Abstract
Background
Acute gastrointestinal bleeding (GIB) rapidly reduces effective blood volume, thereby precipitating acute kidney injury (AKI). Terlipressin, which can induce splanchnic vasoconstriction and increase renal perfusion, has been recommended for acute GIB and hepatorenal syndrome in liver cirrhosis. Thus, we hypothesized that terlipressin might be beneficial for cirrhotic patients with acute GIB and renal impairment.
Methods
In this Chinese multi-center study, 1644 cirrhotic patients with acute GIB were retrospectively enrolled. AKI was defined according to the International Club of Ascites (ICA) criteria. Renal dysfunction was defined as serum creatinine (sCr) > 133 μmol/L at admission and/or any time point during hospitalization. Incidence of renal impairment and in-hospital mortality were the primary end-points.
Results
The incidence of any stage ICA-AKI, ICA-AKI stages 1B, 2, and 3, and renal dysfunction in cirrhotic patients with acute GIB was 7.1%, 1.8%, and 5.0%, respectively. The in-hospital mortality was significantly increased by renal dysfunction (14.5% vs. 2.2%, P < 0.001) and ICA-AKI stages 1B, 2, and 3 (11.1% vs. 2.8%, P = 0.011), but not any stage ICA-AKI (5.7% vs. 2.7%, P = 0.083). The in-hospital mortality was significantly decreased by terlipressin in patients with renal dysfunction (3.6% vs. 20.0%, P = 0.044), but not in those with any stage ICA-AKI (4.5% vs. 6.0%, P = 0.799) or ICA-AKI stages 1B, 2, and 3 (0.0% vs. 14.3%, P = 0.326).
Conclusion
Renal dysfunction increased the in-hospital mortality of cirrhotic patients with acute GIB. Terlipressin might decrease the in-hospital mortality of cirrhotic patients with acute GIB and renal dysfunction.
Trial Registration
NCT03846180 (https://clinicaltrials.gov).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Acute gastrointestinal bleeding rapidly reduces effective blood volume, thereby precipitating acute kidney injury. Terlipressin can induce splanchnic vasoconstriction and increase renal perfusion. |
We hypothesized that terlipressin might be beneficial for cirrhotic patients with acute gastrointestinal bleeding and renal impairment. |
What was learned from the study? |
Renal dysfunction and ICA-AKI stages 1B, 2, and 3 are associated with an increased mortality in cirrhotic patients with acute gastrointestinal bleeding. |
Terlipressin may improve the survival in cirrhotic patients with acute gastrointestinal bleeding and renal dysfunction. |
Introduction
Acute gastrointestinal bleeding (GIB) is an urgent and life-threatening complication of liver cirrhosis with a short-term mortality of 15–20% [1]. Traditionally, the main goals of treatment include control of acute bleeding and prevention of rebleeding [2,3,4,5]. Terlipressin, somatostatin, and octreotide, which have similar treatment efficacy, have been recommended as the standard choice of vasoactive drugs for the management of acute GIB in liver cirrhosis according to the current consensus and guidelines [2,3,4,5].
After an acute massive GIB episode, effective blood volume can be significantly decreased, which will reduce renal blood flow, thereby potentially leading to the development of acute kidney injury (AKI) [6]. The negative effect of renal impairment on the outcomes of cirrhotic patients with acute GIB has been increasingly recognized [7, 8]. Terlipressin acts by binding V1 receptors which reside on the arterial smooth muscle within the splanchnic circulation, and then improves effective blood volume by inducing splanchnic vasoconstriction and increasing renal perfusion [9]. Accordingly, terlipressin is also recommended for the management of hepatorenal syndrome (HRS) [10, 11]. By contrast, it has been reported that somatostatin and octreotide have no beneficial effect on renal plasma flow and glomerular filtration rate [12,13,14,15]. In the present study, we tested the hypothesis that terlipressin was potentially beneficial for improving the outcome of cirrhotic patients with acute GIB and renal dysfunction.
Methods
Study Design
TORCH (i.e., Terlipressin vs. somatostatin/Octreotide on effect of Renal function in Cirrhotic patients with acute gastrointestinal Hemorrhage) is an investigator-initiated retrospective multi-center study across 13 centers from 8 provinces or municipalities in China, which aimed to explore the effect of terlipressin on renal function and in-hospital mortality in cirrhotic patients with acute GIB. The study was approved by the Medical Ethical Committee of the General Hospital of Northern Theater Command, which is the principal affiliation of this study. The Approval No. was k (2019) 01. This study was registered in the ClinicalTrials.gov (NCT03846180) and launched on February 16, 2019. The data collection at each participating center ended on April 30, 2019. The accuracy of the data was checked in May 2019.
