Abstract
Introduction
To explore the efficacy and safety of intravitreal aflibercept (IVT-AFL) proactive, individualized treat-and-extend (T&E) regimens in exudative age-related macular degeneration (AMD) in the subgroup of patients with polypoidal choroidal vasculopathy (PCV) enrolled in the ALTAIR study.
Methods
This was a PCV subgroup analysis of ALTAIR, a 96-week, randomized, open-label, phase 4 study in treatment-naïve patients with exudative AMD in Japan. Following three initial monthly doses, patients received IVT-AFL at week 16 and were randomized 1:1 to T&E regimens with either 2-week (IVT-AFL-2W) or 4-week (IVT-AFL-4W) adjustments. The primary endpoint of ALTAIR was the mean change in best-corrected visual acuity (BCVA) from baseline to week 52. Endpoints were assessed at weeks 52 and 96. Safety analyses were conducted.
Results
A total of 90 patients with PCV were included within the full analysis set. From baseline to week 52, mean [standard deviation (SD)] change in BCVA was + 7.5 (14.7) letters and + 8.2 (11.6) letters in the IVT-AFL-2W and IVT-AFL-4W groups, respectively. From baseline to week 96, 91.3% and 90.9% of patients maintained vision in the IVT-AFL-2W and IVT-AFL-4W groups, respectively. From baseline to week 52, mean (SD) change in central retinal thickness was − 153 (177) µm and −112 (122) µm in the IVT-AFL-2W and IVT-AFL-4W groups, respectively. Overall, 51.1% of patients (IVT-AFL-2W, 43.5%; IVT-AFL-4W, 59.1%) achieved a treatment interval of 16 weeks between weeks 16 and 96. The safety profile of IVT-AFL was consistent with previous studies.
Conclusion
In treatment-naïve patients with PCV, IVT-AFL administered using two different T&E regimens improved and maintained functional and anatomic outcomes over 96 weeks while minimizing treatment burden.
Trial registration
ClinicalTrials.gov identifier, NCT02305238.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Although intravitreal anti-vascular endothelial growth factor (VEGF) therapy has been established as the standard of care for exudative age-related macular degeneration (AMD), the optimal treatment regimen for patients with polypoidal choroidal vasculopathy (PCV) requires further investigation. |
The ALTAIR PCV subgroup analysis explored the efficacy and safety of intravitreal aflibercept (IVT-AFL) administered using proactive, individualized treat-and-extend (T&E) regimens with 2- or 4-week adjustments over 96 weeks in the subgroup of patients with PCV. |
What was learned from this study? |
IVT-AFL administered to treatment-naïve patients with PCV using two different T&E regimens improved and maintained functional and anatomic outcomes over 96 weeks, with approximately half of patients achieving a treatment interval of 16 weeks. |
The results of this subgroup analysis further substantiate that proactive, individualized IVT-AFL T&E regimens can be used to optimize treatment outcomes in patients with PCV, while minimizing treatment burden. |
Introduction
The ALTAIR study demonstrated the efficacy and safety of proactive, individualized intravitreal aflibercept (IVT-AFL) treat-and-extend (T&E) regimens over the longer term (96 weeks), whereby the interval between injections (following three initial monthly doses) could be adjusted in 2-week (IVT-AFL-2W) or 4-week (IVT-AFL-4W) increments, based on visual and/or anatomic outcomes, in treatment-naïve patients with exudative age-related macular degeneration (AMD) in Japan [1]. Improvements in functional and anatomic outcomes were reported at week 52 in both treatment groups and were maintained over 96 weeks. Furthermore, a reduction in treatment burden using both IVT-AFL T&E regimens was noted, with more than 40% (IVT-AFL-2W, 42%; IVT-AFL-4W, 46%) of patients achieving a last treatment interval of 16 weeks up to week 96. ALTAIR included 36.6% patients with polypoidal choroidal vasculopathy (PCV), diagnosed based on the indocyanine green angiography (ICGA) findings at baseline under the investigator’s discretion; no reading center was involved. Alongside PLANET [2], the ALTAIR study is among the first to evaluate IVT-AFL T&E regimens in such a population.
PCV, which is considered to be a subtype of exudative AMD [3,4,5], is characterized by the presence of aneurysmal polypoidal lesions in the choroidal vasculature, involving serosanguineous pigment epithelial detachment [3]. In Asian populations, PCV is prevalent, with approximately 25–65% of Asian patients with exudative AMD reported to have PCV [5,6,7,8,9,10]; this subtype is also being increasingly recognized in white patients, with PCV being reported in 25% of patients of predominantly European ancestry with exudative AMD [11]. Disparity in the epidemiological and clinical characteristics, natural history, and treatment outcomes between patients with PCV and typical exudative AMD has been identified [5]. Although intravitreal anti-vascular endothelial growth factor (VEGF) therapy has been established as the standard of care for exudative AMD, the optimal treatment for patients with PCV requires further investigation [12].
