Abstract
Introduction
There are limited real-world data on treatment patterns, comorbidities, and healthcare burden in pediatric patients with psoriasis. We examined patient demographics, comorbidity burden, treatment patterns, and healthcare use and costs in pediatric psoriasis.
Methods
A retrospective, real-world, exploratory study was conducted using US claims databases. Pediatric patients aged < 18 years with newly diagnosed psoriasis (index date) were selected from IBM® MarketScan® databases (2016–2018). Patients were enrolled continuously for ≥ 12 months pre- and post-index date. Pre-index demographics, comorbidity, treatment drug classes prescribed, and post-index healthcare resource utilization and costs were studied. Study measures are reported for total population and by severity (categorized as mild and moderate-to-severe psoriasis). Variables were compared using t-test (continuous) or chi-square and Fisher’s exact test (categorical).
Results
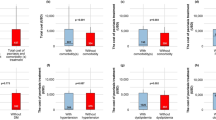
Overall, 4754 pediatric patients with psoriasis (58.3% females) met the selection criteria and were included in the study. Mean and standard deviation (SD) age was 12.6 (3.7) years on index date, with 13.4% patients having moderate-to-severe psoriasis. The mean (SD) Deyo-Charlson Comorbidity Index was 0.14 (0.40); anxiety (6.6%), depression (4.1%), and obesity (3.9%) were the most prevalent comorbidities observed. Topical treatments were prescribed to most patients as first-line treatment of mild (79.1%) and moderate-to-severe (52.0%) psoriasis. Other first-line therapies prescribed in moderate-to-severe cases included non-biologic systemics (21.0%), phototherapy (15.0%), and biologics (9.2%). Healthcare use and costs increased with psoriasis severity during the post-index period. Mean annual total all-cause costs per patient were higher for patients with moderate-to-severe psoriasis compared with mild psoriasis ($27,541 vs. $5,034; P < 0.001).
Conclusions
Psychiatric, metabolic, and inflammatory disorders were observed comorbidities in pediatric patients with psoriasis. For moderate-to-severe psoriasis, topicals, phototherapy, and biologics were a common first-, second-, and third-line treatment sequence. Higher unadjusted healthcare costs by severity were driven by outpatient prescription costs.



Similar content being viewed by others
References
Paller AS, Singh R, Cloutier M, Gauthier-Loiselle M, Emond B, Guerin A, et al. Prevalence of psoriasis in children and adolescents in the United States: a claims-based analysis. J Drugs Dermatol. 2018;17(2):187–94.
Menter A, Cordoro KM, Davis DMR, Kroshinsky D, Paller AS, Armstrong AW, et al. Joint American Academy of Dermatology-National Psoriasis Foundation guidelines of care for the management and treatment of psoriasis in pediatric patients. J Am Acad Dermatol. 2020;82(1):161–201.
Phan K, Lee G, Fischer G. Pediatric psoriasis and association with cardiovascular and metabolic comorbidities: systematic review and meta-analysis. Pediatr Dermatol. 2020;37(4):661–9.
Paller AS, Schenfeld J, Accortt NA, Kricorian G. A retrospective cohort study to evaluate the development of comorbidities, including psychiatric comorbidities, among a pediatric psoriasis population. Pediatr Dermatol. 2019;36(3):290–7.
Tollefson MM, Van Houten HK, Asante D, Yao X, Maradit KH. Association of psoriasis with comorbidity development in children with psoriasis. JAMA Dermatol. 2018;154(3):286–92.
Kara T, Topkarci Z, Yilmaz S, Akaltun I, Erdogan B. Pediatric patients with psoriasis and psychiatric disorders: premorbidity and comorbidity in a case-control study. J Dermatolog Treat. 2019;30(2):129–34.
Osier E, Wang AS, Tollefson MM, Cordoro KM, Daniels SR, Eichenfield A, et al. Pediatric psoriasis comorbidity screening guidelines. JAMA Dermatol. 2017;153(7):698–704.