The medical records collected from January 2010 to December 2018 were reviewed by the investigators at each center. Patients of any age and gender were included in this study if they met the following criteria: (1) diagnosis of liver cirrhosis based on the history of chronic liver diseases, clinical manifestations, laboratory tests, imaging, and histology, if necessary; (2) acute GIB from any source; and (3) treatment with terlipressin and/or somatostatin/octreotide. Criteria for exclusion were as follows: (1) diagnosis of parenchymal nephropathy; (2) missing serum creatinine (sCr) at admission; (3) duration of terlipressin or somatostatin/octreotide shorter than 3 days [4]; (4) missing sCr after vasoactive drugs; (5) transjugular intrahepatic portosystemic shunt, splenectomy, surgical shunt, or liver transplantation; and (6) diagnosis of ischemic hepatitis, which was defined as an increase in either alanine aminotransferase (ALT) or aspartate aminotransferase (AST) to a level of more than 10 times the upper limit of normal [16]. Patients who did not undergo gastrointestinal endoscopy nor those with comorbidities and malignancy were deliberately excluded.
Data Collection
The primary data were collected as follows: age, gender, etiology of liver cirrhosis, history of GIB, clinical manifestations of acute GIB, ascites, hepatic encephalopathy, hepatocellular carcinoma, mean arterial pressure, sCr at admission and after treatment, other laboratory tests at admission [i.e., hemoglobin (Hb), platelet count, total bilirubin, serum albumin, ALT, AST, sodium, and international normalized ratio (INR)], Child–Pugh score, Child–Pugh class, model for end-stage liver disease (MELD), vasoactive drugs during hospitalization (i.e., terlipressin, somatostatin, and octreotide), upper gastrointestinal endoscopic examinations and treatment, blood transfusion, 5-day rebleeding and death, and in-hospital death.
Diagnosis and Definitions
Acute GIB was defined as hematemesis, coffee ground emesis, melena, and hematochezia within 5 days before admission.
The etiology of acute GIB mainly included portal hypertension-related GIB (i.e., esophageal variceal bleeding, gastric varcieal bleeding, and portal hypertensive gastropathy) and non-portal hypertension-related GIB (i.e., peptic ulcer and unclear reasons).
The severity of acute GIB was evaluated according to the clinical manifestations of GIB (hematemesis/coffee ground emesis or melena/hematochezia) at admission [17], Hb concentration (< 70 g/L or ≥ 70 g/L) at admission, systemic hemodynamic status [systolic blood pressure (BP) < 90 mmHg or ≥ 90 mmHg, heart rate ≥ 100 beats per minute (b.p.m.) or < 100 b.p.m.] at admission, and blood transfusion (yes or no) during hospitalization.
AKI was defined as an absolute increase in sCr ≥ 26.5 µmol/L within the first 48 h or a percentage of increase in sCr ≥ 50% within the prior 7 days from baseline according to the criteria of the International Club of Ascites (ICA) [10]. sCr at baseline was defined as the sCr value obtained at admission, because sCr before admission was rarely available in patients developing acute episodes of GIB. AKI stage 1 was defined as an increase in sCr ≥ 26.5 µmol/L or ≥ 1 .5 to 2-fold from baseline, including AKI stage 1A (sCr ≤ 133 µmol/L) and 1B (sCr > 133 µmol/L); AKI stage 2 was defined as an increase in sCr > 2 to 3-fold from baseline; AKI stage 3 was defined as an increase in sCr > 3-fold from baseline or sCr ≥ 353.6 μmol/L with an acute increase in sCr ≥ 26.5 μmol/L or initiation of renal replacement therapy. Initial AKI stage was defined as the one at the first time of developing AKI during hospitalization. Progression or no progression was determined by the AKI stage nearest to discharge as compared with the initial AKI stage.
Renal dysfunction was defined as sCr > 133 μmol/L at admission and/or any time point during hospitalization in this study, which was modified according to the previous studies [7, 8].
Outcomes
The study outcomes mainly included: (1) the incidence of ICA-AKI, ICA-AKI stages 1B, 2, and 3, and renal dysfunction in cirrhotic patients with acute GIB, (2) the association of ICA-AKI, ICA-AKI stages 1B, 2, and 3, and renal dysfunction with in-hospital mortality of cirrhotic patients with acute GIB, and (3) the effect of terlipressin on in-hospital mortality of patients with ICA-AKI, ICA-AKI stages 1B, 2, and 3, and renal dysfunction.
Statistical Analyses
Continuous variables were expressed as median (range) and compared using the nonparametric Mann–Whitney U test. Categorical variables were expressed as frequency (percentage) and compared using the Chi-square test. Subgroup analyses were performed according to the etiology and severity of acute GIB. Cumulative survival rates were calculated by the Kaplan–Meier curves and compared by using the log-rank test. A two-tailed P < 0.05 was considered statistically significant. SPSS 20.0 (IBM, College Station, TX, USA) statistical package and Stata/SE 12.0 (Stata, College Station, TX, USA) software were employed for all statistical analyses.
