Abstract
Introduction
Insulin degludec/insulin aspart (IDegAsp) provides effective glycaemic control with an acceptable safety profile in Japanese patients with diabetes in randomised clinical trials. This post-marketing surveillance study assessed long-term safety and clinical outcomes with IDegAsp in a Japanese real-world setting.
Methods
Multicentre, prospective, observational, open-label, single-arm study of Japanese patients with diabetes requiring insulin therapy, who had switched to IDegAsp at their treating physician’s discretion in clinical practice. One year after initiating IDegAsp, incidence of adverse events (AEs [primary endpoint]), serious AEs, adverse drug reactions (ADRs), and severe hypoglycaemia (secondary safety endpoints) were assessed in the safety analysis set (SAS). Secondary effectiveness endpoints were change from baseline in glycated haemoglobin (HbA1c) and fasting plasma glucose (FPG) in the effectiveness analysis set (EAS).
Results
Overall, 1321 patients were included (SAS, n = 1321; EAS, n = 1285); 4.2% with type 1 diabetes, 95.2% with type 2 diabetes, 0.7% with other/unknown diabetes type. In total, 204 AEs were reported in 132 patients (10.0% of the SAS), at a rate [95% confidence interval (CI)] of 16.2 events/100 patient-years of exposure (PYE) [14.0; 18.4]. By preferred term, ‘hypoglycaemia’ was the most frequent AE (45 events in 31 patients [2.3%]; rate [95% CI] 3.6 events/100 PYE [2.5; 4.6]). Serious AEs occurred in 4.2% of patients (rate [95% CI] 5.7 events/100 PYE [4.4; 7.0]), and ADRs in 3.1% (rate [95% CI] 4.6 reactions/100 PYE [3.4; 5.8]). Six events of severe hypoglycaemia were reported in five patients (0.4%; rate [95% CI] 0.5 events/100 PYE [0.1; 0.9]). Change from baseline to 1 year was − 0.51% and − 32.1 mg/dL for HbA1c and FPG, respectively (P < 0.0001 for both).
Conclusion
In Japanese patients with diabetes, initiation of IDegAsp in real-world clinical practice was well tolerated, with no new safety signals, and associated with improved glycaemic control after 1 year.
Trial Registration
ClinicalTrials.gov identifier, NCT02821052.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Randomised controlled trials have shown that insulin degludec/insulin aspart (IDegAsp) is a well-tolerated and effective therapy for diabetes in Japanese patients, with an acceptable safety profile in line with that observed in global populations. |
However, long-term, real-world safety data are lacking; a post-marketing surveillance study was planned in Japan prior to the launch of IDegAsp in 2015. |
What was learned from this study? |
In a real-world setting, IDegAsp was well tolerated, with no unexpected safety or tolerability concerns, over long-term follow-up in this observational study of clinical practice. |
The initiation of IDegAsp in clinical practice was associated with durable improvements in glycaemic control. |
Introduction
The prevalence of diabetes is increasing in Japan and, in 2019, over 4.9 million people older than 65 years of age were diagnosed with type 1 diabetes (T1D) or type 2 diabetes (T2D) [1]. The rising prevalence is predominantly driven by the increasing prevalence of T2D, and is generally considered to be multifactorial, but attributed in part to lifestyle changes, increasing prevalence of obesity, and an ageing population.
Notably, Japanese patients with diabetes have distinct characteristics from Caucasian populations, specifically among those with T2D. Japanese patients with T2D are more likely to be diagnosed at a younger age, and at a lower body mass index [2, 3]. Asian patients are likely to have lower levels of insulin resistance and greater impairment of insulin secretion relative to patients globally [3]. In light of this, and given the high carbohydrate content of the typical Japanese diet, post-prandial glycaemia is an important consideration in this group. Consequently, the initiation and intensification of insulin therapy are to be taken into careful consideration for Japanese patients with diabetes, to achieve glycaemic targets by targeting both fasting and post-prandial glucose.
However, there are perceived barriers to the use of insulin in Japan, which can result in treatment inertia [4, 5]; these may include the complexity of regimens, in particular those with multiple daily injections; side effects such as hypoglycaemia or weight gain; fear of injections by patients; and healthcare professionals’ perception that adherence is poor [4]. Additionally, the large proportion of elderly patients with diabetes in Japan may amplify these barriers in typical Japanese clinical practice [6]. Therapeutic options with properties that might help to overcome these barriers are therefore an important unmet need in diabetes care.
Insulin degludec/insulin aspart (IDegAsp, [Ryzodeg®, Novo Nordisk, Bagsværd, Denmark]) is a fixed-ratio co-formulation of insulin degludec, a basal insulin with an ultra-long duration of action, and the rapid-acting insulin, insulin aspart [7]. At steady state, IDegAsp offers clear separation of the prandial and basal components’ action, addressing both fasting and post-prandial glycaemia with a single injection [7]. IDegAsp has been extensively investigated in international populations in a global programme of clinical trials, establishing the clinical efficacy of IDegAsp in improving glycaemic control in T1D and a broad spectrum of patients with T2D, with an acceptable safety and tolerability profile in line with its component products [8,9,10,11,12]. IDegAsp was licensed for the treatment of diabetes in adults, adolescents, and children of ≥ 2 years of age in 2013 in Europe [13], and to improve glycaemic control in patients aged ≥ 1 year old with diabetes by the US Food and Drug Administration in 2015 [14].
