Abstract
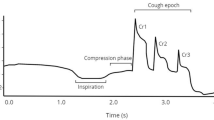
Cerebellar ataxias are neurological conditions with a high prevalence of aspiration pneumonia and dysphagia. Recent research shows that sensorimotor cough dysfunction is associated with airway invasion and dysphagia in other neurological conditions and may increase the risk of pneumonia. Therefore, this study aimed to characterize sensorimotor cough function and its relationship with ataxia severity. Thirty-seven participants with cerebellar ataxia completed voluntary and/or reflex cough testing. Ataxia severity was assessed using the Scale for the Assessment and Rating of Ataxia (SARA). Linear multilevel models revealed voluntary cough peak expiratory flow rate (PEFR) estimates of 2.61 L/s and cough expired volume (CEV) estimates of 0.52 L. Reflex PEFR (1.82 L/s) and CEV (0.34 L) estimates were lower than voluntary PEFR and CEV estimates. Variability was higher for reflex PEFR (15.74% coefficient of variation [CoV]) than voluntary PEFR (12.13% CoV). 46% of participants generated at least two, two-cough responses following presentations of reflex cough stimuli. There was a small inverse relationship between ataxia severity and voluntary PEFR (β = -0.05, 95% CI: -0.09 – -0.01 L) and ataxia severity and voluntary CEV (β = -0.01, 95% CI: -0.02 – -0.004 L/s). Relationships between reflex cough motor outcomes (PEFR β = 0.03, 95% CI: -0.007–0.07 L/s; CEV β = 0.007, 95% CI: -0.004–0.02 L) and ataxia severity were not statistically robust. Results indicate that voluntary and reflex cough sensorimotor dysfunction is present in cerebellar ataxias and that increased severity of ataxia symptoms may impact voluntary cough function.




Similar content being viewed by others
Data Availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Paulson HL. The spinocerebellar ataxias. J Neuroophthalmol. 2009;29(3):227–37.
Abdulmassih EM, da Teive S, Santos HAG. The evaluation of swallowing in patients with spinocerebellar ataxia and oropharyngeal dysphagia: a comparison study of videofluoroscopic and sonar doppler. Int Arch Otorhinolaryngol. 2013;17(1):66–73.
Isono C, Hirano M, Sakamoto H, Ueno S, Kusunoki S, Nakamura Y. Differences in dysphagia between spinocerebellar ataxia type 3 and type 6. Dysphagia. 2013;28(3):413–8.
Isono C, Hirano M, Sakamoto H, Ueno S, Kusunoki S, Nakamura Y. Progression of dysphagia in spinocerebellar ataxia type 6. Dysphagia. 2017;32(3):420–6.
Jardim LB, Pereira ML, Silveira I, Ferro A, Sequeiros J, Giugliani R. Neurologic findings in machado-joseph Disease: relation with Disease duration, subtypes, and (cag)n. Arch Neurol. 2001;58(6):899–904.
Rönnefarth M, Hanisch N, Brandt AU, Mähler A, Endres M, Paul F, et al. Dysphagia affecting quality of life in cerebellar ataxia—a large survey. Cerebellum. 2020;19(3):437–45.
Takahashi H, Ishikawa K, Tsutsumi T, Fujigasaki H, Kawata A, Okiyama R, et al. A clinical and genetic study in a large cohort of patients with spinocerebellar ataxia type 6. J Hum Genet. 2004;49(5):256–64.
Almirall J, Rofes L, Serra-Prat M, Icart R, Palomera E, Arreola V, et al. Oropharyngeal dysphagia is a risk factor for community-acquired Pneumonia in the elderly. Eur Respir J. 2013;41(4):923–8.
Rüb U, Brunt ER, Petrasch-Parwez E, Schöls L, Theegarten D, Auburger G, et al. Degeneration of ingestion-related brainstem nuclei in spinocerebellar ataxia type 2, 3, 6 and 7. Neuropathol Appl Neurobiol. 2006;32(6):635–49.
Pitts T, Bolser D, Rosenbek J, Troche M, Sapienza C. Voluntary cough production and swallow dysfunction in Parkinson’s Disease. Dysphagia. 2008;23(3):297–301.