Results
Patients
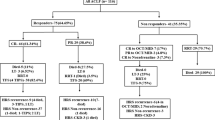
A total of 1644 cirrhotic patients with acute GIB were included. Their median age was 57 (range 18–91) years and most were male (1155, 70.3%) (Table 1). The most common etiology of liver cirrhosis was hepatitis B viral infection (853, 51.9%) followed by alcohol abuse (407, 24.8%). A majority of patients had Child–Pugh class B (922, 57.9%). Median MELD score at admission was 11.55 (range 6.43–39.31). As for the use of vasoactive drugs, 746 (45.4%), 1253 (76.2%), and 850 (51.7%) patients received terlipressin, somatostatin, and octreotide, respectively.
Incidence of ICA-AKI and its Effect on In-Hospital Mortality
sCr was re-tested within the first 48 h in 991 patients, of whom 56 could be diagnosed with ICA-AKI due to an absolute increase in sCr ≥ 26.5 µmol/L from baseline; sCr was re-tested within the first 7 days in 1503 patients, of whom 81 could be diagnosed with ICA-AKI due to a percentage of increase in sCr ≥ 50% from baseline; and 31 patients met both of the two criteria. Thus, 106 (7.1%) patients were diagnosed with ICA-AKI (Fig. S1), including 79 at ICA-AKI stage 1A, 11 at ICA-AKI stage 1B, 10 at ICA-AKI stage 2, and 6 at ICA-AKI stage 3. Among the 1503 patients evaluable for the criteria of ICA-AKI, 44 (2.9%) patients died during hospitalization. The causes of death were uncontrolled gastrointestinal bleeding (n = 23), multiple organ failure (n = 13), liver failure (n = 4), renal failure (n = 2), advanced liver cancer (n = 1), and septic shock (n = 1). The in-hospital mortality was not significantly different between patients with and without ICA-AKI [5.7% (6/106) vs. 2.7% (38/1397), P = 0.083]. Kaplan–Meier curve analysis also did not find any significant difference in cumulative survival rate between them (P = 0.185) (Fig. 1a). In subgroup analyses, ICA-AKI significantly increased the in-hospital mortality in patients with melena/hematochezia (P = 0.003), Hb ≥ 70 g/L at admission (P = 0.031), and systolic BP ≥ 90 mmHg at admission (P = 0.047), but not in others (Table S1).
Effect of terlipressin on ICA-AKI and In-Hospital Mortality
Among the 106 patients diagnosed with ICA-AKI, 22 received terlipressin and 84 did not receive terlipressin after a diagnosis of ICA-AKI (Table 2). Among them, 6 (5.7%) patients died during hospitalization. The in-hospital mortality was not significantly different between patients treated with and without terlipressin [4.5% (1/22) vs. 6.0% (5/84), P = 0.799]. Kaplan–Meier curve analysis also did not find any significant difference in cumulative survival rate between them (P = 0.641) (Fig. 1b). Because sCr was not re-tested after a diagnosis of ICA-AKI in 21 patients, 85 patients were finally evaluable for the progression of ICA-AKI. The rate of progression of ICA-AKI was not significantly different between patients treated with and without terlipressin [14.3% (3/21) vs. 10.9% (7/64), P = 0.679].
Incidence of ICA-AKI Stages 1B, 2, and 3 and its Effect on In-Hospital Mortality
There were 27 patients (1.8%) diagnosed with ICA-AKI stages 1B, 2, and 3 (Fig. S2). The in-hospital mortality was significantly higher in patients with ICA-AKI stages 1B, 2, and 3 than those with ICA-AKI stage 1A and no ICA-AKI [11.1% (3/27) vs. 2.8% (41/1476), P = 0.011]. Kaplan–Meier curve analysis also found a significant difference in cumulative survival rate between them (P = 0.002) (Fig. 2a). In subgroup analyses, ICA-AKI stages 1B, 2, and 3 significantly increased the in-hospital mortality in patients with melena/hematochezia (P = 0.001), Hb ≥ 70 g/L at admission (P = 0.041), systolic BP ≥ 90 mmHg at admission (P = 0.005), heart rate < 100 b.p.m. at admission (P = 0.037), blood transfusion (P = 0.007), and non-portal hypertension related GIB (P = 0.006), but not in others (Table S1).