The efficacy of IDegAsp in Japanese patient populations with diabetes has been assessed through a number of randomised controlled trials (RCTs) [15,16,17,18]. The results of these trials have shown that IDegAsp is associated with significant improvements in glycated haemoglobin (HbA1c) in insulin-naïve patients with T2D versus insulin glargine [15], and non-inferior glycaemic control in insulin-experienced patients with T2D versus biphasic insulin aspart 30 [16]. Furthermore, the safety findings of these trials indicate that the use of IDegAsp in Japanese patients has a similar safety and tolerability profile to that observed in the global RCTs, with no new signals identified [15, 16]. On this basis, IDegAsp was granted approval in Japan in 2012 for the treatment of patients with diabetes requiring insulin, and launched in December 2015 [19]. However, long-term safety data in Japanese patients are still lacking, and this post-marketing surveillance study was planned to investigate outcomes over a longer-term follow-up, as part of the approved drug re-examination period in Japan.
This post-marketing surveillance study was undertaken to assess long-term safety outcomes over 1 year among patients with diabetes mellitus initiated on IDegAsp in clinical practice; long-term clinical outcomes associated with the use of IDegAsp were assessed as a secondary outcome.
Methods
This was a prospective, observational, open-label, single-arm study, conducted between July 2016 and November 2018 at 157 study sites across Japan (Supplementary Material Fig. S1).
Inclusion and Exclusion Criteria
Patients were eligible for inclusion if they had previously been diagnosed with diabetes and required insulin therapy, regardless of age or gender. The decision to initiate IDegAsp was made by the treating physician in clinical practice, prior to enrolment in the study. Patients who had previously been treated with IDegAsp were not included in the study, and patients could be withdrawn at any time as a result of withdrawn consent, discontinuation of study medication, or the treating physician’s concern about safety. A full list of inclusion, exclusion, and withdrawal criteria can be found in Supplementary Material Table S1.
Treatment
Patients were treated with IDegAsp according to clinical practice at the discretion of their treating physician, and in accordance with the IDegAsp package insert [20]; this included the starting dose of IDegAsp and any subsequent dose adjustments. Additional visits or assessments were not undertaken as part of the study. Diet and exercise therapy, and concomitant medications, were initiated, changed, or discontinued at the treating physician’s discretion. Adherence to treatment, after initiation of IDegAsp, was defined at the physician’s discretion as excellent (≥ 90% compliant), good (50–90% compliant), poor (10–50% compliant), or no compliance (≤ 10% compliant).
Study Populations
Two study populations for analysis were defined: the safety analysis set (SAS) and the effectiveness analysis set (EAS). The SAS comprised all patients who received ≥ 1 dose of IDegAsp during the study period and the EAS comprised all patients from the SAS with ≥ 1 post-baseline measurement of either HbA1c or fasting plasma glucose (FPG) (both could include patients who withdrew from the study). Patients with other types of diabetes (not categorised as either T1D or T2D) were included in the analyses and contributed to the ‘overall’ data, but to neither diabetes type alone.
Compliance with Ethics Guidelines
The study protocol was approved by the central Institutional Review Board (IRB) Japan Conference of Clinical Research, or at participating study sites. The study was conducted in accordance with the Declaration of Helsinki, 1964, and its later amendments, and the Pharmaceutical and Medical Devices Agency Good Post-Marketing Study Practice (GPSP) guidance. All patients provided informed consent for participation.
Endpoints
Primary and secondary safety endpoints were assessed within the SAS; secondary effectiveness and clinical outcome assessments were analysed in the EAS. Pre-specified sub-analyses by diabetes type (T1D or T2D) and age group (< 65, ≥ 65 to < 75, or ≥ 75 years old), and sub-analyses for patients with renal impairment were also conducted for selected endpoints. Renal impairment was defined as mild (creatine clearance rate [CCR] ≥ 50 to ≤ 80 mL/min), moderate (CCR ≥ 30 to < 50 mL/min), or severe (CCR < 30 mL/min) at baseline.
Primary and Secondary Safety Endpoints
The primary safety endpoint was the incidence of adverse events (AEs) occurring within 1 year of initiating treatment. AEs were defined as any untoward medical occurrence in a patient administered IDegAsp, whether it was related to IDegAsp or not.
Secondary safety endpoints included the incidence over 1 year after the initiation of IDegAsp of the following events in the SAS: serious adverse events (SAEs), adverse drug reactions (ADRs), serious ADRs (SADRs), severe hypoglycaemic episodes, and serious allergic reactions (systemic or localised, including injection-site reactions). ADRs were defined as any untoward medical occurrence in a patient administered IDegAsp where a causal relationship between IDegAsp and the occurrence was suspected. Causality was based on the judgement of the treating physician or the study sponsor, Novo Nordisk. Hypoglycaemia was judged at the physician’s discretion and was based on presenting symptoms, self-measured or laboratory-measured blood glucose levels, or continuous glucose monitoring according to the definition of hypoglycaemia as published in the Treatment Guide for Diabetes by the Japan Diabetes Society. Severe hypoglycaemia was defined in this study as an episode requiring the assistance of another person to actively administer carbohydrate, glucagon, or other resuscitative actions. SAEs and SADRs were defined as those resulting in any of the following outcomes: death, a life-threatening experience, in-patient hospitalisation or prolongation of an existing hospitalisation, a persistent or significant disability or incapacity, a congenital anomaly or birth defect, or when an AE may have jeopardised the patient or required medical and/or surgical intervention to prevent one of the outcomes listed previously, on the basis of appropriate medical judgement.