Current treatment modalities for PCV include anti-VEGF monotherapy, photodynamic therapy (PDT) with verteporfin, and combination therapy with PDT and anti-VEGF therapy [2, 13]. The PLANET study demonstrated that IVT-AFL was efficacious in patients with PCV, and that the addition of rescue PDT showed no additional benefits [2, 14]. The adoption of anti-VEGF T&E regimens for the treatment of exudative AMD has been shown to maintain visual acuity while reducing treatment burden [15,16,17,18]. Previous studies assessing IVT-AFL T&E regimens in patients with PCV determined that it is an effective treatment option up to a maximum treatment interval of 12 weeks [19,20,21]; however, evidence for treatment intervals > 12 weeks has been limited and is only from retrospective studies [22, 23]. Furthermore, the optimum treatment regimen for polypoidal lesion closure and reduction of subretinal hemorrhage or other exudative changes over the long term is still unknown.
The present ALTAIR PCV subgroup analysis explored the efficacy and safety of IVT-AFL administered using T&E regimens over 96 weeks in the subgroup of patients with PCV. Unlike prior randomized controlled trials of IVT-AFL T&E regimens in such patients, treatment intervals could be extended to > 12 weeks, up to a maximum of 16 weeks, and adjusted in 4-week increments.
Methods
Study Design
This was a subgroup analysis of data from ALTAIR, a 96-week, prospective, randomized, open-label, phase 4 study (NCT02305238), in Japanese treatment-naïve patients with exudative AMD. ALTAIR was conducted at 41 study sites across Japan between December 2014 and November 2017, in accordance with the Declaration of Helsinki and the International Conference on Harmonisation guidelines E6: Good Clinical Practice. The protocol and any amendments were approved by the independent ethics committee or institutional review board at each study site. All enrolled patients provided written informed consent.
Patients
Treatment-naïve adults aged ≥ 50 years with exudative changes due to active subfoveal choroidal neovascularization (CNV) lesions secondary to AMD, including juxtafoveal lesions affecting the fovea that were evaluated using fluorescein angiography in the study eye, were included. Optical coherence tomography (OCT), fundus photography, and ICGA were also conducted for all patients at baseline. Patients had a best-corrected visual acuity (BCVA) of 73–25 Early Treatment Diabetic Retinopathy Study (ETDRS) letters (approximately 20/40–20/320 Snellen equivalent) in the study eye. Full details of the ALTAIR study population and inclusion/exclusion criteria have been reported previously [1].
This subgroup analysis reports the efficacy and safety of IVT-AFL administered using two different T&E regimens in patients with PCV in the ALTAIR full analysis set (FAS) and safety analysis set, respectively. PCV was diagnosed at baseline based on the ICGA findings under investigator discretion; no reading center was involved.
Interventions
The methodology of ALTAIR has been published previously, including criteria for shortening, maintaining, or extending the treatment interval [1]. Briefly, patients received three initial monthly doses of IVT-AFL 2 mg at baseline, week 4, and week 8. At week 16, patients received IVT-AFL and were then randomized 1:1 to two T&E dosing regimen arms: IVT-AFL-2W or IVT-AFL-4W. Randomization was stratified by baseline BCVA (< 55 and ≥ 55 ETDRS letters) and exudative AMD subtype (presence or absence of PCV, as assessed by the investigator). Treatment intervals were extended, maintained or shortened based on prespecified functional and anatomic criteria. The minimum and maximum treatment intervals were 8 and 16 weeks from week 16 to week 96. Safety evaluations were conducted at every treatment and evaluation visit, including the follow-up visit.
Study Endpoints
The primary endpoint of ALTAIR was the mean change in BCVA (ETDRS letters) from baseline to week 52. Here, we report the following outcomes, assessed at weeks 52 and 96, in the PCV subgroup: the mean change in BCVA and central retinal thickness (CRT), the proportion of patients who lost < 15 letters (defined as vision maintenance), the mean number of IVT-AFL injections, the proportion of patients who achieved and maintained treatment intervals up to 16 weeks, and the proportion of patients without fluid on OCT and polyp status on ICGA. The last treatment interval up to week 96 (the interval between the last two injections) is also reported. Safety analyses were also conducted.
Statistical Analysis
In this subgroup analysis, the FAS included all patients with PCV (as assessed by the investigator) from the ALTAIR FAS, and both prespecified and post hoc analyses were performed. Efficacy variables were summarized descriptively for the subgroup of patients with PCV. Patients who received ≥ one of the three initial monthly doses of IVT-AFL comprised the safety analysis set. Statistical evaluation was performed using Statistical Analysis Software v.9.2 or higher (SAS Institute, Cary, NC, USA).
Results
Patients
In total, 90 patients with PCV were included in the FAS. Baseline demographics and disease characteristics were relatively similar between the PCV and non-PCV subgroups (Table 1). Notably, the proportion of male patients, the proportion with occult CNV, and the presence of pigment epithelium detachment was relatively higher in the PCV subgroup. In patients with PCV, the mean [standard deviation (SD)] age was 74.1 (7.4; IVT-AFL-2W) and 73.5 (7.4; IVT-AFL-4W) years, mean baseline BCVA was 52.7 (13.6; IVT-AFL-2W) and 57.5 (9.0; IVT-AFL-4W) ETDRS letters, and mean baseline CRT was 400 (184; IVT-AFL-2W) and 372 (136; IVT-AFL-4W) µm.