Effect of Terlipressin on ICA-AKI Stages 1B, 2, and 3 and In-Hospital Mortality
Among the 27 patients diagnosed with ICA-AKI stages 1B, 2, and 3, 6 received terlipressin and 21 did not receive terlipressin after a diagnosis of ICA-AKI stages 1B, 2, and 3 (Table 3). Among them, 3 (11.1%) patients died during hospitalization. The in-hospital mortality was not significantly different between patients treated with and without terlipressin (0.0% [0/6] vs. 14.3% [3/21], P = 0.326). Kaplan–Meier curve analysis also did not find any significant difference in cumulative survival rate between them (P = 0.297) (Fig. 2b). Because sCr was not re-tested after a diagnosis of ICA-AKI stages 1B, 2, and 3 in 6 patients, 21 patients were finally evaluable for the progression of ICA-AKI stages 1B, 2, and 3. The rate of progression of ICA-AKI was not significantly different between patients treated with and without terlipressin (16.7% [1/6] vs. 26.7% [4/15], P = 0.627).
Incidence of Renal Dysfunction and its Effect on In-Hospital Mortality
sCr was re-tested in all of the 1644 included patients after admission. Among them, 51 patients had sCr > 133 μmol/L at admission; 70 had sCr > 133 μmol/L at any time after admission; and 38 had sCr > 133 μmol/L at both of the two time points. Thus, 83 (5.0%) patients were diagnosed with renal dysfunction (Fig. S3). Among the 1644 patients evaluable for the criteria of renal dysfunction, 47 (2.9%) patients died during hospitalization. The causes of death were uncontrolled gastrointestinal bleeding (n = 26), multiple organ failure (n = 13), liver failure (n = 4), renal failure (n = 2), advanced liver cancer (n = 1), and septic shock (n = 1). The in-hospital mortality was significantly higher in patients with renal dysfunction than those without renal dysfunction [14.5% (12/83) vs. 2.2% (35/1561), P < 0.001]. Kaplan–Meier curve analysis also found a significant difference in cumulative survival rate between them (P < 0.001) (Fig. 3a). In subgroup analyses, renal dysfunction significantly increased the in-hospital mortality in patients with hematemesis/coffee ground emesis (P < 0.001), both Hb < 70 g/L (P < 0.001) and ≥ 70 g/L (P < 0.001) at admission, both systolic BP < 90 mmHg (P < 0.001) and ≥ 90 mmHg (P < 0.001) at admission, both heart rate ≥ 100 b.p.m. (P < 0.001) and < 100 b.p.m. (P < 0.001) at admission, blood transfusion (P = 0.007), both portal hypertension (P = 0.002) and non-portal hypertension (P < 0.001)-related GIB, but not in others (Table S1).
Effect of Terlipressin on Renal Dysfunction and In-Hospital Mortality
Among the 83 patients diagnosed with renal dysfunction, 28 received terlipressin and 55 did not receive terlipressin after a diagnosis of renal dysfunction (Table 4). Among them, 12 (14.5%) died during hospitalization. The in-hospital mortality was significantly lower in patients treated with terlipressin than those treated without terlipressin [3.6% (1/28) vs. 20.0% (11/55), P = 0.044]. Kaplan–Meier curve analysis also found a significant difference in cumulative survival rate between them (P = 0.040) (Fig. 3b). Because sCr was not re-tested after a diagnosis of renal dysfunction in 13 patients, 70 patients were finally evaluable for the dynamic change of sCr. The rate of a decrease in sCr was significantly higher in patients treated with terlipressin than those treated without terlipressin [92.9% (26/28) vs. 59.5% (25/42), P = 0.002].
Discussion
Generally, renal impairment, such as AKI and renal failure, is a negative prognostic indicator in patients with liver cirrhosis [18,19,20]. In detail, it is significantly related to higher mortality in cirrhotic patients accompanied with different decompensation events, such as infection (i.e., spontaneous bacterial peritonitis, cellulitis, or other types of infection) [21,22,23], ascites [24,25,26], acute-on-chronic liver failure [27], and critical illness [28]. Recently, our meta-analysis confirmed that renal dysfunction significantly increased a 4.92-fold risk of death in cirrhotic patients with acute GIB [29]. In consistency with previous studies, the present study has demonstrated that both ICA-AKI stages 1B-3 and renal dysfunction significantly increased the risk of in-hospital death. However, the impact of any stage ICA-AKI on the in-hospital death disappeared, suggesting that renal impairment reflected by any stage ICA-AKI might not be a favorite predictor for outcomes of cirrhotic patients with acute GIB.