Secondary Effectiveness and Clinical Outcome Assessment Endpoints
The following secondary effectiveness endpoints were all assessed (measured by local laboratory) after 1 year of treatment in the EAS: change from baseline to 1 year after initiation of IDegAsp in HbA1c and FPG; responder endpoints for HbA1c < 6.0%, < 7.0%, and < 8.0%; and composite responder endpoints for HbA1c < 6.0%, < 7.0%, and < 8.0%, without severe hypoglycaemic episodes.
Statistical Analyses
The study sample size of 1000 patients completing 1 year of treatment was agreed with the Pharmaceuticals and Medical Devices Agency (PMDA); the aim to enrol 1250 patients was based on an assumed drop-out rate of 20%, i.e. 250 patients who did not complete 1 year of treatment with IDegAsp and the study. Electronic data collection was carried out in ADDIN (INTAGE Healthcare Inc., Tokyo, Japan) and data analysis using SAS version 9.4 (SAS Institute, Cary, NC, USA).
Safety endpoints were summarised descriptively by system organ class (SOC) or preferred term (PT), as the number of patients with at least one event (n), the percentage of patients with at least one event (%), the number of events (E), and the rate per 100 person-years of exposure (PYE, [R]), with 95% confidence intervals (CIs). AEs and ADRs were coded using the most recent version of the Medical Dictionary for Regulatory Activities (MedDRA) coding and MedDRA/J version 22.0. Concomitant medications were coded using the Medicinal Drug Name Data File.
Repeated measurements for effectiveness endpoints (i.e. HbA1c or FPG) were summarised descriptively at each visit using observed data without any imputation for missing data. Available data at each visit or time point were used; not all participants had data available at each visit. For patients who discontinued the study medication or withdrew from the study, available data from time points prior to discontinuation or withdrawal were used in the effectiveness analyses. Changes from baseline in HbA1c and FPG were analysed using a paired t test in patients with data available at end of study (EOS) (i.e. who had not discontinued the study medication or withdrawn from the study during follow-up). All results were interpreted in a descriptive manner.
Results
Patient Disposition
Overall, 1355 patients were enrolled across the 157 participating study sites; electronic case report forms were completed for 1331 patients (Fig. 1). Altogether, 10 patients were excluded from the SAS (n = 1321); reasons for exclusion are provided in Fig. 1. In total, 1285 patients had sufficient data to be included in the EAS, of whom, at 1 year, 973 had a recorded HbA1c measurement and 319 had a measurement for FPG. Over 1 year of treatment, 17.4% (n = 230) of patients in the SAS discontinued the study. Reasons for discontinuation included not attending visits, changing hospital, deciding to discontinue, symptoms improving, lack of efficacy, and AEs. Of the patients in the SAS, 2.7% (n = 36) discontinued the study because of AEs.
Baseline characteristics of patients in the SAS are shown overall and by diabetes type in Table 1. Overall, 95.2% of patients in the SAS had T2D, 4.2% T1D, and 0.7% other or unknown diabetes type (nine patients had been diagnosed with a type of diabetes other than T1D or T2D). Mean (standard deviation [SD]) age among the SAS was 67.5 years (12.6), duration of diabetes was 16.8 years (10.0), and HbA1c was 8.5% (1.8); 55.6% were male. No paediatric patients were enrolled in the study; 446 patients (33.8% of the SAS) were aged < 65 years, 446 (33.8%) were aged ≥ 65 to < 75 years, and 428 (32.4%) were aged ≥ 75 years. In total, 502 patients had renal impairment at baseline. The most common reason for initiating IDegAsp was ‘to improve glycaemic control’ in both patients with T1D and T2D (65.5% and 87.7% of the SAS, respectively). Diabetes-related complications were recorded at baseline but only reported as an AE if new onset or if symptoms became exacerbated; at baseline 665 patients (50.3%) in the SAS reported microangiopathy.
IDegAsp Dosing and Adherence
At baseline, more patients were administered IDegAsp once daily (n = 762) compared with twice daily (n = 549). At 1 year, 560 patients were taking IDegAsp once daily, compared with 492 taking IDegAsp twice daily. Most patients reported excellent adherence (78.5% of the SAS [defined as ≥ 90% compliance]) or good adherence (19.3% [defined as 50–90% compliance]) to their IDegAsp regimen during the first month from baseline; at 7–12 months, this was 68.0% and 28.2%, respectively. The mean (SD) daily total insulin dose at baseline was 9.0 U (14.0 [units] U); by 1 year after initiating IDegAsp, the mean (SD) change from baseline in total daily insulin dose was 11.3 U (14.2 U).
Primary Outcome
In total, 204 AEs were reported in 132 patients, representing 10.0% of patients in the SAS. AEs occurred at a rate (95% CI) of 16.2 events per 100 PYE [14.0; 18.4] (Table 2). The most frequently reported AEs by SOC were ‘metabolism and nutrition disorders’, ‘infections and infestations’, and ‘vascular disorders’. By PT, ‘hypoglycaemia’ was the most frequently reported AE, with 45 events occurring in 31 patients (2.3% of the SAS), a rate (95% CI) of 3.6 events per 100 PYE (2.5; 4.6). ‘Hypertension’ and ‘pneumonia’ were the next most common AEs, with 11 events occurring in 11 patients (0.8%, rate [95% CI] 0.9 [0.4; 1.4]), and six events in six patients (0.5% of the SAS, rate [95% CI] 0.5 [0.1; 0.9]), respectively. Of the 204 AEs reported, 58 had a determined causality to IDegAsp.