Treatment Exposure
From baseline to week 96, patients received a mean (SD) of 10.0 (2.9) and 9.9 (2.5) injections in the IVT-AFL-2W and IVT-AFL-4W groups. From baseline to week 52, patients in the IVT-AFL-2W and IVT-AFL-4W groups received a mean (SD) of 7.1 (1.0) and 6.7 (1.1) injections, and, from week 52 to week 96, a mean of 3.4 (1.8) and 3.5 (1.4) injections. Up to week 96, 41.3% and 47.7% of patients achieved a last treatment interval of 16 weeks in the IVT-AFL-2W and IVT-AFL-4W groups (Supplemental Fig. 1).
A comparable proportion of patients met the criteria for treatment interval maintenance at least once in both groups [IVT-AFL-2W, 30.4% (n = 14); IVT-AFL-4W, 34.1% (n = 15)]. Similarly, the proportion of patients meeting shortening criteria at least once was comparable between groups [IVT-AFL-2W, 60.9% (n = 28); IVT-AFL-4W, 61.4% (n = 27)]. However, the total number of treatment intervals shortened and maintained was numerically higher in the IVT-AFL-2W group than in the IVT-AFL-4W group (115 vs. 105 treatment intervals shortened, and 37 vs. 32 treatment intervals maintained, respectively). The proportion of patients with at least one extension was higher in the IVT-AFL-4W group [84.1% (n = 37)] versus the IVT-AFL-2W group [71.7% (n = 33)].
Overall, between week 16 and week 96, the proportion of patients achieving a treatment interval of ≥ 12 weeks was 70.0% (60.9%, IVT-AFL-2W; 79.5%, IVT-AFL-4W), and 50.0% (50.0%, IVT-AFL-2W; 50.0%, IVT-AFL-4W) maintained a treatment interval of ≥ 12 weeks (extended to ≥ 12 weeks, and never shortened to < 12 weeks). Additionally, 51.1% (43.5%, IVT-AFL-2W; 59.1%, IVT-AFL-4W) achieved a treatment interval of 16 weeks between week 16 and week 96, and 43.3% (41.3%, IVT-AFL-2W; 45.5%, IVT-AFL-4W) maintained a treatment interval of 16 weeks (extended to 16 weeks and never shortened).
Efficacy
Functional Outcomes
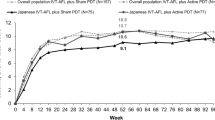
From baseline to week 52, patients with PCV showed improvement in mean (SD) BCVA of 52.7 (13.6) to 60.1 (18.5) letters [change from baseline: + 7.5 (14.7) letters] and 57.5 (9.0) to 65.6 (13.0) letters [change from baseline: + 8.2 (11.6) letters] in the IVT-AFL-2W and IVT-AFL-4W groups (Fig. 1).
Absolute BCVA for patients in the PCV subgroup between baseline and week 96. Full analysis set. Last observation carried forward. Boxesshow the IQR (25–75%). The center line of the box and “+” show median and mean values, respectively. The top and bottom of the vertical bars show the maximum and minimum values (where values were within the range of 1.5 IQR); the values that exceed the range of 1.5 IQR were defined as outliers and are shown outside the vertical bars as an “x.” Mean BCVA: IVT-AFL-2W: baseline, 52.7; week 4, 56.7; week 8, 59.3; week 16, 59.3; week 24, 60.2; week 32, 59.8; week 40, 60.1; week 48, 59.8; week 52, 60.1; week 56, 59.3; week 64, 60.0; week 72, 59.9; week 80, 59.3; week 88, 59.3; week 96, 56.3. IVT-AFL-4W: baseline, 57.5; week 4, 59.3; week 8, 62.8; week 16, 65.3; week 24, 65.9; week 32, 65.0; week 40, 64.8; week 48, 65.5; week 52, 65.6; week 56, 64.3; week 64, 64.6; week 72, 63.7; week 80, 63.8; week 88, 62.8; week 96, 62.3. 2W/4W 2-/4-week adjustment, BCVA best-corrected visual acuity, ETDRS Early Treatment Diabetic Retinopathy Study, IQR interquartile range, IVT-AFL intravitreal aflibercept, PCV polypoidal choroidal vasculopathy
Improvements in BCVA from baseline to week 52 were generally maintained up to week 80; however, there was a numerical decline in BCVA toward week 96 (Supplemental Fig. 2). From baseline to week 96, patients showed improvement in mean (SD) BCVA, from 52.7 (13.6) to 56.3 (21.1) letters [change from baseline: + 3.7 (18.5) letters] and 57.5 (9.0) to 62.3 (18.9) letters [change from baseline: + 4.9 (17.7) letters] in the IVT-AFL-2W and IVT-AFL-4W groups. At week 96, the mean absolute BCVA was numerically lower in the IVT-AFL-2W group (56.3 letters) than in the IVT-AFL-4W group (62.3 letters).
