the interpretation of the analysis is unchanged by the absolute event rates in the included studies. A qualitative evaluation of key hematological parameters and use of concomitant erythropoiesis stimulating agents (ESAs) showed average values to be comparable in the trial arms in all four of the included studies (Table 3).
In interpreting the results of the present study, it is also important to consider the relatively short follow-up periods of the trials used to inform the analysis, especially when compared with the much longer follow-up periods of, for instance, the cardiovascular outcomes trials (CVOTs) now mandated by the FDA during the development of drugs for the treatment of type 2 diabetes [37]. These trials are often designed to follow patients until a specific number of cardiovascular events have occurred to ensure the findings are appropriately powered to draw conclusions around relative incidence of a composite cardiovascular endpoint such as major adverse cardiovascular events (MACE), including myocardial infarction, stroke, and cardiovascular death. Conversely, the four RCTs included in the present study were not specifically powered to detect differences in cardiovascular event incidence. FERWONIDA, for example, was powered to detect differences in the co-primary endpoints of serious or severe hypersensitivity reactions and change in Hb from baseline to week 8; cardiovascular adverse event incidence was a secondary safety endpoint. Relatedly, the absolute incidence of the cardiovascular events comprising the composite endpoint should be considered when interpreting the overall odds ratio from the indirect comparison; in the general IDA trials, there were a total of 35 adjudicated events in 1956 patients, corresponding to a crude pooled incidence rate of 1.8% across all three iron formulations. Rates in the CKD trials were much higher, with a total of 408 events in the 4086 patients enrolled, corresponding to a crude pooled incidence of 10.0%; sensitivity analyses in which the CKD trials were removed either individually or together resulted in odds ratios that still directionally favored FDI, but not significantly so.
Conclusions
The present analysis showed significantly lower incidence of cardiovascular events with FDI relative to IS and FCM. The results were based on four large-scale RCTs conducted in over 6000 patients with IDA of various etiologies, representing the largest and most robust effort to synthesize evidence on the cardiovascular safety of different IV iron formulations to date. Further research in the form of a head-to-head RCT of adjudicated cardiovascular event incidence with FCM and FDI should ideally be conducted to confirm the findings of the present study.
References
Dignass AU, Gasche C, Bettenworth D, Birgegård G, Danese S, Gisbert JP, Gomollon F, Iqbal T, Katsanos K, Koutroubakis I, Magro F, Savoye G, Stein J, Vavricka S, European Crohn’s and Colitis Organisation. European consensus on the diagnosis and management of iron deficiency and anaemia in inflammatory bowel diseases. J Crohns Colitis. 2015;9(3):211–22.
KDIGO Anemia Work Group. KDIGO clinical practice guideline for anemia in chronic kidney disease. Kidney Int Suppl. 2012;2:279–335. Available from: https://kdigo.org/wp-content/uploads/2016/10/KDIGO-2012-Anemia-Guideline-English.pdf. Last accessed July 27, 2022.
Avni T, Bieber A, Steinmetz T, Leibovici L, Gafter-Gvili A. Treatment of anemia in inflammatory bowel disease—systematic review and meta-analysis. PLoS ONE. 2013;8(12): e75540.
Bonovas S, Fiorino G, Allocca M, Lytras T, Tsantes A, Peyrin-Biroulet L, Danese S. Intravenous versus oral iron for the treatment of anemia in inflammatory bowel disease: a systematic review and meta-analysis of randomized controlled trials. Medicine (Baltimore). 2016;95(2): e2308.
Avni T, Leibovici L, Gafter-Gvili A. Iron supplementation for the treatment of chronic heart failure and iron deficiency: systematic review and meta-analysis. Eur J Heart Fail. 2012;14(4):423–9.
O’Lone EL, Hodson EM, Nistor I, Bolignano D, Webster AC, Craig JC. Parenteral versus oral iron therapy for adults and children with chronic kidney disease. Cochrane Database Syst Rev. 2019;2:CD007857.
Susantitaphong P, Alqahtani F, Jaber BL. Efficacy and safety of intravenous iron therapy for functional iron deficiency anemia in hemodialysis patients: a meta-analysis. Am J Nephrol. 2014;39(2):130–41.
Reveiz L, Gyte GM, Cuervo LG, Casasbuenas A. Treatments for iron-deficiency anaemia in pregnancy. Cochrane Database Syst Rev. 2011;10:CD003094.