Patients with T1D reported a numerically higher rate of AEs (rate [95% CI], 20.9 per 100 PYE [8.5; 33.2]) compared with patients with T2D (rate [95% CI], 15.7 per 100 PYE [13.4; 17.9]); however, the overall incidences of AEs were low, with events occurring in 14.5% and 9.6% of these subgroups, respectively (Table 2). The most commonly reported AEs by SOC and PT in both groups were consistent with the overall study population.
Patients aged ≥ 75 years experienced the highest rate (95% CI) of AEs, at 24.8 events per 100 PYE (19.9; 29.7), compared with 11.3 (8.1; 14.5) and 13.2 (9.7; 16.6) events per 100 PYE in the ≥ 65 to < 75 years, and < 65 years groups, respectively (Supplementary Material Table S2). The most frequently reported AEs by SOC and PT were broadly consistent across age groups.
Secondary Safety Outcomes
SAEs
Overall, 72 SAEs were reported in 56 patients (4.2% of the SAS), at a rate (95% CI) of 5.7 events per 100 PYE (4.4; 7.0) (Table 3). ‘Neoplasms benign, malignant, and unspecified (including cysts and polyps)’ were the most frequently reported SAEs by SOC. The next most commonly observed SAEs by SOC were ‘cardiac disorders’ and ‘infections and infestations’. The most commonly reported SAE by PT was ‘pneumonia’, with five SAEs in five patients (0.4% of the SAS), at a rate (95% CI) of 0.4 per 100 PYE (0.0; 0.7). Three SAEs occurred in a total of three patients (0.2% of the SAS) for both ‘pancreatic carcinoma’ and ‘acute myocardial infarction’, respectively, both at a rate (95% CI) of 0.2 (0.0; 0.5). Two patients experienced ‘inadequate diabetes mellitus control’, and two patients died (0.2% of the SAS, rate [95% CI] 0.2 [0.0; 0.4] for both). Rates (95% CI) of SAEs were 5.7 (0.0; 12.1) and 5.3 (4.0; 6.6) events per 100 PYE in patients with T1D and T2D, respectively; ‘neoplasms’, ‘cardiac disorders’, and ‘metabolic and nutritional disorders’ were reported with equal frequency in patients with T1D, while ‘neoplasms’ were most frequently reported in patients with T2D.
ADRs
Overall, 58 ADRs were reported in 41 patients (3.1% of the SAS), occurring at a rate (95% CI) of 4.6 reactions per 100 PYE (3.4; 5.8) (Table 4). The most commonly reported ADRs by SOC were ‘metabolism and nutrition disorders’, followed by ‘general disorders and administration-site conditions’. The rate of ADRs (95% CI) was higher in patients with T1D (11.4 reactions per 100 PYE [2.3; 20.5]) than T2D (4.2 reactions per 100 PYE [3.1; 5.4]), driven in part by a higher rate of hypoglycaemia (7.6 versus 3.4 reactions per 100 PYE, respectively). The incidence of ADRs was highest in patients aged ≥ 75 years (3.7% of this subgroup) versus those aged ≥ 65 to < 75 years (2.9%) or < 65 years (2.7%); rates (95% CI) of ADRs were also higher, at 7.8 (5.0; 10.5), 3.2 (1.5; 4.9), and 3.1 (1.4; 4.7) reactions per 100 PYE, respectively (Supplementary Material Table S3). ‘Hypoglycaemia’ was the most common ADR by PT, with 45 reactions reported in 31 patients (2.3% of the SAS), at a rate (95% CI) of 3.6 reactions per 100 PYE (2.5; 4.6), and this was consistent across age groups and diabetes types. Among 502 patients with renal impairment, 24 ADRs occurred in 20 patients (4.0% of this subgroup), and these were broadly consistent by SOC with the overall study population.
SADRs
As shown in Table 5, over 1 year of treatment, 10 SADRs were reported in nine patients (0.7% of the SAS), with an overall rate (95% CI) of 0.8 per 100 PYE (0.3; 1.3). The most frequently reported SADRs by SOC were ‘metabolism and nutrition disorders’; this was followed by ‘general disorders and administration-site conditions’. ‘Hypoglycaemia’, ‘inadequate diabetes mellitus control’, and ‘death’ were the most common SADRs by PT, and each occurred in two patients (0.2% of the SAS), respectively. The numerical rate (95% CI) of SADRs was higher in patients with T1D (1.9 per 100 PYE [0.0; 5.6]) versus T2D (0.7 per 100 PYE [0.2; 1.1]), but this was based on one reaction in one patient in the former group, compared with eight reactions in seven patients in the latter group.
Hypoglycaemia
Hypoglycaemic episodes in the SAS occurred with 46 events in 32 patients (2.4% of the SAS), at a rate (95% CI) of 3.7 per 100 PYE (2.6; 4.7) (Supplementary Material Table S4). Rates (95% CI) of hypoglycaemia were higher in patients with T1D (7.6 per 100 PYE [0.2; 15.0]) versus T2D (3.5 per 100 PYE [2.4; 4.6]), and in patients ≥ 75 years old (6.5 per 100 PYE [4.0; 9.0]) compared with younger patients. Severe hypoglycaemic episodes were uncommon, with six events occurring in five patients (0.4% of the SAS), all with T2D (Supplementary Material Table S4). The overall rate was 0.5 per 100 PYE [0.1; 0.9]); severe episodes were most common in patients aged ≥ 75 years, with a rate (95% CI) of 1.3 events per 100 PYE (0.2; 2.3) (Supplementary Material Table S4). Two nocturnal hypoglycaemic events were reported in two patients with T2D. One event occurred in a patient aged < 65 years and one in a patient aged ≥ 75 years.