Four patients (patients 1–4) in the IVT-AFL-2W group and four patients (patients 5–8) in the IVT-AFL-4W group experienced at least moderate vision loss (defined as > 15-letter loss) between baseline and week 96 (Fig. 2). Between weeks 88 and 96, three patients (patients 1, 9, and 10) within the IVT-AFL-2W group experienced at least moderate vision loss (Supplemental Fig. 3).
Most patients (> 90%) maintained vision (< 15-letter loss) from baseline to week 96. At week 52, 95.7% and 97.7% of patients maintained vision, and at week 96, 91.3% and 90.9% of patients maintained vision in the IVT-AFL-2W and IVT-AFL-4W groups, respectively.
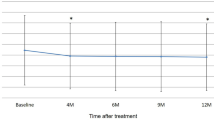
Anatomic Outcomes
From baseline to week 52, mean (SD) CRT decreased from 400 (184) µm to 251 (73) µm [mean (SD) change from baseline: − 153 (177) µm] and from 372 (136) µm to 260 (114) µm [mean (SD) change from baseline: − 112 (122) µm] in the IVT-AFL-2W and IVT-AFL-4W groups, respectively (Fig. 3; Supplemental Fig. 4). From baseline to week 96, mean (SD) CRT decreased from 400 (184) µm to 251 (67) µm [change from baseline: − 153 (179) µm] and from 372 (136) µm to 263 (91) µm [change from baseline: − 110 (112) µm] in the IVT-AFL-2W and IVT-AFL-4W groups, respectively.
Fluid
In the IVT-AFL-2W group, 60.9% of patients at week 52 and 60.9% at week 96 had no fluid on OCT. In the IVT-AFL-4W group, 75.0% of patients at week 52 and 70.5% at week 96 had no fluid on OCT.
Polyp Status
Investigators assessed ICGA findings for presence or absence of polyps. Cases of “probable” polyps were registered as “indefinite” in the data analysis. At week 52, complete polyp regression on ICGA (imputed by the last observation carried forward method) was reported in 47.8% and 52.3% of patients in the IVT-AFL-2W and IVT-AFL-4W groups, respectively (Supplemental Fig. 5). At week 96, complete polyp regression was reported in 56.5% and 50.0% of patients in the IVT-AFL-2W and IVT-AFL-4W groups, respectively.
Safety
An overview of the main safety data for patients in the PCV subgroup is shown in Table 2. Three patients in the IVT-AFL-2W group discontinued the study because of adverse events (AEs): renal failure, exudative AMD (worsening of the underlying disease), or AMD in the fellow eye. A relationship to the study drug, injection procedure, or protocol procedure was not reported in any of these cases. One patient in the IVT-AFL-4W group discontinued the study because of urticaria; this AE was related to the study drug. There was one case of vitreous hemorrhage reported in the IVT-AFL-2W group, but no cases in the IVT-AFL-4W group. Submacular hemorrhage as a treatment-emergent adverse event was not reported in either the IVT-AFL-2W or IVT-AFL-4W groups.
Of the three patients in the IVT-AFL-2W group who experienced at least moderate vision loss (> 15-letter loss) at the end of the study (weeks 88–96), two experienced AEs in the study eye: one patient experienced mild progression of cataract in the study eye between weeks 78 and 82 (patient 1), and one patient experienced mild dry eye in both eyes between weeks 80 and 88 (patient 9). No AEs were reported in the study eye of the remaining patient who experienced at least moderate vision loss at the end of the study (patient 10). A few retinal hemorrhage events were observed in these patients; however, none of these findings were reported as an AE or polyp rupture. One patient (patient 1) reported intraretinal bleeding at baseline and weeks 4 and 8, and one patient (patient 9) reported intraretinal bleeding throughout the course of the study. Neither finding was reported as an AE by the investigators. There were no hemorrhagic findings in the third patient (patient 10).
An Antiplatelet Trialists’ Collaboration event of intracranial hemorrhage occurred in one patient in the IVT-AFL-2W group, which was assessed by the investigator as being severe in intensity, as well as serious due to death as an outcome; it was unrelated to the study drug, injection procedure, or protocol procedure. Overall, no cases of endophthalmitis, intraocular inflammation, or retinal vasculitis were reported.
Discussion
This analysis has evaluated the efficacy and safety of IVT-AFL T&E regimens over 96 weeks in the subgroup of patients with PCV enrolled in the ALTAIR study, and is among the first to examine administering IVT-AFL in a T&E regimen in this population. The baseline BCVA and CRT values indicate the possibility of a harder-to-treat population in ALTAIR compared with prior studies in patients with PCV [14, 18, 21, 24,25,26,27,28]. Although there was no substantial difference between PCV and non-PCV patients in terms of baseline BCVA, it was numerically lower, and CRT was numerically higher, in PCV patients the IVT-AFL-2W group than in the IVT-AFL-4W group. Despite a 2-week adjustment in treatment intervals being more conservative than a 4-week adjustment, the proportion of patients with at least one shortening was comparable between groups (based on T&E regimen criteria). On the other hand, the proportion of patients with at least one extension was higher in the IVT-AFL-4W PCV subgroup, which conversely shows that a numerically higher number of patients stayed on an 8-week treatment interval throughout the study in the IVT-AFL-2W PCV subgroup compared with the IVT-AFL-4W PCV subgroup. Considering this, the possibility cannot be excluded that there was a small difference in the number of harder-to-treat patients between the IVT-AFL-2W and IVT-AFL-4W PCV subgroups. Nonetheless, in this subgroup of patients with PCV, improvements in functional and anatomic outcomes, as well as a reduction in treatment burden, were achieved with IVT-AFL in a T&E regimen with 2- or 4-week adjustments. The safety profile of IVT-AFL was consistent with previous studies.
