Abstract
The purpose of this study was to assess the impact of COVID-19 on long-term outcomes in the geriatric hip fracture population. We hypothesize that COVID + geriatric hip fracture patients had worse outcomes at 1-year follow-up. Between February and June 2020, 224 patients > 55 years old treated for a hip fracture were analyzed for demographics, COVID status on admission, hospital quality measures, 30- and 90-day readmission rates, 1-year functional outcomes (as measured by the EuroQol- 5 Dimension [EQ5D-3L] questionnaire), and inpatient, 30-day, and 1-year mortality rates with time to death. Comparative analyses were conducted between COVID + and COVID- patients. Twenty-four patients (11%) were COVID + on admission. No demographic differences were seen between cohorts. COVID + patients experienced a longer length of stay (8.58 ± 6.51 vs. 5.33 ± 3.09, p < 0.01) and higher rates of inpatient (20.83% vs. 1.00%, p < 0.01), 30-day (25.00% vs. 5.00%, p < 0.01), and 1-year mortality (58.33% vs. 18.50%, p < 0.01). There were no differences seen in 30- or 90-day readmission rates, or 1-year functional outcomes. While not significant, COVID + patients had a shorter average time to death post-hospital discharge (56.14 ± 54.31 vs 100.68 ± 62.12, p = 0.171). Pre-vaccine, COVID + geriatric hip fracture patients experienced significantly higher rates of mortality within 1 year post-hospital discharge. However, COVID + patients who did not die experienced a similar return of function by 1-year as the COVID- cohort.
Similar content being viewed by others
Introduction
Since the first case arose in late 2019, the COVID-19 pandemic has spread across the globe and caused significant strain to the global healthcare system. Case totals across the world have since risen to over 400 million people, more than 5 million of which have resulted in death [1]. Since the first case in January 2020, the United States case total has risen to over 77 million individuals with over 900,000 deaths [2].
While the overall incidence of middle-aged and geriatric trauma decreased amidst the height of the initial wave of the pandemic, hip fractures continued to occur at frequency similar to pre-pandemic levels [3]. Notably, these patients have significantly higher rates of morbidity and mortality as compared to before the pandemic. Patients who sustained hip fractures within the first months of the pandemic experienced drastically increased rates of inpatient mortality, 30-day mortality, longer hospital stays with higher rates of inpatient complications and worse functional outcomes [4,5,6,7,8,9,10,11,12,13,14]. This was most pronounced in patients that tested positive for COVID on admission. The long-term implications of COVID infection in middle-aged and geriatric hip fracture patients are not well described. The purpose of this study was to assess the impact of COVID-19 on long-term outcomes in the middle-aged and geriatric hip fracture population. To our knowledge, this is the first study to do so. We hypothesize that COVID + hip fracture patients in these populations had worse outcomes at 1-year follow-up.
Methods
This is a prospective observational cohort study following previously published work that evaluated the inpatient and 30-day outcomes of hip fracture patients treated during the initial months of the COVID-19 pandemic. An Institutional Review Board-approved geriatric trauma database was queried for the following inclusion criteria: all patients aged 55 or older who sustained a hip fracture (femoral neck, intertrochanteric, and subtrochanteric fracture [AO/OTA fracture classifications: 31A, 31B, 32(A-C)]) via a low-energy mechanism (fall from standing or height < 2 stairs) between February–May 2020. Exclusion criteria included all patients younger than 55 years old and those who did not have complete data. Patients were recruited from one academic medical center in a large urban setting that includes four American College of Surgeons verified Level 1 trauma centers, one university-based tertiary care referral hospital, and one orthopedic specialty hospital. Patients included in this study were treated at one of these six hospitals.
Data collected included demographics, COVID status on admission, hospital quality measures, discharge locations, readmissions, inpatient (defined as patients who passed away during their index hospitalization), 30-day and 1-year mortality, and 1-year functional outcomes (as measured by the EuroQol- 5 Dimension [EQ5D-3L] questionnaire). Patients were contacted by phone to complete the EQ5D-3L questionnaires on functional status along with their respective visual analog scores (VAS). A validated inpatient mortality risk assessment score—Score for Trauma Triage of Geriatric and Middle Age patients (STTGMA)—was calculated for each patient. Patients were identified as COVID-19 positive if they had a positive COVID-19 RT-PCR test at the time of their admission to the hospital. For study analysis, patients were divided into a COVID + and a COVID- cohort. A sub-analysis compared the survivors within each cohort at the 1-year time point. Another sub-analysis was conducted comparing the hospital quality measures, and long-term functional and mortality outcomes between patients stratified by cohorts based on the treatment they received for their injury.