Serious Allergic Reactions
No serious allergic reactions were reported within the study.
AEs of Special Interest
There were 20 reported patient deaths overall, as an outcome of 22 AEs, three of which (0.2% of the SAS) were not judged to be ‘unlikely’ to be related to the study product. In total, 13 patients reported neoplasm AEs; all were judged ‘unlikely’ to be related to the study product. Oedema AEs occurred in four patients, all of which were judged ‘unlikely’ to be related to the study product. No patients were pregnant at baseline, or reported a pregnancy during the study.
Secondary Effectiveness Outcomes
Change from Baseline in HbA1c
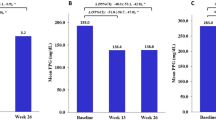
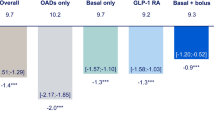
Of the patients in the EAS (n = 1285), 973 remained in the study after 1 year and had measurements of HbA1c available at baseline and at 1 year. Treatment initiation with IDegAsp was associated with a significant change from baseline in HbA1c after 1 year of − 0.51% (n = 973, P < 0.0001). Mean HbA1c over 1 year is shown in Fig. 2a. A trend towards reduction in HbA1c was also seen at 3 months (− 0.50%, n = 1084 [significance not tested]), as was a statistically significant reduction at 6 months (− 0.50%, n = 1073, P < 0.0001).
a Change from baseline in HbA1c, overall and by diabetes type, 1 year after initiation of IDegAsp; b Mean HbA1c (%) by diabetes type over 1 year of treatment. Effectiveness analysis set. Data are observed means (± SEM in a). Data were included for patients with an available HbA1c measurement at a given time point; missing data were not imputed. HbA1c glycated haemoglobin, n number of patients with an HbA1c measurement at time point, T1D type 1 diabetes, T2D type 2 diabetes, SEM standard error of the mean
The reductions in HbA1c were significant for patients with T2D (− 0.52%, P < 0.0001), but not for patients with T1D (− 0.27%, P = 0.1105) at 1 year (Fig. 2b). This was consistent across patients aged < 65 years and ≥ 65 to < 75 years, with reductions of − 0.57% and − 0.56%, respectively; slightly smaller reductions were seen in patients aged ≥ 75 years (− 0.39% [P < 0.0001 for all age groups]).
Among patients with renal impairment, changes in HbA1c were slightly greater at 6 months and 1 year (− 0.57% [n = 412] and − 0.58% [n = 379], respectively) compared with patients without renal impairment (− 0.46% [n = 638] and − 0.48% [n = 572], respectively); changes were significant at 6 months and 1 year in both groups (P < 0.0001 for all).
HbA1c at baseline was 8.48% (n = 236) and 8.42% (n = 1240) for patients receiving metformin > 750 mg/day and for all patients in the EAS, respectively. The change from baseline in HbA1c at 1 year in patients receiving metformin > 750 mg/day at least once during the study period was − 0.49% (n = 199, [no statistical analysis]). This was similar to the change from baseline in HbA1c after 1 year of − 0.51% (n = 973, P < 0.0001) for all patients. No other analysis was performed for the effect of concomitant drugs on HbA1c.
Change from Baseline in FPG
There were significant changes from baseline in FPG at 6 months (n = 415) and 1 year (n = 319) in the EAS (− 28.1 mg/dL and − 32.1 mg/dL, respectively, P < 0.0001 for both [Supplementary Material Fig. S2]). This was also observed among patients with T2D [n = 304] (− 31.9 mg/dL at 1 year, P < 0.0001); there was a numerical trend towards reduced FPG in patients with T1D [n = 14], but this was not significant (− 36.7 mg/dL at 1 year, P > 0.05 [Supplementary Material Fig. S2]). Patients in all age groups experienced significant reductions in FPG: − 41.0 mg/dL for those aged < 65 years (n = 102), − 27.5 mg/dL for those aged ≥ 65 to < 75 years (n = 115), and − 28.6 mg/dL for those aged ≥ 75 years (n = 102 [P < 0.001 for all age groups]).
Among patients with renal impairment, changes in FPG were − 27.2 mg/dL [n = 142] and − 29.3 mg/dL [n = 114] at 6 months and 1 year, compared with − 29.2 mg/dL [n = 269] and − 33.9 mg/dL [n = 204], respectively, for patients without impairment. The change from baseline was significant at 6 months and 1 year for patients with and without renal impairment (P < 0.05 for all comparisons).
Responder Endpoints for HbA1c Targets
In total, among the EAS, 22.7% (n = 225) of patients at 1 year achieved the Japan Diabetes Society (JDS) target HbA1c of < 7% to prevent complications (Supplementary Material Fig. S3) [21]. Overall, 1.3% (n = 13) of the EAS achieved the JDS target of HbA1c < 6% for normal glycaemia, and 65.9% (n = 654) achieved the JDS HbA1c target of < 8% for people among whom treatment intensification is considered difficult (Supplementary Material Fig. S3) [21]. More patients with T2D than with T1D achieved the JDS HbA1c < 7% target (23.1% versus 12.5% of the EAS, respectively [Supplementary Material Fig. S3]).