Most patients (> 90%) maintained vision from baseline to week 96 in both treatment groups. A decrease in CRT from baseline to week 96 was also seen; however, variation was observed during the first year (Fig. 3), particularly in the IVT-AFL-4W group. This decrease in CRT observed in the IVT-AFL-4W group was numerically lower than in the IVT-AFL-2W group. This may be due to the ceiling effect (shown by the absolute mean CRT values in Supplemental Fig. 4), as baseline CRT was also numerically lower in the IVT-AFL-4W group.
Overall, 70% of patients achieved a treatment interval of ≥ 12 weeks between weeks 16 and 96, and 50% of these patients maintained a treatment interval of ≥ 12 weeks (never shortened to < 12 weeks). Furthermore, 51% achieved a treatment interval of 16 weeks between weeks 16 and 96, and 43% of these patients maintained a 16-week treatment interval (never shortened to < 16 weeks). Over 96 weeks, patients with PCV received a mean of 10.0 and 9.9 injections in the IVT-AFL-2W and IVT-AFL-4W groups, whereas, in the non-PCV ALTAIR population, the mean number of injections was 10.6 in both groups [29]. Previous studies have shown a lower mean number of injections in patients with PCV compared to those with typical exudative AMD [18], which is similar to our results. Notably, at week 96, complete polyp regression on ICGA (as assessed by the investigator) was reported in more than half of patients in the IVT-AFL-2W group (57%) and in half of patients in the IVT-AFL-4W group (50%). Similarly, in prior prospective studies evaluating polyp status in patients treated with IVT-AFL monotherapy, complete polyp regression rate on ICGA was reported at between 39 and 74% at year 1 [10, 21, 26,27,28], and 33% [10] and 67% [21] at year 2.
The results of this subgroup analysis, including the boxplot analysis (Fig. 1), support the fact that most patients with PCV can be treated effectively with IVT-AFL administered in a T&E regimen (even with 4-week adjustments and extension of the treatment interval to 16 weeks), highlighting the potential of such a regimen to reduce treatment burden in patients with PCV. Notably, no hemorrhagic adverse events (that can lead to severe vision loss) were reported in the IVT-AFL-4W group. Furthermore, submacular hemorrhage in patients with exudative AMD does not seem to be associated with extended treatment intervals, suggesting a low risk of submacular hemorrhage with a 4-week adjustment [30]. It is important to note that, as per the study protocol, when a patient in the IVT-AFL-4W group had a history of a treatment interval being shortened by 4 weeks during this study, the treatment interval would be extended by only 2 weeks. This may reduce the risk of further vision loss and provide an opportunity for vision recovery in eyes that were not optimized by IVT-AFL T&E treatment with 4-week adjustments.
Between weeks 88 and 96, three patients within the IVT-AFL-2W group experienced at least moderate vision loss (> 15-letter loss), and a numerical decline in BCVA toward week 96 was observed. This vision decline was not associated with polyp rupture, geographic/macular atrophy, non-response/resistance to IVT-AFL, or the T&E dosing regimen. Importantly, the retinal hemorrhage events observed in these patients were not reported as AEs or polyp rupture, which can occur in patients with PCV. Two of these patients reported AEs, cataract (patient 1), and dry eye (patient 9), and the substantial difference between mean and median BCVA values suggest that a small number of outliers in the PCV subgroup affected the mean absolute BCVA; however, the extent to which the AEs in these patients impacted vision decline was not specifically evaluated in this study, and other factors cannot be ruled out. In the IVT-AFL-4W group, eight patients lost ≥ 5 letters between weeks 88 and 96 without any remarkable AEs, which potentially caused the moderate vision loss observed in this group.