Jahn MR, Andreasen HB, Fütterer S, Nawroth T, Schünemann V, Kolb U, Hofmeister W, Muñoz M, Bock K, Meldal M, Langguth P. A comparative study of the physicochemical properties of iron isomaltoside 1000 (Monofer), a new intravenous iron preparation and its clinical implications. Eur J Pharm Biopharm. 2011;78(3):480–91.
Cabantchik ZI. Labile iron in cells and body fluids: physiology, pathology, and pharmacology. Front Pharmacol. 2014;5:45.
Kruszewski M. Labile iron pool: the main determinant of cellular response to oxidative stress. Mutat Res. 2003;531(1–2):81–92.
Haase M, Bellomo R, Haase-Fielitz A. Novel biomarkers, oxidative stress, and the role of labile iron toxicity in cardiopulmonary bypass-associated acute kidney injury. J Am Coll Cardiol. 2010;55:2024–33.
Panth N, Paudel KR, Parajuli K. Reactive oxygen species: a key hallmark of cardiovascular disease. Adv Med. 2016;2016:9152732.
Toblli JE, Cao G, Angerosa M. Cardiovascular outcomes of intravenous iron in perspective of clinical trials and the use of different iron preparations. Int J Cardiol. 2015;187:196–7.
Kuo KL, Hung SC, Lee TS, Tarng DC. Iron sucrose accelerates early atherogenesis by increasing superoxide production and upregulating adhesion molecules in CKD. J Am Soc Nephrol. 2014;25(11):2596–606.
Hougen I, Collister D, Bourrier M, Ferguson T, Hochheim L, Komenda P, Rigatto C, Tangri N. Safety of intravenous iron in dialysis: a systematic review and meta-analysis. Clin J Am Soc Nephrol. 2018;13(3):457–67.
Wolf M, Rubin J, Achebe M, Econs MJ, Peacock M, Imel EA, Thomsen LL, Carpenter TO, Weber T, Brandenburg V, Zoller H. Effects of iron isomaltoside vs ferric carboxymaltose on hypophosphatemia in iron-deficiency anemia: two randomized clinical trials. JAMA. 2020;323(5):432–43.
Ariyoshi N, Nogi M, Ando A, Watanabe H, Umekawa S. Cardiovascular consequences of hypophosphatemia. Panminerva Med. 2017;59(3):230–40.
Auerbach M, Henry D, Derman RJ, Achebe MM, Thomsen LL, Glaspy J. A prospective, multi-center, randomized comparison of iron isomaltoside 1000 versus iron sucrose in patients with iron deficiency anemia; the FERWON-IDA trial. Am J Hematol. 2019;94(9):1007–14.
Bhandari S, Kalra PA, Berkowitz M, Belo D, Thomsen LL, Wolf M. Safety and efficacy of iron isomaltoside 1000/ferric derisomaltose versus iron sucrose in patients with chronic kidney disease: the FERWON-NEPHRO randomized, open-label, comparative trial. Nephrol Dial Transplant. 2021;36(1):111–20.
Onken JE, Bregman DB, Harrington RA, Morris D, Buerkert J, Hamerski D, Iftikhar H, Mangoo-Karim R, Martin ER, Martinez CO, Newman GE, Qunibi WY, Ross DL, Singh B, Smith MT, Butcher A, Koch TA, Goodnough LT. Ferric carboxymaltose in patients with iron-deficiency anemia and impaired renal function: the REPAIR-IDA trial. Nephrol Dial Transplant. 2014;29(4):833–42.
Onken JE, Bregman DB, Harrington RA, Morris D, Acs P, Akright B, Barish C, Bhaskar BS, Smith-Nguyen GN, Butcher A, Koch TA, Goodnough LT. A multicenter, randomized, active-controlled study to investigate the efficacy and safety of intravenous ferric carboxymaltose in patients with iron deficiency anemia. Transfusion. 2014;54(2):306–15.
Sourcerer. Covalence Research Ltd. London, UK. Available from: https://sourcerer.pro. Last accessed June 5, 2022.
Higgins JP, Savovic J, Page MJ, Sterne JA, ROB2 Development Group. Revised Cochrane risk-of-bias tool for randomized trials (RoB 2) 2019. Available from: https://sites.google.com/site/riskofbiastool/welcome/rob-2-0-tool. Last accessed June 5, 2022.