Tabor-Gray LC, Gallestagui A, Vasilopoulos T, Plowman EK. Characteristics of impaired voluntary cough function in individuals with Amyotrophic Lateral Sclerosis. Amyotroph Lateral Scler Frontotemporal Degeneration. 2019;20(1–2):37–42.
Troche MS, Schumann B, Brandimore AE, Okun MS, Hegland KW. Reflex cough and Disease duration as predictors of swallowing dysfunction in Parkinson’s Disease. Dysphagia. 2016;31(6):757–64.
Fusco AF, Pucci LA, Switonski PM, Biswas DD, McCall AL, Kahn AF et al. Respiratory dysfunction in a mouse model of spinocerebellar ataxia type 7. Dis Models Mech 2021; 14(7).
Borders JC, Brandimore AE, Troche MS. Variability of voluntary cough airflow in healthy adults and Parkinson’s Disease. Dysphagia. 2021;36(4):700–6.
Shah VV, Rodriguez-Labrada R, Horak FB, McNames J, Casey H, Hansson Floyd K, et al. Gait variability in spinocerebellar ataxia assessed using wearable inertial sensors. Mov Disord. 2021;36(12):2922–31.
Schmitz-Hübsch T, Montcel ST, du, Baliko L, Berciano J, Boesch S, Depondt C, et al. Scale for the assessment and rating of ataxia: development of a new clinical scale. Neurology. 2006;66(11):1717–20.
Vovk A, Bolser DC, Hey JA, Danzig M, Vickroy T, Berry R, et al. Capsaicin exposure elicits complex airway defensive motor patterns in normal humans in a concentration-dependent manner. Pulm Pharmacol Ther. 2007;20(4):423–32.
Davenport PW, Clinical Cough I. The Urge-To-Cough: a respiratory sensation. In: Chung KF, Widdicombe J, editors. Eds. Pharmacology and therapeutics of Cough. Berlin, Heidelberg: Springer; 2009. pp. 263–76. (Handbook of Experimental Pharmacology).
Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14(5):377–81.
Slovarp LJ, Bozarth E. Altering cough reflex sensitivity with aerosolized capsaicin paired with behavioral cough suppression: a proof-of-concept study. Ann Transl Med. 2019;7(1):7.
Dicpinigaitis PV. Experimentally induced cough. Pulm Pharmacol Ther. 2007;20(4):319–24.
Fleiss JL, Cohen J, Everitt BS. Large sample standard errors of kappa and weighted kappa. Psychol Bull. 1969;72(5):323–7.
Hegland K, Troche M, Davenport P. Cough expired volume and airflow rates during sequential induced cough. Front Physiol 2013; 4.
Jekel JF. Should we stop using the P value in descriptive studies? Pediatrics. 1977;60(1):124–6.
R Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing. 2023. Available from: https://www.R-project.org/.
Bates D, Mächler M, Bolker B, Walker S. Fitting linear mixed-effects models using lme4. 2015. https://doi.org/10.18637/jss.v067.i01.
Lenth R. emmeans: Estimated marginal means, aka least-squares means. 2023.
Dickson RP, Erb-Downward JR, Martinez FJ, Huffnagle GB. The microbiome and the respiratory tract. Annu Rev Physiol. 2016;78:481–504.
Hegland KW, Okun MS, Troche MS. Sequential voluntary cough and aspiration or aspiration risk in Parkinson’s Disease. Lung. 2014;192(4):601–8.
Troche MS, Brandimore AE, Okun MS, Davenport PW, Hegland KW. Decreased cough sensitivity and aspiration in Parkinson Disease. Chest. 2014;146(5):1294–9.
Brandimore AE, Troche MS, Huber JE, Hegland KW. Respiratory kinematic and airflow differences between reflex and voluntary cough in healthy young adults. Front Physiol 2015; 6.
Borders JC, Sevitz JS, Curtis JA, Vanegas-Arroyave N, Troche MS. Sensorimotor cough dysfunction is prevalent and pervasive in Progressive supranuclear palsy. Mov Disord. 2021;36(11):2624–33.