Eichenfield LF, Paller AS, Tom WL, Sugarman J, Hebert AA, Friedlander SF, et al. Pediatric psoriasis: evolving perspectives. Pediatr Dermatol. 2018;35(2):170–81.
Etanercept [package insert]. Thousand Oaks, CA: Amgen Inc.; 2020. Available at https://www.pi.amgen.com/~/media/amgen/repositorysites/pi-amgen-com/enbrel/enbrel_pi.pdf. Revised August 2020.
Ustekinumab [package insert]. Horsham, PA: Janssen Biotech, Inc.; 2020. Available at http://www.janssenlabels.com/package-insert/product-monograph/prescribing-information/STELARA-pi.pdf. Revised December 2020.
Ixekizumab [package insert]. Indianapolis, IN: Eli Lilly and Company; 2020. Available at https://pi.lilly.com/us/taltz-uspi.pdf. Revised May 2020.
[EMA] European Medicines Agency. Extension of indication variation assessment report. EMA/CHMP/177541/2015. 2015. Available at https://www.ema.europa.eu/en/documents/variation-report/humira-h-c-481-ii-0134-epar-assessment-report-extension_en.pdf.
Hawkes JE, Chan TC, Krueger JG. Psoriasis pathogenesis and the development of novel targeted immune therapies. J Allergy Clin Immunol. 2017;140(3):645–53.
Bronckers I, Paller AS, West DP, Lara-Corrales I, Tollefson MM, Tom WL, et al. A comparison of psoriasis severity in pediatric patients treated with methotrexate vs biologic agents. JAMA Dermatol. 2020;156(4):384–92.
Lansang P, Bergman JN, Fiorillo L, Joseph M, Lara-Corrales I, Marcoux D, et al. Management of pediatric plaque psoriasis using biologics. J Am Acad Dermatol. 2020;82(1):213–21.
Klufas DM, Wald JM, Strober BE. Treatment of moderate to severe pediatric psoriasis: a retrospective case series. Pediatr Dermatol. 2016;33(2):142–9.
Beukelman T, Xie F, Chen L, Horton DB, Lewis JD, Mamtani R, et al. Risk of malignancy associated with paediatric use of tumour necrosis factor inhibitors. Ann Rheum Dis. 2018;77(7):1012–6.
Bronckers I, Seyger MMB, West DP, Lara-Corrales I, Tollefson M, Tom WL, et al. Safety of systemic agents for the treatment of pediatric psoriasis. JAMA Dermatol. 2017;153(11):1147–57.
Augustin M, Glaeske G, Radtke MA, Christophers E, Reich K, Schafer I. Epidemiology and comorbidity of psoriasis in children. Br J Dermatol. 2010;162(3):633–6.
Augustin M, Radtke MA, Glaeske G, Reich K, Christophers E, Schaefer I, et al. Epidemiology and comorbidity in children with psoriasis and atopic eczema. Dermatology. 2015;231(1):35–40.
Kimball AB, Wu EQ, Guerin A, Yu AP, Tsaneva M, Gupta SR, et al. Risks of developing psychiatric disorders in pediatric patients with psoriasis. J Am Acad Dermatol. 2012;67(4):651-657 e1-2.
Todberg T, Egeberg A, Jensen P, Gislason G, Skov L. Psychiatric comorbidities in children and adolescents with psoriasis: a population-based cohort study. Br J Dermatol. 2017;177(2):551–3.
Bronckers IM, Paller AS, van Geel MJ, van de Kerkhof PC, Seyger MM. Psoriasis in children and adolescents: diagnosis management and comorbidities. Paediatr Drugs. 2015;17(5):373–84.
Edson-Heredia E, Zhu B, Lefevre C, Wang M, Barrett A, Bushe CJ, et al. Prevalence and incidence rates of cardiovascular, autoimmune, and other diseases in patients with psoriatic or psoriatic arthritis: a retrospective study using Clinical Practice Research Datalink. J Eur Acad Dermatol Venereol. 2015;29(5):955–63.