Univariate analyses were conducted between each cohort using Chi Square, Mann-Whitney U tests, and Independent Sample T-Tests as appropriate. Multivariable logistic regression was used to assess the impact of COVID + status on 1-year mortality. Kaplan–Meier survival curves were constructed for both the COVID + and COVID- cohorts.
All statistics were calculated with IBM SPSS data software, Version 25 (Armonk, NY). Significance was set at an alpha of 0.05.
Results
Between February 2020 and May 2020 there were 224 patients treated for a hip fracture that were age 55 or older. Twenty-four patients (11.00%) were COVID + on admission to the hospital at the time of their injury. There were 86 men (38%) and 138 women (62%). The majority of patients were white (80%). Mean age was 81.25 ± 10.00 years [COVID + Age Range: 60–95, COVID- Age Range: 55–100]. Mean BMI was 24.38 ± 5.77. Mean Charlson Comorbidity Index (CCI) was 1.38 ± 1.55. Mean American Society of Anesthesiology Score (ASA) was 2.88 ± 0.74. At baseline, 60% of patients were community ambulators, 38% of patients were household ambulators, and 2% were non-ambulatory. The majority of patients sustained either a 31A (55%) or 31B (44%) fracture as classified by AO/OTA guidelines [15]. Patients were treated with: short cephalomedullary nail (37%), long cephalomedullary nail (18%), hemiarthroplasty (24%), total hip arthroplasty (7%), sliding hip screw (4%), closed reduction percutaneous pinning (CRPP) (9%) or non-operatively (3%). Most patients (67%) were discharged to an acute rehabilitation or skilled nursing facility, while 32% of patients were discharged home independently or home with health services.
COVID + patients were more likely to be non-ambulatory or wheelchair-bound with a worse baseline ambulatory status (12.50% vs. 2.00%, p < 0.01), more likely to undergo nonoperative treatment (20.83% vs. 2.50%, p < 0.01), as well as more likely to die during index hospitalization or be discharged to hospice (20.83% vs. 1.50%, p < 0.01). COVID- patients were more likely to be discharged home independently or with health services (32.00% vs. 8.33%, p = 0.016). There was no difference in age, BMI, gender, race, CCI, or ASA between cohorts (Table 1).
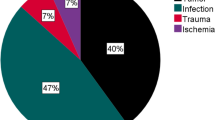
COVID + patients had significantly longer lengths of hospital stay (8.58 ± 6.51 vs. 5.33 ± 3.09, p < 0.01) and higher rates of inpatient (20.83% vs. 1.00%, p < 0.01), 30-day (25.00% vs. 5.00%, p < 0.01), and 1-year mortality (58.33% vs. 18.50%, p < 0.01) as compared to COVID- patients (Fig. 1). While not significant, COVID + patients experienced a shorter average post-discharge time to death (56.14 ± 54.31 vs. 100.68 ± 62.12, p = 0.077).
Rates of 30- day (12.50% vs. 7.50%, p = 0.392) and 90-day readmission (12.50% vs. 11.00%, p = 0.996) were similar between cohorts. COVID + patients were ~ 2 × more likely to require ICU level care (29.17% vs. 14.00%, p = 0.053). Finally, 1-year functional outcomes including EQ-5D index score (0.71 ± 0.35 vs. 0.70 ± 0.43, p = 0.982) and VAS score (72.14 ± 33.91 vs. 72.30 ± 37.85, p = 0.866) were similar between cohorts (Table 2). There was no difference in mean time to surgery (in days) between cohorts.
COVID + patients that died within 1-year were found to have a higher CCI as compared to COVID + patients that survived through 1-year (2.21 ± 1.42 vs. 1.00 ± 1.16, p = 0.037).
A multivariable logistical regression model was generated to examine whether COVID positivity on admission and other clinical and demographic data were independently associated with an increased rate of 1-year mortality. COVID + status on admission (OR 5.701, 95% CI 2.116–15.359, p < 0.01), older age (OR 1.044, 95% CI 1.002–1.089, p = 0.042), and a higher CCI (OR 1.335, 95% CI 1.058–1.686, p = 0.015) were found to be independent risk factors for 1-year mortality. Female gender was found to be independently protective against 1-year mortality in this cohort (OR 0.320, 95% CI 0.157–0.651, p < 0.01) (Table 3).
Sub-analysis comparing COVID + and COVID- survivors demonstrated COVID + survivors had higher STTGMA scores (14.73 ± 18.06 vs. 1.05 ± 1.92, p < 0.01), longer lengths of stay (10.10 ± 9.01 vs. 4.99 ± 2.42, p = 0.014), and inpatient hospital complications (80.00% vs. 34.97%, p < 0.01). At 1-year, there was no significant difference in the change in assistive device needed from baseline (for example, wheelchair to walker or vice versa, walker to cane or vice versa, etc.) between cohorts (Table 4).