Schalling E, Hammarberg B, Hartelius L. Perceptual and acoustic analysis of speech in individuals with spinocerebellar ataxia (SCA). Logopedics Phoniatrics Vocology. 2007;32(1):31–46.
Schalling E, Hartelius L. Acoustic analysis of speech tasks performed by three individuals with spinocerebellar ataxia. Folia Phoniatr Logop. 2004;56(6):367–80.
Davenport PW. Urge-to-cough: what can it teach us about cough? Lung. 2008;186(1):107–11.
Smith JA, Aliverti A, Quaranta M, McGuinness K, Kelsall A, Earis J, et al. Chest wall dynamics during voluntary and induced cough in healthy volunteers. J Physiol. 2012;590(Pt 3):563–74.
Borders J, Troche M. Voluntary cough effectiveness and airway clearance in neurodegenerative Disease. J Speech Lang Hear Res. 2021;65:1–19.
Troche MS, Curtis JA, Sevitz JS, Dakin AE, Perry SE, Borders JC, et al. Rehabilitating cough dysfunction in Parkinson’s Disease: a randomized controlled trial. Mov Disord. 2023;38(2):201–11.
Biswas DD, El Haddad L, Sethi R, Huston ML, Lai E, Abdelbarr MM, et al. Neuro-respiratory pathology in spinocerebellar ataxia. J Neurol Sci. 2022;443:120493.
Shannon R, Baekey DM, Morris KF, Nuding SC, Segers LS, Lindsey BG. Production of reflex cough by brainstem respiratory networks. Pulm Pharmacol Ther. 2004;17(6):369–76.
Hegland KW, Bolser DC, Davenport PW. Volitional control of reflex cough. J Appl Physiol. 2012;113(1):39–46.
Acknowledgements
The authors would like to thank our colleagues at the Laboratory for the Study of Upper Airway Dysfunction at Teachers College, Columbia University and the Department of Neurology at Columbia University Medical Center for their help with the recruitment of patients. We also thank our participants for their contribution to this research.
Author information
Authors and Affiliations
Contributions
(1) Research Project: (A) Conception, (B) Organization, (C) Execution. (2) Statistical Analysis: (A) Design, (B) Execution, (C) Review and Critique. (3) Manuscript: (A) Writing of the First Draft, (B) Review and Critique. E.R.L.: 1A, 1B, 1C, 2A, 2B, 2C, 3A, 3B. J.C.B: 1A, 1B, 1C, 2A, 2B, 2C, 3A, 3B. S.H.K.: 1A, 1B, 1C, 2C, 3A, 3C. S.E.P.: 1A, 1B, 1C, 2C, 3A, 3C. A.E.D.: 1A, 1B, 1C, 2C, 3A, 3C. J.S.S.: 1A, 1B, 1C, 2C, 3A, 3C. M.S.T.: 1A, 1B, 2A, 2C, 3A, 3B, 3C.
Corresponding author
Ethics declarations
Conflict of Interest
S.E.P. receives grant funding/salary for employment at the University of Otago/Neurological Foundation of New Zealand. S.H.K receives salary for employment at Columbia University, and serves on advisory boards for Praxis, Sage Therapeutics, Reata, and Biohaven. M.S.T. receives salary for employment at Teachers College, Columbia University, grant funding from NIH/NINDS, and royalties for consulting at MedBridge. M.S.T. also serves as a board member for the Dysphagia Research Society. No other authors have financial disclosures or conflicts of interest to report.
Ethics Approval
The studies included in this manuscript were approved by the institutional review board of Teachers College at Columbia University (19–321, 15–430). We confirm that we have read the Journal’s position on issues involved in ethical publication and affirm that this work is consistent with those guidelines.
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Consent for Publication
Participants signed informed consent regarding publishing their data.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lowell, E.R., Borders, J.C., Perry, S.E. et al. Sensorimotor Cough Dysfunction in Cerebellar Ataxias. Cerebellum (2023). https://doi.org/10.1007/s12311-023-01635-0
Accepted:
Published:
DOI: https://doi.org/10.1007/s12311-023-01635-0