This analysis has several strengths. To the best of our knowledge, the ALTAIR PCV subgroup analysis is the first prospective longer-term study (96 weeks) to explore the efficacy of IVT-AFL T&E for patients with PCV starting directly after treatment initiation in year 1. Most prior studies have not included 4-week adjustment of treatment intervals or a maximum treatment interval of 16 weeks [19,20,21], and the only reports of treatment intervals > 12 weeks are from retrospective studies [22, 23]. Interval maintenance was also a unique feature of the ALTAIR study. There were limitations in this analysis that are worth consideration. No reading center was involved in the study; prespecified diagnosis of PCV by ICGA and determination of the next treatment interval were at the discretion of the investigators. The inclusion/exclusion criteria for the ALTAIR study do not include lesion size, unlike some studies assessing IVT-AFL T&E treatment in patients with PCV [14]. As the manifestation of PCV varies between individuals, additional data to describe the baseline state and severity of PCV in detail (e.g., the number and size of polyps, whether they were clustered or non-clustered) would be useful to more fully understand the results of this study; however, these data were not investigated in ALTAIR. There is also a lack of information on subfoveal choroidal thickness. It has been reported that change in subfoveal choroidal thickness after IVT-AFL treatment is related to visual and anatomic outcomes [31], and that differences in baseline subfoveal choroidal thickness might influence the number of injections needed, which may therefore explain the variation in treatment burden [19]. Furthermore, it should be acknowledged that the possibility remains that some patients may have experienced no recurrence after initial treatment.
Conclusions
IVT-AFL administered to treatment-naïve patients with PCV using two different T&E regimens, with a minimum treatment interval of 8 weeks and a maximum interval of 16 weeks, improved and maintained functional and anatomic outcomes over 96 weeks. Furthermore, treatment burden on patients was minimized, with approximately half of patients achieving a treatment interval of 16 weeks and a similar distribution of treatment intervals to that of the entire ALTAIR population. The results of this subgroup analysis further substantiate that proactive, individualized IVT-AFL T&E regimens can be used to optimize BCVA outcomes in patients with PCV while reducing treatment burden.
References
Ohji M, Takahashi K, Okada AA, et al. Efficacy and safety of intravitreal aflibercept treat-and-extend regimens in exudative age-related macular degeneration: 52- and 96-week findings from ALTAIR. Adv Ther. 2020;37(3):1173–87.
Lee WK, Iida T, Ogura Y, et al. Efficacy and safety of intravitreal aflibercept for polypoidal choroidal vasculopathy in the PLANET study: a randomized clinical trial. JAMA Ophthalmol. 2018;136(7):786–93.
Wong RL, Lai TY. Polypoidal choroidal vasculopathy: an update on therapeutic approaches. J Ophthalmic Vis Res. 2013;8(4):359–71.
Yannuzzi LA, Sorenson J, Spaide RF, Lipson B. Idiopathic polypoidal choroidal vasculopathy (IPCV). Retina (Philadelphia, PA). 1990;10(1):1–8.
Wong CW, Yanagi Y, Lee WK, et al. Age-related macular degeneration and polypoidal choroidal vasculopathy in Asians. Prog Retin Eye Res. 2016;53:107–39.
Laude A, Cackett PD, Vithana EN, et al. Polypoidal choroidal vasculopathy and neovascular age-related macular degeneration: same or different disease? Prog Retin Eye Res. 2009;29(1):19–29.
Kwok AK, Lai TY, Chan CW, Neoh EL, Lam DS. Polypoidal choroidal vasculopathy in Chinese patients. Br J Ophthalmol. 2002;86(8):892–7.
Byeon SH, Lee SC, Oh HS, Kim SS, Koh HJ, Kwon OW. Incidence and clinical patterns of polypoidal choroidal vasculopathy in Korean patients. Jpn J Ophthalmol. 2008;52(1):57–62.
Gomi F, Tano Y. Polypoidal choroidal vasculopathy and treatments. Curr Opin Ophthalmol. 2008;19(3):208–12.
Wong TY, Ogura Y, Lee WK, et al. Efficacy and safety of intravitreal aflibercept for polypoidal choroidal vasculopathy: 2-year results of the PLANET study. Am J Ophthalmol. 2019;204:80–9.
Kokame GT, deCarlo TE, Kaneko KN, Omizo JN, Lian R. Anti-vascular endothelial growth factor resistance in exudative macular degeneration and polypoidal choroidal vasculopathy. Ophthalmol Retin. 2019;3(9):744–52.
Cheung CMG, Lai TYY, Ruamviboonsuk P, et al. Polypoidal choroidal vasculopathy: definition, pathogenesis, diagnosis, and management. Ophthalmology. 2018;125(5):708–24.
Koh A, Lee WK, Chen LJ, et al. EVEREST study: efficacy and safety of verteporfin photodynamic therapy in combination with ranibizumab or alone versus ranibizumab monotherapy in patients with symptomatic macular polypoidal choroidal vasculopathy. Retina (Philadelphia, PA). 2012;32(8):1453–64.
Ogura Y, Lida T, Lee WK, et al. Efficacy and safety of intravitreal aflibercept for polypoidal choroidal vasculopathy: 96-week outcomes in the Japanese subgroup of the PLANET study. Jpn J Ophthalmol. 2021;65:344–53.
Yamamoto A, Okada AA, Nakayama M, Yoshida Y, Kobayashi H. One-year outcomes of a treat-and-extend regimen of Aflibercept for exudative age-related macular degeneration. Ophthalmologica. 2017;237(3):139–44.
Barthelmes D, Nguyen V, Daien V, et al. Two year outcomes of “treat and extend” intravitreal therapy using aflibercept preferentially for neovascular age-related macular degeneration. Retina (Philadelphia, PA). 2018;38(1):20–8.