Rücker G, Krahn U, König J, Efthimiou O, Davies A, Papakonstantinou T, Schwarzer G. netmeta: network meta-analysis using frequentist methods. R package version 2.0-0. Available from: https://CRAN.R-project.org/package=netmeta Last accessed June 14, 2022.
Center for Drug Evaluation and Research. Injectafer (VIT-45, ferric carboxymaltose injection; FCM) for the treatment of iron deficiency anemia. Medical Review. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/nda/2013/203565Orig1s000MedR.pdf Last accessed June 5, 2022.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–88.
Mantel N, Haenszel W. Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst. 1959;22(4):719–48.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60.
Higgins JP. Commentary: heterogeneity in meta-analysis should be expected and appropriately quantified. Int J Epidemiol. 2008;37(5):1158–60.
Bucher HC, Guyatt GH, Griffith LE, Walter SD. The results of direct and indirect treatment comparisons in meta-analysis of randomized controlled trials. J Clin Epidemiol. 1997;50(6):683–91.
Grambsch PM, Therneau TM. Proportional hazards tests and diagnostics based on weighted residuals. Biometrika. 1994;81(3):515–26.
Pollock RF, Biggar P. Indirect methods of comparison of the safety of ferric derisomaltose, iron sucrose and ferric carboxymaltose in the treatment of iron deficiency anemia. Expert Rev Hematol. 2020;13(2):187–95.
Adkinson NF, Strauss WE, Macdougall IC, Bernard KE, Auerbach M, Kaper RF, Chertow GM, Krop JS. Comparative safety of intravenous ferumoxytol versus ferric carboxymaltose in iron deficiency anemia: a randomized trial. Am J Hematol. 2018;93(5):683–90.
Bewick V, Cheek L, Ball J. Statistics review 12: survival analysis. Crit Care. 2004;8(5):389–94.
Brookhart MA, Freburger JK, Ellis AR, Winkelmayer WC, Wang L, Kshirsagar AV. Comparative short-term safety of sodium ferric gluconate versus iron sucrose in hemodialysis patients. Am J Kidney Dis. 2016;67(1):119–27.
Cefalu WT, Kaul S, Gerstein HC, Holman RR, Zinman B, Skyler JS, Green JB, Buse JB, Inzucchi SE, Leiter LA, Raz I, Rosenstock J, Riddle MC. Cardiovascular outcomes trials in type 2 diabetes: where do we go from here? Reflections from a Diabetes Care editors’ expert forum. Diabetes Care. 2018;41(1):14–31.
Acknowledgements
Funding
The study, Rapid Service Fee, and Open Access fees were funded by Pharmacosmos A/S.
Author Contributions
Richard F Pollock, Fozia Z Ahmed, Philip A Kalra, and Paul R Kalra conceived of the analysis. Richard F Pollock and Fozia Z Ahmed designed and executed the literature review. Richard F Pollock conducted the initial analyses and drafted the manuscript. Fozia Z Ahmed, Philip A Kalra, and Paul R Kalra provided clinical input and reviewed the draft manuscript for intellectual content. Richard F Pollock incorporated changes arising from the review and prepared the manuscript for submission.
Disclosures
Fozia Z Ahmed has received speaker/consultancy fees from Pharmacosmos (unrelated to this study) and Vifor. Richard F Pollock is a director of Covalence Research Ltd, which received consultancy fees from Pharmacosmos A/S to conduct the study and write the manuscript. Philip A Kalra has received speaker/consultancy fees from Pharmacosmos and Vifor and has been co-author of several manuscripts relating to analyses and studies sponsored by Pharmacosmos. Paul R Kalra has received speaker/consultancy fees from Pharmacosmos and Vifor and research grants from Pharmacosmos.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any data from studies of human or animal participants performed by any of the authors.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Pollock, R.F., Kalra, P.A., Kalra, P.R. et al. A Systematic Review, Meta-Analysis, and Indirect Comparison of Blindly Adjudicated Cardiovascular Event Incidence with Ferric Derisomaltose, Ferric Carboxymaltose, and Iron Sucrose. Adv Ther 39, 4678–4691 (2022). https://doi.org/10.1007/s12325-022-02242-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-022-02242-x