Abstract
Introduction
The incidence of inflammatory bowel disease (IBD) in Denmark is among the highest in the world, with Crohn’s disease and ulcerative colitis occurring at rates of 9.1 and 18.6 per 100,000 person-years respectively in 2010–2013. Anemia is the most prevalent extraintestinal complication of IBD, most commonly caused by iron deficiency. In treating IBD-associated iron deficiency anemia (IDA), intravenous iron is more effective and better tolerated and shows a faster response than oral iron. The present study evaluated resource use and costs associated with using iron isomaltoside (Monofer; IIM) versus ferric carboxymaltose (Ferinject; FCM) in patients with IDA and IBD in Denmark.
Methods
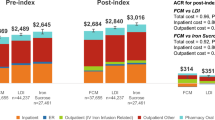
A budget impact model was developed to evaluate the cost of IIM compared with FCM from a Danish healthcare payer perspective. Iron deficits were modeled using dosing tables and a joint distribution of bodyweight [mean 75.4 kg, standard deviation (SD) 17.4 kg] and hemoglobin (mean 10.8 g/dL, SD 1.4 g/dl) based on observational data from patients with IBD. Retreatment frequency was modeled using a pooled retrospective analysis of randomized trial data, and costs were modeled using diagnosis-related groups with an outpatient infusion cost of DKK 2855.
Results
Using IIM required 1.2 infusions (per treatment) to correct the mean iron deficit compared with 1.6 with FCM. Treating 2.54 patients with IIM would therefore avoid one infusion compared with FCM. Patients using IIM required multiple infusions in 25.0% of cases compared with 64.3% with FCM. Over 5 years, total estimated costs were DKK 21,406 per patient with IIM compared with DKK 28,137 with FCM, corresponding to savings of DKK 6731 with IIM.
Conclusion
Using IIM in place of FCM markedly reduced the number of iron infusions required in patients with IBD and IDA in Denmark. The reduction in infusions was accompanied by reductions in cost compared with FCM.
Funding
Pharmacosmos A/S.




Similar content being viewed by others
References
Loddo I, Romano C. Inflammatory bowel disease: genetics, epigenetics, and pathogenesis. Front Immunol. 2015;6:551.
Lophaven SN, Lynge E, Burisch J. The incidence of inflammatory bowel disease in Denmark 1980–2013: a nationwide cohort study. Aliment Pharmacol Ther. 2017;45(7):961–72.
Molodecky NA, Soon IS, Rabi DM, et al. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology. 2012;142(46–54):e42.
Odes S, Vardi H, Friger M, Wolters F, Russel MG, Riis L, Munkholm P, Politi P, Tsianos E, Clofent J, Vermeire S, Monteiro E, Mouzas I, Fornaciari G, Sijbrandij J, Limonard C, Van Zeijl G, O’Morain C, Moum B, Vatn M, Stockbrugger R. Cost analysis and cost determinants in a European inflammatory bowel disease inception cohort with 10 years of follow-up evaluation. Gastroenterology. 2006;131(3):719–28.
Kaitha S, Bashir M, Ali T. Iron deficiency anemia in inflammatory bowel disease. World J Gastrointest Pathophysiol. 2015;6(3):62–72.
WHO. Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. Vitamin and mineral nutrition information system. World Health Organization, Geneva, Switzerland. 2011. Available form: http://www.who.int/vmnis/indicators/haemoglobin.pdf. Accessed 26 Jun 2018.
Dignass AU, Gasche C, Bettenworth D, et al. European Crohn’s and Colitis Organisation [ECCO]. European consensus on the diagnosis and management of iron deficiency and anaemia in inflammatory bowel diseases. J Crohns Colitis. 2015;9(3):211–22.
Aksan A, Işık H, Radeke HH, Dignass A, Stein J. Systematic review with network meta-analysis: comparative efficacy and tolerability of different intravenous iron formulations for the treatment of iron deficiency anaemia in patients with inflammatory bowel disease. Aliment Pharmacol Ther. 2017;45(10):1303–18.
Bhandari S. Update of a comparative analysis of cost minimization following the introduction of newly available intravenous iron therapies in hospital practice. Ther Clin Risk Manag. 2011;7:501–9.
Koch TA, Myers J, Goodnough LT. Intravenous iron therapy in patients with iron deficiency anemia: dosing considerations. Anemia. 2015;2015:763576.
Kulnigg S, Stoinov S, Simanenkov V, et al. A novel intravenous iron formulation for treatment of anemia in inflammatory bowel disease: the ferric carboxymaltose (FERINJECT) randomized controlled trial. Am J Gastroenterol. 2008;103(5):1182–92.