The diagnosis of ICA-AKI depends on a dynamic change of sCr within a short period (48 h and 7 days), but does not consider the absolute sCr value at admission or dynamic change of sCr after 7 days [10]. Acute GIB is an urgent medical condition in which pre-admission sCr is often lacking and sCr at admission has to be defined as baseline value. Thus, some patients with massive GIB might have already developed AKI episodes before they were sent to hospital. Indeed, in our study, there were 51 patients with sCr > 133 μmol/L (range 134.00–372.80) at admission, of whom 7 (13.7%) were diagnosed with ICA-AKI and the remaining 44 (86.3%) were not diagnosed with ICA-AKI. The reasons why the 44 patients were not diagnosed with ICA-AKI were as follows: (1) 27 (61.4%) patients had sCr values re-tested within 48 h, of whom 19 had an absolute increase in sCr < 26.5 μmol/L, 1 had an unchanged sCr, and 7 had a decrease in sCr; (2) 42 (95.5%) patients had sCr values re-tested within 7 days, of whom 14 had a percentage of increase in sCr < 50%, 1 had an unchanged sCr, and 27 had a decrease in sCr; and (3) 2 (4.5%) patients did not have sCr re-tested within 48 h or 3–7 days (Fig. S4). Additionally, in our study, there were 122 patients with a percentage of increase in sCr ≥ 50% during hospitalization, of whom 82 (67.2%) were diagnosed with ICA-AKI and the remaining 40 (32.8%) were not diagnosed with ICA-AKI due to a percentage of increase in sCr ≥ 50% after 7 days rather than within 7 days. These considerations regarding sCr at admission and change of sCr after 7 days are potentially helpful for improving the definition of ICA-AKI in cirrhotic patients with acute GIB.
By comparison, our study found that ICA-AKI stages 1B, 2, and 3, which had sCr > 133 μmol/L, and renal dysfunction, which was defined as sCr > 133 μmol/L at any time, significantly influenced the in-hospital mortality. Indeed, the cut-off value of sCr > 133 μmol/L has been supported by previous studies. Cirrhotic patients with infection and sCr > 133 μmol/L had an inferior survival rate compared with those with sCr ≤ 133 μmol/L (63% vs. 81%) [21, 30]. Furthermore, the sub-classification of AKI stage 1 was in favor of the prognostic importance of sCr > 133 μmol/L. Cirrhotic patients at AKI stage 1 with sCr < 133 μmol/L had a similar survival rate to those without AKI according to the Acute Kidney Injury Network criteria, but higher resolution and lower mortality than those at AKI stage 1 with sCr > 133 μmol/L [20, 24]. Similarly, cirrhotic patients at AKI stage 1 with sCr ≥ 133 μmol/L had significantly longer hospital stay and lower AKI resolution and survival rates as compared to those at AKI stage 1 with sCr < 133 μmol/L according to the ICA-AKI criteria [31]. In addition, the significant detrimental effect of sCr > 133 μmol/L on resolution and survival is also reported in cirrhotic patients with gastric variceal bleeding at any AKI stage [8]. Therefore, the identification of sCr > 133 μmol/L may be essential to evaluate the prognosis of cirrhotic patients with acute GIB.
Evidence from meta-analyses has confirmed that terlipressin is not superior to somatostatin or octreotide in cirrhosis in the terms of controlling bleeding or improving survival [32, 33]. In accordance with previous findings, our study also suggested that the mortality was not significantly different between cirrhotic patients with acute GIB who received terlipressin and those who did not receive terlipressin (somatostatin/octreotide). However, previous studies have never explored the effect of terlipressin on renal function parameters in such patients. Considering that terlipressin has been widely used for improving renal function in patients with HRS [34], it might be beneficial in cirrhotic patients with acute GIB and renal dysfunction [35]. By contrast, somatostatin and octreotide seemed to be ineffective or detrimental to renal function in healthy subjects and cirrhotic patients [12,13,14,15]. Our study found that terlipressin significantly decreased the in-hospital mortality of cirrhotic patients with acute GIB who developed renal dysfunction. Thus, the theoretical advantage of telipressin over somatostatin and octreotide in such patients should be considered.
Our study had several limitations. First, the number of patients included varied among the participating centers. Because the deadline of data collection was pre-specified in our study, the investigators at each center collected the data as much as possible within the deadline and then filled the paper version case report forms and electronic tables. Second, the cause of GIB was not limited. Indeed, GIB from any source would lead to acute blood loss and pre-renal renal impairment. Additionally, the survival rate was similar between cirrhotic patients with variceal bleeding and acute peptic ulcer bleeding after a standard treatment strategy [36]. Third, due to the retrospective nature of this study, the etiology of AKI could not be accurately evaluated, which limited us to perform subgroup analysis according to the etiology of AKI. However, it should be noted that we have clearly excluded patients with a history of parenchymal nephropathy and those with ischemic hepatitis which may be potentially associated with acute tubular necrosis. Additionally, because all of our included patients had acute GIB, the use of diuretics is often delayed or abandoned in such patients. In this setting, HRS could not be evaluated, because the withdrawal of diuretics should be one of diagnosis criteria for HRS. Fourth, the time when sCr was re-examined during hospitalization was not restricted, despite patients with sCr values at admission and during hospitalization were considered eligible for our study. Fifth, the use of vasoactive drugs was not standardized, and a combination of vasoactive drugs was often employed. Sixth, endoscopy was not performed in all patients. Notably, a large-scale international study found that nearly one-third of patients manifested as hematemesis and/or melena did not undergo endoscopy examinations in real-world practice [37].