Composite Endpoints for HbA1c < 6%, < 7%, and 8%, Respectively, and Without Severe Hypoglycaemia
Among patients in the EAS, 22.6% achieved HbA1c < 7% without a severe hypoglycaemic episode at 1 year; a greater proportion of patients also achieved HbA1c < 6% or < 8% at 1 year compared with baseline (Supplementary Material Fig. S3). This occurred more frequently in patients with T2D versus those with T1D.
Discussion
This was a prospective, observational, open-label, multicentre, post-marketing surveillance study of patients with diabetes requiring insulin in Japan, who were initiated on IDegAsp at their treating physician’s discretion in clinical practice. Over 1 year of IDegAsp treatment, rates of AEs and SAEs were low, as were rates of ADRs and SADRs. Rates of study drug discontinuation due to AEs after 1 year were also low—taking place in 2.7% of the SAS—indicating that IDegAsp was generally well tolerated.
RCTs of IDegAsp have previously been conducted in international and Japanese populations, which have assessed safety and tolerability in T1D and across the clinical continuum of T2D [8,9,10,11,12]. However, while RCTs offer many benefits for collecting high-quality evidence and reducing bias, supporting real-world data are key to confirming the generalisability of findings to realistic clinical practice settings. Additionally, given potential differences in local practice, and in disease characteristics of local populations, studies conducted in Japanese patients are also an important regulatory requirement of the PMDA, to confirm the results of global studies.
In this study, the most commonly identified AE by PT was hypoglycaemia, and by SOC was ‘metabolism, and nutrition disorders’. ‘Neoplasms’ were the most frequently occurring SAE by SOC, with ‘pneumonia’ the most common by PT. There were no new safety signals identified in Japanese patients compared with the global RCTs, and the AE profile for IDegAsp was also consistent with the known safety profiles of its individual components. Rates of neoplasms were low and in line with previous clinical trials with IDegAsp.
IDegAsp has also previously been examined in two Japanese RCTs of patients with T2D who were insulin-naïve (once-daily dosing) and insulin-experienced (twice-daily dosing) [15, 16]. The incidence of AEs over 26 weeks in these trials was 69.5% and 71.0%, respectively, compared with 10.0% over 1 year in this study [15, 16]. This was considerably higher than the rates of AEs reported in this study; this is likely to be due to the significant differences in detection and reporting of AEs between RCTs, wherein they are likely to be systematically collected, and in clinical practice, where there may be considerable reporting bias. The incidence of SAEs in the RCTs was 8.2% and 3.4%, respectively, compared with 4.2% in this study. The smaller disparity between the results of this analysis and previous trials may reflect that SAEs are more likely than AEs to be reported by patients in clinical practice.
Similarly, the rates of reported hypoglycaemia were generally low within this study, with few reported incidences of severe episodes in particular. The disparity in hypoglycaemia rates between RCTs (e.g. [15,16,17]) and this study may be due to similar reasons as those mentioned above for AEs. Although hypoglycaemia may be more likely in a treat-to-target trial versus a real-world study, it should also be considered that patients may under-recognise and under-report hypoglycaemia, and that reporting bias may be an important factor in differences in reported rates. Equally, the wide CI for the hypoglycaemia rate estimates likely reflects the relatively small number of episodes occurring that could be included in the analysis.
Overall, the safety profiles of IDegAsp in patients with T1D and T2D were generally consistent, albeit with a slightly higher rate of AEs and hypoglycaemic episodes among patients with T1D. However, relatively few patients with T1D were identified for inclusion in the study compared with T2D, meaning that these data for T1D may be less robust, and this may be reflected in the large CI for the rate of AEs after initiating IDegAsp in patients with T1D. It is also notable that the rates of both AEs and severe hypoglycaemia were slightly higher among older patients compared with younger patients. This is notable given the large elderly population in Japan; however, in light of the relatively small number of events and large uncertainties, these results should be interpreted with caution.
To our knowledge, this is the first study to prospectively investigate glycaemic control with IDegAsp in Japanese patients with diabetes over 1 year (52 weeks) in routine practice. In comparison, a previous study assessed glycaemic control with IDegAsp in Japanese patients with T2D over a 1-year period; however, that study was retrospectively designed [22]. Furthermore, a shorter (26-week), prospective study of IDegAsp in Japanese patients with T2D has been completed [23]. Initiating IDegAsp was associated with significant reductions in HbA1c and FPG at 6 months, which were durable at 1 year. The most notable reductions in HbA1c were observed in younger people, and those with T2D. Overall, over a fifth of patients who had an HbA1c measurement available at EOS achieved an HbA1c < 7% at 1 year, and in particular without experiencing severe hypoglycaemia. This may be an important clinical consideration, given that hypoglycaemia can be a barrier to insulin intensification, particularly in elderly patients. The proportion of patients achieving HbA1c targets was greater among patients with T2D than T1D, which is in keeping with outcomes in previous trials.
The significant improvements in glycaemic control observed in this study are consistent with previous findings [15, 16]. However, the magnitude of HbA1c reductions was smaller in this study compared with previous RCTs in patients with T2D from Japan (1.4% for both) [15, 16], which is likely explained by the differences in the study populations, given the considerably more permissive and broad eligibility criteria here, and the prior therapies used by the RCT cohorts, and in the trial design. The RCTs used a treat-to-target trial design, with a pre-specified titration algorithm, compared with the non-interventional study design presented here. Antidiabetic medications were also more likely to have been prescribed prior to this study compared with the RCTs, and therefore it is not unexpected for the new therapy to have exerted less effect here.