Pollock RF, Kappelgaard AM, Seitz L. An analysis of product wastage arising from dosing increment granularity in four modern growth hormone administration devices. Expert Opin Drug Deliv. 2015;12(3):353–60.
Cheng HL, Bryant C, Cook R, O’Connor H, Rooney K, Steinbeck K. The relationship between obesity and hypoferraemia in adults: a systematic review. Obes Rev. 2012;13(2):150–61.
Electronic Medicines Compendium (eMC). Ferinject (ferric carboxymaltose) summary of product characteristics. Available from: https://www.medicines.org.uk/emc/medicine/24167. Accessed 26 Jun 2018.
Frigstad SO, Haaber A, Bajor A, Fallingborg J, Hammarlund P, Bonderup OK, Blom H, Rannem T, Hellström PM. The NIMO Scandinavian Study: a prospective observational study of iron isomaltoside treatment in patients with iron deficiency. Gastroenterol Res Pract. 2017;2017:4585164.
Pollock RF, Muduma G. Intravenous iron treatments for iron deficiency anemia in inflammatory bowel disease: a budget impact analysis of iron isomaltoside 1000 (Monofer) in the UK. Expert Opin Drug Deliv. 2017;14(12):1439–46.
Kulnigg S, Teischinger L, Dejaco C, Waldhör T, Gasche C. Rapid recurrence of IBD-associated anemia and iron deficiency after intravenous iron sucrose and erythropoietin treatment. Am J Gastroenterol. 2009;104(6):1460–7.
Statistics Danmark. Folketal den 1. i kvartalet. 2018K2. Available from: https://www.dst.dk/da/Statistik/emner/befolkning-og-valg/befolkning-og-befolkningsfremskrivning/folketal. Accessed 22 Jul 2018.
Jacobsen BA, Fallingborg J, Rasmussen HH, Nielsen KR, Drewes AM, Puho E, Nielsen GL, Sørensen HT. Increase in incidence and prevalence of inflammatory bowel disease in northern Denmark: a population-based study, 1978–2002. Eur J Gastroenterol Hepatol. 2006;18(6):601–6.
Molodecky NA, Soon IS, Rabi DM, Ghali WA, Ferris M, Chernoff G, Benchimol EI, Panaccione R, Ghosh S, Barkema HW, Kaplan GG. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology. 2012;142(1):46–54.
Burisch J, Jess T, Martinato M, Lakatos PL, ECCO-EpiCom. The burden of inflammatory bowel disease in Europe. J Crohns Colitis. 2013;7(4):322–37.
Filmann N, Rey J, Schneeweiss S, Ardizzone S, Bager P, Bergamaschi G, Koutroubakis I, Lindgren S, Morena Fde L, Moum B, Vavricka SR, Schröder O, Herrmann E, Blumenstein I. Prevalence of anemia in inflammatory bowel diseases in european countries: a systematic review and individual patient data meta-analysis. Inflamm Bowel Dis. 2014;20(5):936–45.
Sullivan SD, Mauskopf JA, Augustovski F, et al. Budget impact analysis-principles of good practice: report of the ISPOR 2012 budget impact analysis good practice II task force. Value Health. 2014;17(1):5–14.
Bhandari S. A hospital-based cost minimization study of the potential financial impact on the UK health care system of introduction of iron isomaltoside 1000. Ther Clin Risk Manag. 2011;7:103–13.
Olejaz M, Nielsen AJ, Rudkjøbing A, Birk HO, Krasnik A, Hernández-Quevedo C. Denmark: health system review. Health systems in transition. 2012;14(2):1–192. Available from: http://www.euro.who.int/__data/assets/pdf_file/0004/160519/e96442.pdf. Accessed 18 Oct 2018.
Acknowledgements
Funding
Sponsorship for this study and the article publication charges were provided by Pharmacosmos A/S.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Richard F. Pollock is a full-time employee of Ossian Health Economics and Communications GmbH, which received consultancy fees to develop the budget impact model and conduct the Danish analysis. Gorden Muduma is a full-time employee of Pharmacosmos A/S, which is the EU marketing authorization holder for iron isomaltoside.
Compliance with Ethics Guidelines
This article does not include any studies of human participants or animals performed by any of the authors.
Data Availability
All data generated or analyzed during this study are included in this published article/as supplementary information files.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced Digital Features
To view enhanced digital features for this article go to https://doi.org/10.6084/m9.figshare.7235048.
Rights and permissions
About this article
Cite this article
Pollock, R.F., Muduma, G. An Economic Evaluation of Iron Isomaltoside 1000 Versus Ferric Carboxymaltose in Patients with Inflammatory Bowel Disease and Iron Deficiency Anemia in Denmark. Adv Ther 35, 2128–2137 (2018). https://doi.org/10.1007/s12325-018-0827-5
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-018-0827-5