In conclusion, the management of ICA-AKI stages 1B, 2, and 3 and renal dysfunction should be considered in cirrhotic patients with acute GIB due to their effects on the in-hospital mortality. Additionally, terlipressin may be effective for the improvement of survival in cirrhotic patients with acute GIB and sCr > 133 μmol/L, probably because of its beneficial effect on renal function. Further well-designed prospective studies should be performed to compare the efficacy of terlipressin versus other vasoactive drugs in such patients.
References
Garcia-Tsao G, Bosch J. Management of varices and variceal hemorrhage in cirrhosis. N Engl J Med. 2010;362(9):823–32.
Garcia-Tsao G, Abraldes JG, Berzigotti A, Bosch J. Portal hypertensive bleeding in cirrhosis: risk stratification, diagnosis, and management: 2016 practice guidance by the American Association for the study of liver diseases. Hepatology. 2017;65(1):310–35.
EASL. EASL Clinical Practice Guidelines for the management of patients with decompensated cirrhosis. J Hepatol. 2018;69(2):406–60.
de Franchis R. Expanding consensus in portal hypertension: report of the Baveno VI Consensus Workshop: stratifying risk and individualizing care for portal hypertension. J Hepatol. 2015;63(3):743–52.
Tripathi D, Stanley AJ, Hayes PC, Patch D, Millson C, Mehrzad H, et al. UK guidelines on the management of variceal haemorrhage in cirrhotic patients. Gut. 2015;64(11):1680–704.
Garcia-Tsao G, Parikh CR, Viola A. Acute kidney injury in cirrhosis. Hepatology. 2008;48(6):2064–77.
Cardenas A, Gines P, Uriz J, Bessa X, Salmeron JM, Mas A, et al. Renal failure after upper gastrointestinal bleeding in cirrhosis: incidence, clinical course, predictive factors, and short-term prognosis. Hepatology. 2001;34(4 Pt 1):671–6.
Hsieh YC, Lee KC, Chen PH, Su CW, Hou MC, Lin HC. Acute kidney injury predicts mortality in cirrhotic patients with gastric variceal bleeding. J Gastroenterol Hepatol. 2017;32(11):1859–66.
Papaluca T, Gow P. Terlipressin: Current and emerging indications in chronic liver disease. J Gastroenterol Hepatol. 2018;33(3):591–8.
Angeli P, Gines P, Wong F, Bernardi M, Boyer TD, Gerbes A, et al. Diagnosis and management of acute kidney injury in patients with cirrhosis: revised consensus recommendations of the International Club of Ascites. J Hepatol. 2015;62(4):968–74.
Zhang J, Rossle M, Zhou X, Deng J, Liu L, Qi X. Terlipressin for the treatment of hepatorenal syndrome: an overview of current evidence. Curr Med Res Opin. 2019;35(5):859–68.
Vora JP, Owens DR, Ryder R, Atiea J, Luzio S, Hayes TM. Effect of somatostatin on renal function. Br Med J (Clin Res Ed). 1986;292(6537):1701–2.
Ottesen LH, Aagaard NK, Kiszka-Kanowitz M, Rehling M, Henriksen JH, Pedersen EB, et al. Effects of a long-acting formulation of octreotide on renal function and renal sodium handling in cirrhotic patients with portal hypertension: a randomized, double-blind, controlled trial. Hepatology. 2001;34(3):471–7.
Gines A, Salmeron JM, Gines P, Jimenez W, Salo J, Piera C, et al. Effects of somatostatin on renal function in cirrhosis. Gastroenterology. 1992;103(6):1868–74.
Malesci A, Tacconi M, Valentini A, Basilico M, Lorenzano E, Salerno F. Octreotide long-term treatment in patients with portal hypertension: persistent inhibition of postprandial glucagon response without major changes in renal function. J Hepatol. 1997;26(4):816–25.
Lightsey JM, Rockey DC. Current concepts in ischemic hepatitis. Curr Opin Gastroenterol. 2017;33(3):158–63.
Li Y, Li H, Zhu Q, Tsochatzis E, Wang R, Guo X, et al. Effect of acute upper gastrointestinal bleeding manifestations at admission on the in-hospital outcomes of liver cirrhosis: hematemesis versus melena without hematemesis. Eur J Gastroenterol Hepatol. 2019;31(11):1334–411.
Belcher JM, Garcia-Tsao G, Sanyal AJ, Bhogal H, Lim JK, Ansari N, et al. Association of AKI with mortality and complications in hospitalized patients with cirrhosis. Hepatology. 2013;57(2):753–62.