This study was designed to reflect clinical practice, with a real-world study setting and assessments and other diabetes management as per the treating physician. The long-term follow-up allowed for extended monitoring for new safety signals. Additionally, the use of permissive and broad inclusion criteria enhances the generalisability of the findings to the general population of patients with diabetes seen in clinical practice in Japan. Furthermore, the study employed a prospective design to optimise data collection that reflected routine clinical practice and reduced bias, and the large number of study sites and patients enrolled may contribute to a robust dataset within the limitations of an observational study.
The key limitation of the study is the open-label, single-arm, observational design. As with any open-label study, the absence of blinding to treatment introduces the risk of reporting bias. Equally, given that the study was non-interventional and did not use a comparator arm, it is not possible to assess whether switching to IDegAsp was responsible for the study outcomes. However, these elements of the study design were necessary to allow for the collection of a sufficiently large real-world dataset to evaluate long-term safety in clinical practice. In the absence of head-to-head study data, researchers might consider a network meta-analysis in an attempt to quantify the effectiveness of IDegAsp versus comparators in real-world settings using the available data.
This study also did not use any form of imputation for effectiveness endpoints, and patients with missing data at a given time point were not included within the analysis. This may have led to selection bias; however, while a relatively small number of patients had sufficient FPG data at EOS, a large proportion of the SAS had sufficient data to be included in the EAS at EOS for change in HbA1c.
Conclusion
The findings of this post-marketing surveillance study of patients with diabetes in Japan support a long-term safety profile for IDegAsp in line with its component products, and previous results in global populations. No new safety or tolerability signals were identified, and initiating IDegAsp in clinical practice was associated with durable glycaemic benefits. These results support the findings of previous RCTs and suggest that IDegAsp may be a well-tolerated treatment option for Japanese patients with diabetes who require insulin therapy.
References
International Diabetes Federation. IDF diabetes atlas. 9th edn. 2019. https://www.idf.org/e-library/epidemiology-research/diabetes-atlas/159-idf-diabetes-atlas-ninth-edition-2019.html. Accessed 15 Mar 2021.
Kaku K. Pathophysiology of type 2 diabetes and its treatment policy. JAMA. 2010;52:41–6.
Chan JC, Malik V, Jia W, et al. Diabetes in Asia: epidemiology, risk factors, and pathophysiology. JAMA. 2009;301(20):2129–40.
Russell-Jones D, Pouwer F, Khunti K. Identification of barriers to insulin therapy and approaches to overcoming them. Diabetes Obes Metab. 2018;20(3):488–96.
Yoshioka N, Ishii H, Tajima N, Iwamoto Y. Differences in physician and patient perceptions about insulin therapy for management of type 2 diabetes: the DAWN Japan study. Curr Med Res Opin. 2014;30(2):177–83.
Saeedi P, Petersohn I, Salpea P, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res Clin Pract. 2019;157:107843.
Haahr H, Fita EG, Heise T. A review of insulin degludec/insulin aspart: pharmacokinetic and pharmacodynamic properties and their implications in clinical use. Clin Pharmacokinet. 2017;56(4):339–54.
Kumar A, Franek E, Wise J, Niemeyer M, Mersebach H, Simo R. Efficacy and safety of once-daily insulin degludec/insulin aspart versus insulin glargine (U100) for 52 weeks in insulin-naive patients with type 2 diabetes: a randomized controlled trial. PLoS ONE. 2016;11(10):e0163350.
Kumar S, Jang HC, Demirag NG, Skjoth TV, Endahl L, Bode B. Efficacy and safety of once-daily insulin degludec/insulin aspart compared with once-daily insulin glargine in participants with type 2 diabetes: a randomized, treat-to-target study. Diabet Med. 2017;34(2):180–8.
Hirsch IB, Bode B, Courreges JP, et al. Insulin degludec/insulin aspart administered once daily at any meal, with insulin aspart at other meals versus a standard basal-bolus regimen in patients with type 1 diabetes: a 26-week, phase 3, randomized, open-label, treat-to-target trial. Diabetes Care. 2012;35(11):2174–81.
Fulcher GR, Christiansen JS, Bantwal G, et al. Comparison of insulin degludec/insulin aspart and biphasic insulin aspart 30 in uncontrolled, insulin-treated type 2 diabetes: a phase 3a, randomized, treat-to-target trial. Diabetes Care. 2014;37(8):2084–90.
Rodbard HW, Cariou B, Pieber TR, Endahl LA, Zacho J, Cooper JG. Treatment intensification with an insulin degludec (IDeg)/insulin aspart (IAsp) co-formulation twice daily compared with basal IDeg and prandial IAsp in type 2 diabetes: a randomized, controlled phase III trial. Diabetes Obes Metab. 2016;18(3):274–80.
Novo Nordisk. Ryzodeg summary of product characteristics®. 2013. https://www.ema.europa.eu/en/documents/product-information/ryzodeg-epar-product-information_en.pdf. Accessed 19 Feb 2021.
Novo Nordisk. Ryzodeg® Prescribing information. 2015. https://www.novo-pi.com/ryzodeg7030.pdf. Accessed 19 Feb 2021.