Sub-analysis comparing patients within each treatment group demonstrated patients treated non-operatively had higher rates of mortality as compared to those who underwent operative fixation. Patients treated with a total hip arthroplasty had the lowest mortality rates and best long-term functional outcomes (Table 5).
Discussion
The purpose of this study was to investigate the impact of COVID-19 infection on long-term outcomes in the middle-aged and geriatric hip fracture population. Hip fractures alone carry significant morbidity and mortality, especially in the geriatric population [16]. Therefore, the long-term implications of concomitant hip fracture and COVID-19 infection in these populations remain a significant public healthcare concern. No study to date has assessed outcomes past 6-months in the middle-aged and geriatric hip fracture population. Our study demonstrated higher rates of mortality in COVID + patients out to the 1-year mark, however, those who survived experienced a similar return to function and health status at 1 year as COVID- patients.
High rates of inpatient and 30-day mortality, longer hospital stays, and poor short-term functional outcomes for geriatric hip fracture patients infected with COVID-19 are well-documented in the literature and reflected in this group’s previous study [4]. Our study demonstrates that the increase in short-term mortality seen in COVID + patients extends to the 1-year mark, with a mortality rate approaching 60% in our cohort. The cause of this higher mortality rate is likely multifactorial. Infection with COVID-19 is the most significant risk factor. COVID + patients in our cohort had a 20 × higher inpatient mortality rate, 5 × higher 30-day mortality rate, and more than 3 × higher rate of 1-year mortality than COVID- patients. 1-year survival, therefore, was roughly 42% and 82% for both cohorts, respectively. Multivariable analysis supports this finding with COVID positivity on admission being a statistically significant factor in 1-year mortality.
In this study, COVID + patients who died within 1-year had a higher CCI at baseline as compared to COVID + patients who survived, highlighting the higher mortality risk in patients with more severe comorbidity profiles. It is well documented that COVID infection in patients with higher comorbidity burden have more severe physiologic sequelae and morbidity. For example, patients with pre-existing lung disease (e.g., COPD, asthma) are more likely to require mechanical ventilation and are therefore more prone to developing pneumonia and further respiratory compromise [17, 18].
Additionally, patients with pre-existing cardiovascular disease (e.g., heart failure, coronary artery disease) may be more at risk for viral infection extending to the cardiac tissue, allowing for direct cardiac injury or subsequent cardiomyopathies [19]. Regardless of a patient’s comorbidity profile, studies have found that patients previously infected with COVID-19 may have lasting effects including cardiac sequelae, neurological symptoms, acute kidney injury, osteoporosis, and various psychological pathologies such as depression, anxiety, and post-traumatic stress disorder [20,21,22,23,24,25]. In this middle-aged and geriatric population, infection with COVID-19 can both worsen pre-existing conditions and trigger additional long-term complications which patients may eventually succumb to.
This study found age and increased CCI to be independent risk factors for 1-year mortality, while female gender was found to be a protective factor. This corresponds with findings prior to the pandemic as older age and a more extensive comorbidity profile are directly related to higher risk of 1-year mortality following a hip fracture [26]. Pre-pandemic studies also show male gender to be a risk factor, with female gender reciprocally being protective for 1-year mortality [27]. This may reflect worse comorbidity profiles or less physiologic reserve seen in males. These trends have persisted amidst the pandemic with literature demonstrating age, male gender, and a worse comorbidity profile increase risk of 1-year mortality, especially in the COVID + population [28].
Among survivors, 1-year functional outcomes were nearly equivalent between COVID + and COVID- cohorts. A subgroup analysis of these survivors demonstrated no difference in age or CCI but a much higher STTGMA score in the COVID + patients. This is due to the composite STTGMA score accounting for their COVID + status on admission—highlighting a higher risk of inpatient mortality. Longer lengths of stay and higher rates of inpatient complication despite nearly equivalent 1-year functional outcomes demonstrate that although these patients may experience a more challenging initial infection and recovery course, over time they recover the same functional status as COVID- patients.
It is also possible that patients who survived up to 1-year may have had a milder infectious course, mitigating the potential health complications and functional limitations associated with severe COVID-19 infection. The ability for COVID + patients to return to a similar level of function as compared to COVID- patients is debated in the literature. One study highlighted a reduced exercise capacity in the form of mean walking distance even months after infection [29]. However, another study demonstrates a similar return to function as seen in our study for COVID + patients that undergo inpatient rehabilitation after their infectious course, with these patients achieving a similar functional status despite worse condition when they started rehabilitation [30].