Fede G, D'Amico G, Arvaniti V, Tsochatzis E, Germani G, Georgiadis D, et al. Renal failure and cirrhosis: a systematic review of mortality and prognosis. J Hepatol. 2012;56(4):810–8.
Fagundes C, Barreto R, Guevara M, Garcia E, Sola E, Rodriguez E, et al. A modified acute kidney injury classification for diagnosis and risk stratification of impairment of kidney function in cirrhosis. J Hepatol. 2013;59(3):474–81.
Wong F, O'Leary JG, Reddy KR, Patton H, Kamath PS, Fallon MB, et al. New consensus definition of acute kidney injury accurately predicts 30-day mortality in patients with cirrhosis and infection. Gastroenterology. 2013;145(6):1280–8.e1.
Follo A, Llovet JM, Navasa M, Planas R, Forns X, Francitorra A, et al. Renal impairment after spontaneous bacterial peritonitis in cirrhosis: incidence, clinical course, predictive factors and prognosis. Hepatology. 1994;20(6):1495–501.
Garcia Garcia de Paredes A, Tellez L, Rodriguez Gandia MA, Martinez J, Rodriguez de Santiago E, Aguilera Castro L, et al. Incidence, predictive factors and impacts of acute kidney injury in cirrhotic patients hospitalized for cellulitis. Liver Int. 2018;38(2):285–94.
Piano S, Rosi S, Maresio G, Fasolato S, Cavallin M, Romano A, et al. Evaluation of the acute kidney injury network criteria in hospitalized patients with cirrhosis and ascites. J Hepatol. 2013;59(3):482–9.
Bucsics T, Mandorfer M, Schwabl P, Bota S, Sieghart W, Ferlitsch A, et al. Impact of acute kidney injury on prognosis of patients with liver cirrhosis and ascites: a retrospective cohort study. J Gastroenterol Hepatol. 2015;30(11):1657–65.
de Carvalho JR, Villela-Nogueira CA, Luiz RR, Guzzo PL, da Silva Rosa JM, Rocha E, et al. Acute Kidney Injury Network criteria as a predictor of hospital mortality in cirrhotic patients with ascites. J Clin Gastroenterol. 2012;46(3):e21–e2626.
Zang H, Liu F, Liu H, You S, Zhu B, Wan Z, et al. Incidence, risk factors and outcomes of acute kidney injury (AKI) in patients with acute-on-chronic liver failure (ACLF) of underlying cirrhosis. Hepatol Int. 2016;10(5):807–18.
Tu KH, Jenq CC, Tsai MH, Hsu HH, Chang MY, Tian YC, et al. Outcome scoring systems for short-term prognosis in critically ill cirrhotic patients. Shock. 2011;36(5):445–50.
Bai Z, Primignani M, Guo X, Zheng K, Li H, Qi X. Incidence and mortality of renal dysfunction in cirrhotic patients with acute gastrointestinal bleeding: a systematic review and meta-analysis. Expert Rev Gastroenterol Hepatol. 2019;13(12):1181–8.
Wong F, O'Leary JG, Reddy KR, Kamath PS, Garcia-Tsao G, Maliakkal B, et al. A cut-off serum creatinine value of 1.5 mg/dl for AKI—to be or not to be. J Hepatol. 2015;62(3):741–3.
Khatua CR, Sahu SK, Barik RK, Pradhan S, Panigrahi S, Mishra D, et al. Validation of International Club of Ascites subclassification of stage 1 acute kidney injury in chronic liver disease. JGH Open. 2019;3(4):290–4.
Wells M, Chande N, Adams P, Beaton M, Levstik M, Boyce E, et al. Meta-analysis: vasoactive medications for the management of acute variceal bleeds. Aliment Pharmacol Ther. 2012;35(11):1267–78.
Zhou X, Tripathi D, Song T, Shao L, Han B, Zhu J, et al. Terlipressin for the treatment of acute variceal bleeding: a systematic review and meta-analysis of randomized controlled trials. Medicine (Baltimore). 2018;97(48):e13437.
Nanda A, Reddy R, Safraz H, Salameh H, Singal AK. Pharmacological therapies for hepatorenal syndrome: a systematic review and meta-analysis. J Clin Gastroenterol. 2018;52(4):360–7.
Zhang J, Liu J, Wu Y, Romeiro FG, Levi Sandri GB, Zhou X, et al. Effect of terlipressin on renal function in cirrhotic patients with acute upper gastrointestinal bleeding. Ann Transl Med. 2020;8(6):340.
Ardevol A, Ibanez-Sanz G, Profitos J, Aracil C, Castellvi JM, Alvarado E, et al. Survival of patients with cirrhosis and acute peptic ulcer bleeding compared with variceal bleeding using current first-line therapies. Hepatology. 2018;67(4):1458–71.