Onishi Y, Ono Y, Rabol R, Endahl L, Nakamura S. Superior glycaemic control with once-daily insulin degludec/insulin aspart versus insulin glargine in Japanese adults with type 2 diabetes inadequately controlled with oral drugs: a randomized, controlled phase 3 trial. Diabetes Obes Metab. 2013;15(9):826–32.
Kaneko S, Chow F, Choi DS, et al. Insulin degludec/insulin aspart versus biphasic insulin aspart 30 in Asian patients with type 2 diabetes inadequately controlled on basal or pre-/self-mixed insulin: a 26-week, randomised, treat-to-target trial. Diabetes Res Clin Pract. 2015;107(1):139–47.
Taneda S, Hyllested-Winge J, Gall MA, Kaneko S, Hirao K. Insulin degludec/insulin aspart versus biphasic insulin aspart 30 twice daily in insulin-experienced Japanese subjects with uncontrolled type 2 diabetes: subgroup analysis of a Pan-Asian, treat-to-target phase 3 trial. J Diabetes. 2017;9(3):243–7.
Haahr H, Sasaki T, Bardtrum L, Ikushima I. Insulin degludec/insulin aspart in Japanese patients with type 1 diabetes mellitus: distinct prandial and basal glucose-lowering effects. J Diabetes Investig. 2016;7(4):574–80.
Evaluation and Licensing Division PaFSB. Ryzodeg, report on the deliberation results. 2012.
Pharmaceuticals and Medical Devices Agency. Ryzodeg® combination Injection FlexTouch®. 2020. https://www.pmda.go.jp/PmdaSearch/iyakuDetail/ResultDataSetPDF/620023_2492500G1025_1_04. Accessed 19 Feb 2021.
Haneda M, Noda M, Origasa H, et al. Japanese clinical practice guideline for diabetes 2016. Diabetol Int. 2018;9(1):1–45.
Kaneko S, da Rocha Fernandes JD, Yamamoto Y, Langer J, Faurby M. A Japanese study assessing glycemic control with use of IDegAsp co-formulation in patients with type 2 diabetes in clinical practice: the JAGUAR study. Adv Ther. 2021;38(3):1638–49.
Novo Nordisk A/S. RESILIENT: a research study, looking at how Ryzodeg® works in people with type 2 diabetes in local clinical practice in Japan (RESILIENT). 2019. https://clinicaltrials.gov/ct2/show/NCT03745157. Accessed Mar 2021.
Acknowledgements
The authors would like to thank the participants of the study.
Funding
Funding for this study was provided by Novo Nordisk A/S; the Open Access and Rapid Access journal fees were funded by Novo Nordisk Pharma Ltd.
Medical Writing, Editorial, and Other Assistance
The authors acknowledge the review and input of Akiko Sato of Novo Nordisk Pharma Ltd. Medical writing and editorial support for the development of this manuscript, under the direction of the authors, were provided by Chloe Harrison and Helen Marshall, of Ashfield MedComms, an Ashfield Health company, and funded by Novo Nordisk, Pharma Ltd.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authors' Contributions
Takuyuki Katabami, Kirsten Thorup Eriksen, Yuiko Yamamoto, and Yasushi Ishigaki contributed equally to the drafting, statistical analysis, and review of the manuscript. All authors were involved in the decision to submit the article for publication.
Disclosures
Takuyuki Katabami declares grants and/or personal fees from Astellas Pharma Inc., MSD Corporation, Ono Pharmaceutical Co., Ltd., Takeda Pharmaceutical Co., Ltd., Mitsubishi Tanabe Pharma Corporation, Eli Lilly Japan K.K., Novo Nordisk Pharma Ltd., Daiichi Sankyo Co., Ltd., Taisho Pharma Co., Ltd., Sumitomo Dainippon Pharma Co., Ltd., Kowa Pharmaceutical Co., Ltd., Nippon Boehringer Ingelheim Co., Ltd., Novartis Pharma K.K., Kyowa Kirin Co., Ltd., and Terumo Co., Ltd. Kirsten Thorup Eriksen is an employee of Novo Nordisk A/S. Yuiko Yamamoto is an employee of Novo Nordisk Pharmaceuticals Ltd. Yasushi Ishigaki has received lecture fees from Bayer Yakuhin, Kowa Pharmaceutical Co., Ltd., MSD Corporation, Novartis Pharma K.K., Novo Nordisk Pharma Ltd., Ono Pharmaceutical Co., Ltd., Sanofi K.K., and Takeda Pharmaceutical Co., Ltd.; scholarship donations from MSD Corporation, and Ono Pharmaceutical Co., Ltd.; and research funding from Daiichi Sankyo Co., Ltd.
Compliance with Ethics Guidelines
The study protocol was approved by the central IRB Japan Conference of Clinical Research, or at participating study sites. The study was conducted in accordance with the Declaration of Helsinki, 1964, and its later amendments, and the Pharmaceutical and Medical Devices Agency Good Post-Marketing Study Practice (GPSP) guidance. All patients provided informed consent for participation.
Data Availability
The datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Katabami, T., Eriksen, K.T., Yamamoto, Y. et al. Long-Term Safety and Clinical Outcomes with Insulin Degludec/Insulin Aspart Treatment in Japanese Patients with Diabetes: A Real-World, Prospective, Observational Study. Adv Ther 39, 544–561 (2022). https://doi.org/10.1007/s12325-021-01978-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-021-01978-2