Yamamoto A, Okada AA, Kano M, et al. One-year results of intravitreal aflibercept for polypoidal choroidal vasculopathy. Ophthalmology. 2015;122(9):1866–72.
Maruko I, Ogasawara M, Yamamoto A, et al. Two-year outcomes of treat-and-extend intravitreal aflibercept for exudative age-related macular degeneration: a prospective study. Ophthalmol Retin. 2020;4(8):767–76.
Morimoto M, Matsumoto H, Mimura K, Akiyama H. Two-year results of a treat-and-extend regimen with aflibercept for polypoidal choroidal vasculopathy. Graefes Arch Clin Exp Ophthalmol. 2017;255(10):1891–7.
Matsumoto H, Morimoto M, Mimura K, Ito A, Akiyama H. Treat-and-extend regimen with aflibercept for neovascular age-related macular degeneration. Ophthalmol Retin. 2018;2(5):462–8.
Sakamoto S, Takahashi H, Inoue Y, et al. Intravitreal aflibercept for exudative age-related macular degeneration with good visual acuity: 2-year results of a prospective study. Clin Ophthalmol. 2018;12:1137–47.
Morizane-Hosokawa M, Morizane Y, Kimura S, et al. Impact of polyp regression on 2-year outcomes of intravitreal aflibercept injections: a treat-and-extend regimen for polypoidal choroidal vasculopathy. Acta Med Okayama. 2018;72(4):379–85.
Tamachi T, Kohno T, Yamamoto M, et al. One-year results of a treat-and-extend regimen of intravitreal aflibercept for polypoidal choroidal vasculopathy. Ophthalmol Ther. 2020;9(4):1069–82.
Teo KYC, Jordan-Yu JM, Tan ACS, et al. Efficacy of a novel personalised aflibercept monotherapy regimen based on polypoidal lesion closure in participants with polypoidal choroidal vasculopathy. Br J Ophthalmol. 2021. https://doi.org/10.1136/bjophthalmol-2020-318354 (Online ahead of print).
Inoue M, Arakawa A, Yamane S, Kadonosono K. Short-term efficacy of intravitreal aflibercept in treatment-naive patients with polypoidal choroidal vasculopathy. Retina (Philadelphia, PA). 2014;34(11):2178–84.
Arakawa A, Inoue M, Sato S, Yamane S, Kadonosono K. Efficacy of intravitreal aflibercept injections for Japanese patients with polypoidal choroidal vasculopathy. Clin Ophthalmol. 2017;11:797–802.
Oishi A, Tsujikawa A, Yamashiro K, et al. One-year result of aflibercept treatment on age-related macular degeneration and predictive factors for visual outcome. Am J Ophthalmol. 2015;159(5):853-60.e1.
Oshima Y, Kimoto K, Yoshida N, et al. One-year outcomes following intravitreal aflibercept for polypoidal choroidal vasculopathy in Japanese patients: the APOLLO study. Ophthalmologica. 2017;238(3):163–71.
Ohji M, Okada A, Takahashi K, Kobayashi M, Terano Y. Intravitreal aflibercept treat-and-extend dosing for wet age-related macular degeneration: ALTAIR 96-week results. Asia-Pacific Vitreoretinal Society (APVRS) Meeting, Seoul, South Korea; 2018.
Matsunaga DR, Su D, Sioufi K, et al. The timing of large submacular hemorrhage secondary to age-related macular degeneration relative to anti-VEGF therapy. Ophthalmol Retin. 2021;5(4):342–7.
Koizumi H, Kano M, Yamamoto A, et al. Subfoveal choroidal thickness during aflibercept therapy for neovascular age-related macular degeneration twelve-month results. Ophthalmology. 2016;123(3):617–24.
Acknowledgements
The authors thank all the patients and investigators who participated in the ALTAIR study.
List of study Investigators Masahito Ohji, Tsukasa Hanemoto, Tatsushi Kaga, Takeya Kouno, Hirokuni Kitamei, Shinpei Sato, Kanji Takahashi, Ryoji Yanai, Eiichi Uchio, Kazunori Miyata, Yoshihiro Wakabayashi, Takatoshi Maeno, Tsutomu Yasukawa, Masayuki Horiguchi, Tetsuya Nishimura, Akiteru Kawahara, Yasuo Kurimoto, Kenichi Murai, Namie Kobayashi, Wataru Kimura, Eriko Matsushita, Tomohiro Iida, Kanako Yasuda, Masahiro Miura, Annabelle Ayame Okada, Ryusaburo Mori, Atsushi Sugiyama, Yasuo Ito, Daisaku Kimura, Kei Nakai, Chota Matsumoto, Shinobu Takeuchi, Kishiko Okoshi, Yoshihisa Nuno, Yohei Nomoto, Toshio Mori, Muneyasu Takeda, Noriko Yoshida, Mio Hosokawa, Kohei Sonoda.