Laine L, Laursen SB, Zakko L, Dalton HR, Ngu JH, Schultz M, et al. Severity and outcomes of upper gastrointestinal bleeding with bloody vs. coffee-grounds hematemesis. Am J Gastroenterol. 2018;113(3):358–66.
Acknowledgements
Funding
No funding was received for this study or publication of this article.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authorship Contributions
Conceptualization: Xingshun Qi; Methodology: Xingshun Qi and Xiangbo Xu; Software: Xiangbo Xu and Xingshun Qi; Validation: Xingshun Qi; Investigation: Xingshun Qi; Resource: Xiangbo Xu, Bang Liu, Su Lin, Bimin Li, Yunhai Wu, Yiling Li, Qiang Zhu, Yida Yang, Shanhong Tang, Fanping Meng, Yu Chen, Shanshan Yuan, Lichun Shao, and Xingshun Qi; Data curation: Xiangbo Xu, Bang Liu, Su Lin, Bimin Li, Yunhai Wu, Yiling Li, Qiang Zhu, Yida Yang, Shanhong Tang, Fanping Meng, Yu Chen, Shanshan Yuan, Lichun Shao, and Xingshun Qi; Writing–original draft: Xiangbo Xu and Xingshun Qi; Writing–review and editing: Xiangbo Xu, Bang Liu, Su Lin, Bimin Li, Yunhai Wu, Yiling Li, Qiang Zhu, Yida Yang, Shanhong Tang, Fanping Meng, Yu Chen, Shanshan Yuan, Lichun Shao, Mauro Bernardi, Eric M. Yoshida, and Xingshun Qi; Supervision: Xingshun Qi; Project administration: Xingshun Qi. All authors have made an intellectual contribution to the manuscript and approved the submission.
List of Investigators
The efforts of the investigators who collected data at each center should be acknowledged. They included Xiangbo Xu, Le Wang, Yang An, Ruirui Feng, Yingying Li, Fangfang Yi, Yanyan Wu, Li Luo, and Zhaohui Bai from General Hospital of Northern Theater Command; Bang Liu, Jing Lin and Lulu Zhu from 900 Hospital of the Joint Logistics Team; Su Lin, Ruolin Dong, Huoyu Li, Wen Lin, Xiaofan Wan, Mengru Wei, Haiyan Weng, Hui Xiao, and Li Zhao from The First Affiliated Hospital of Fujian Medical University; Bimin Li, Yixing Luo, Fangming Ruan, and Yuan Song from The First Affiliated Hospital of Nanchang University; Yunhai Wu, Yuan Ban, Jinli Hao, Na Sun, Qiaonan Tao, and Gang Zhang from The Sixth People's Hospital of Shenyang; Yiling Li, Ningning Wang, Zilu Zeng, Xue Wang, and Hao Bing from The First Affiliated Hospital of China Medical University; Qiang Zhu and Huanran Lv from Shandong Provincial Hospital Affiliated to Shandong University; Yida Yang and Dairong Xiang from The First Affiliated Hospital, College of Medicine, Zhejiang University; Shanhong Tang and Mengying Sun from General Hospital of Western Theater Command; Fanping Meng and Junqing Luan from The Fifth Medical Center of PLA General Hospital; Yu Chen and Manman Xu from YouAn Hospital, Capital Medical University; Shanshan Yuan from Xi'an Central Hospital; and Lichun Shao, Tingxue Song, Zewei Guo, Yuli Wang, and Yanfei Yu from Air Force Hospital of Northern Theater Command.
Prior Presentation
The abstract has been accepted as an E-poster presentation in the APDW 2019 conference.
Disclosures
Xiangbo Xu, Bang Liu, Su Lin, Bimin Li, Yunhai Wu, Yiling Li, Qiang Zhu, Yida Yang, Shanhong Tang, Fanping Meng, Yu Chen, Shanshan Yuan, Lichun Shao, Mauro Bernardi, Eric M. Yoshida, and Xingshun Qi have nothing to disclose.
Compliance with Ethics Guidelines
The study was conducted in accordance with the Helsinki Declaration and approved by the Medical Ethical Committee of the General Hospital of Northern Theater Command. [k (2019) 01]. Due to the retrospective observational nature of the study, the requirement for patient consent was waived.
Data Availability
The datasets during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Additional information
Digital Features
To view digital features for this article go to https://doi.org/10.6084/m9.figshare.12771014.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Xu, X., Liu, B., Lin, S. et al. Terlipressin May Decrease In-Hospital Mortality of Cirrhotic Patients with Acute Gastrointestinal Bleeding and Renal Dysfunction: A Retrospective Multicenter Observational Study. Adv Ther 37, 4396–4413 (2020). https://doi.org/10.1007/s12325-020-01466-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-020-01466-z