Armstrong AW, Foster SA, Comer BS, Lin CY, Malatestinic W, Burge R, et al. Real-world health outcomes in adults with moderate-to-severe psoriasis in the United States: a population study using electronic health records to examine patient-perceived treatment effectiveness, medication use, and healthcare resource utilization. BMC Dermatol. 2018;18(1):4.
Evans C. Managed care aspects of psoriasis and psoriatic arthritis. Am J Manag Care. 2016;22(8 Suppl):s238–43.
Vogel SA, Yentzer B, Davis SA, Feldman SR, Cordoro KM. Trends in pediatric psoriasis outpatient health care delivery in the United States. Arch Dermatol. 2012;148(1):66–71.
Patel KR, Lee HH, Rastogi S, Singam V, Vakharia PP, Silverberg JI. Association of psoriasis with psychiatric hospitalization in United States children and adults. Dermatology. 2019;235(4):276–86.
Murage MJ, Anderson A, Oliveria SA, Casso D, Ojeh CK, Muram TM, et al. Healthcare resource utilization and costs among psoriasis patients treated with biologics, overall and by disease severity. J Med Econ. 2018;21(8):745–54.
Acknowledgements
Funding
This research and Rapid Service and Open Access Fees were funded by Eli Lilly and Company.
Medical Writing Assistance Editorial, and Other Assistance
The authors would like to acknowledge Amy Paller, MD, for her contribution towards the study review and interpretation of results. Minal Jaggar, PhD, an employee of Eli Lilly Services India Pvt. Ltd., provided medical writing support at the time of manuscript preparation. Uma Jyothi Kommoju, PhD, an employee of Eli Lilly Services India Private Limited, provided writing support at the time of revision of the manuscript.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Emily Edson-Heredia and Seth Anderson contributed to the concept and design of the study. Seth Anderson, Jiaying Guo, William Malatestinic, and Elizabeth Swason contributed to the data analysis. Emily Edson-Heredia, Seth Anderson, Jiaying Guo, Baojin Zhu, and Lara Wine-Lee contributed to the interpretation of the data. Seth Anderson and William Malatestinic contributed to drafting of the manuscript. Emily Edson-Heredia, Seth Anderson, Jiaying Guo, Baojin Zhu, Lara Wine-Lee, Elizabeth Swason, and William Malatestinic contributed to the critical revision of the manuscript.
Compliance with Ethics Guidelines
No human subjects were directly involved, precluding the requirement for internal review board approval.
Disclosures
Emily Edson-Heredia, Jiaying Guo, Baojin Zhu, and William N. Malatestinic are current employees and/or minor stockholders of Eli Lilly and Company. Seth Anderson was a former employee of Eli Lilly and Company and is a current employee of GlaxoSmithKline. Lara Wine-Lee has received grants from and is on the advisory boards for Eli Lilly and Company and AbbVie and has received grants from Celgene. ES has been a speaker for Almirall, Amgen, Eli Lilly and Company, Janssen, Ortho Dermatologics, Pfizer, and Sanofi-Regeneron and has been on advisory boards for Cassiopea, Eli Lilly and Company, Janssen, Ortho Dermatologics, and Sanofi-Regeneron. Part of the study results was presented at the Society of Pediatric Dermatology virtual conference 2020 and 8th Pediatric Dermatology Research Alliance (PeDRA) Annual Conference 2020 held virtually.
Data Availability
All data generated or analyzed during this study are available from the corresponding author upon reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Edson-Heredia, E., Anderson, S., Guo, J. et al. Real-World Claims Analyses of Comorbidity Burden, Treatment Pattern, Healthcare Resource Utilization, and Costs in Pediatric Psoriasis. Adv Ther 38, 3948–3961 (2021). https://doi.org/10.1007/s12325-021-01795-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-021-01795-7