Funding
The ALTAIR study was sponsored by Bayer Yakuhin Ltd. This post hoc analysis was funded by Bayer Consumer Care AG, Pharmaceuticals, Basel, Switzerland. The journal’s Rapid Service and Open Access Fees were funded by Bayer Consumer Care AG.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
All named authors (Annabelle A. Okada, Kanji Takahashi, Masahito Ohji, SungChul Charles Moon, Tobias Machewitz and Koji Sasaki) contributed to the design; data acquisition, analysis, and interpretation; and preparation and final review of the manuscript. All named authors also approved the manuscript for submission.
Medical Writing/Editorial Assistance
Medical writing and editorial support for the preparation of this manuscript, under the direction of the authors, was provided by Charlotte Head, ApotheCom (London), and funded by Bayer Consumer Care AG, Basel, Switzerland, in accordance with Good Publication Practice (GPP3) guidance (Ann Intern Med 2015;163:461–464).
Disclosures
Annabelle A. Okada has received research funds from Alcon Pharma Japan, Bayer Japan, Kowa, and Mitsubishi Tanabe Pharma; consultant fees from Apellis Pharmaceuticals Inc., Bayer Healthcare, Bayer Japan, Biocon Biologics, Chugai, HOYA, Kowa, Novartis Japan, and Novartis Pharma; and lecture fees from AbbVie Japan, Alcon Pharma Japan, Allergan Japan, Bayer Japan, Kowa, Mitsubishi Tanabe Pharma, Novartis Japan, Otsuka Pharmaceutical, Pfizer Japan, Santen Pharmaceutical, and Senju Pharmaceutical. Kanji Takahashi has received grants and personal fees from Alcon Japan, Allergan Japan, Bayer Yakuhin, Ltd. (Japan), HOYA, Kowa, Kyowa Kirin Co., Ltd., Nitto Medic, Novartis Pharma, Ono, Otsuka Pharmaceuticals, Santen Pharmaceuticals Co., Ltd., and Senju Pharmaceutical Co., Ltd., during the conduct of the study. Masahito Ohji has received grants and personal fees from AbbVie Japan, Inc., Alcon Pharma K.K. (Japan), Allergan, B.L.J. Ltd., Bayer Yakuhin, Ltd. (Japan), Chengdu Kanghong Biotechnology Co., Ltd., Chugai, HOYA, Kowa, Novartis Pharma K.K., Otsuka Pharmaceuticals, Pfizer Pharmaceuticals K.K, Santen Pharmaceuticals Co., Ltd., Senju Pharmaceutical Co., Ltd., and Topcon, during the conduct of the study. SungChul Charles Moon and Tobias Machewitz are employees of Bayer AG, Berlin, Germany. Koji Sasaki is an employee of Bayer Yakuhin Ltd., Japan.
Compliance with Ethics Guidelines
The ALTAIR study was conducted at 41 study sites across Japan between December 2014 and November 2017, in accordance with the Declaration of Helsinki and the International Conference on Harmonization guidelines E6: Good Clinical Practice. The protocol and any amendments were approved by the independent ethics committee or institutional review board at each study site (see Supplementary Material). There was no central IRB involved in the study and the protocol was reviewed and approved by the IRB at each participating center. All enrolled patients provided written informed consent. A list of investigators who participated in the study is provided in the supplementary material.
Data Availability
Availability of the data underlying this publication will be determined later according to Bayer’s commitment to the EFPIA/PhRMA “Principles for responsible clinical trial data sharing.” This pertains to scope, time point and process of data access.
As such, Bayer commits to sharing upon request from qualified scientific and medical researchers patient-level clinical trial data, study-level clinical trial data, and protocols from clinical trials in patients for medicines and indications approved in the United States (US) and European Union (EU) as necessary for conducting legitimate research. This applies to data on new medicines and indications that have been approved by the EU and US regulatory agencies on or after January 01, 2014.
Interested researchers can use http://www.clinicalstudydatarequest.com to request access to anonymized patient-level data and supporting documents from clinical studies to conduct further research that can help advance medical science or improve patient care. Information on the Bayer criteria for listing studies and other relevant information is provided in the study sponsors section of the portal. Data access will be granted to anonymized patient-level data, protocols and clinical study reports after approval by an independent scientific review panel. Bayer is not involved in the decisions made by the independent review panel. Bayer will take all necessary measures to ensure that patient privacy is safeguarded.
Prior Presentation
This study was presented at the 57th Annual Meeting of Japanese Retina and Vitreous Society (JRVS) Congress, December 7–9, 2018, Kyoto, Japan, and the 12th Asia-Pacific Vitreo-Retina Society (APVRS) Congress, December 14–16, 2018, Seoul, Korea.
Author information
Authors and Affiliations
Consortia
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visithttp://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Okada, A.A., Takahashi, K., Ohji, M. et al. Efficacy and Safety of Intravitreal Aflibercept Treat-and-Extend Regimens in the ALTAIR Study: 96-Week Outcomes in the Polypoidal Choroidal Vasculopathy Subgroup. Adv Ther 39, 2984–2998 (2022). https://doi.org/10.1007/s12325-022-02162-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-022-02162-w