Our study found differences in functional outcomes and mortality between patients in each of the various treatment groups. Most notably, patients who were treated non-operatively had higher rates of mortality and readmission while patients treated with total hip arthroplasty had lower rates of mortality and better functional outcomes at the 1-year mark. However, it is important to acknowledge patients treated non-operatively who survived out to the 1-year mark were able to recover and attain good functional outcomes. While these differences in outcome are apparent between the treatment groups, the reason is likely that sicker patients were treated non-operatively, while less sick patients were treated with total hip arthroplasty as is usually the case in treatment selection.
This study has several limitations. First, our overall cohort only included patients from the first few months of the pandemic. Therefore, the 1-year outcomes experienced by these patients amidst the early stages of the pandemic might not be generalizable across the entire pandemic’s duration. Second, we do not know the duration of facility or home rehabilitation each patient received postoperatively, therefore we cannot correlate outcomes based on the functional level patients reached before completion of their rehabilitation regiment. As the pandemic continues to evolve and treatment modalities improve, additional studies must be conducted to assess the long-term outcomes in COVID + hip fracture patients.
In conclusion, the first wave of COVID + middle-aged and geriatric hip fracture patients experienced significantly higher rates of mortality up to 1 year. However, COVID + patients who did not die experienced a similar return to 1-year functionality as the COVID- cohort. These data are useful in understanding the long-term effects of COVID + infection in the early stages of the pandemic in this hip fracture population. As COVID infection had no effect on outcomes other than death, we recommend no changes in workflow or hip fracture protocols as waves of the disease may progress. With the vaccine demonstrating efficacy in preventing death, it is hoped that the expected mortality following hip fracture care will return to historic levels.
References
World Health Organization. WHO Coronavirus 2022 [Internet]. 2022. Available from: https://covid19.who.int/.
Center for Disease Control and Prevention. CDC Coronavirus 2022 [Internet]. 2022. Available from: https://covid.cdc.gov/covid-data-tracker/?CDC_AA_refVal=https%3A//www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html#demographicsovertime.
Haskel JD, Lin CC, Kaplan DJ, Dankert JF, Merkow D, Crespo A et al (2020) Hip fracture volume does not change at a New York City Level 1 trauma center during a period of social distancing. Geriatr Orthop Surg Rehabil 11:2151459320972674
Egol KA, Konda SR, Bird ML, Dedhia N, Landes EK, Ranson RA et al (2020) Increased mortality and major complications in hip fracture care during the COVID-19 pandemic: a New York City perspective. J Orthop Trauma 34(8):395–402
LeBrun DG, Konnaris MA, Ghahramani GC, Premkumar A, DeFrancesco CJ, Gruskay JA et al (2020) hip fracture outcomes during the COVID-19 pandemic: early results from New York. J Orthop Trauma 34(8):403–410
Hall AJ, Clement ND, Farrow L, MacLullich AMJ, Dall GF, Scott CEH et al (2020) IMPACT-Scot report on COVID-19 and hip fractures. Bone Joint J. 102(9):1219–28
Crozier-Shaw G, Hughes AJ, Conlon B, Sheehan E, Merghani K (2021) Hip fracture care during Covid-19: a regional trauma centre’s experience. Ir J Med Sci 190(4):1275–1280
Biarnés-Suñé A, Solà-Enríquez B, González Posada MÁ, Teixidor-Serra J, García-Sánchez Y, Manrique MS (2021) Impact of the COVID-19 pandemic on the mortality of the elderly patient with a hip fracture. Rev Esp Anestesiol Reanim (Engl Ed) 68(2):65–72
Hadfield JN, Gray AC (2020) The evolving COVID-19 effect on hip fracture patients. Injury 51(7):1411–1412
Mahmood A, Rashid F, Limb R, Cash T, Nagy MT, Zreik N et al (2021) Coronavirus infection in hip fractures (CHIP) study. Bone Joint J. 103(4):782–7
Lim MA, Pranata R (2021) Coronavirus disease 2019 (COVID-19) markedly increased mortality in patients with hip fracture - A systematic review and meta-analysis. J Clin Orthop Trauma 12(1):187–193
Wang KC, Xiao R, Cheung ZB, Barbera JP, Forsh DA (2020) Early mortality after hip fracture surgery in COVID-19 patients: a systematic review and meta-analysis. J Orthop 22:584–591
Zhong H, Poeran J, Liu J, Wilson LA, Memtsoudis SG (2021) Hip fracture characteristics and outcomes during COVID-19: a large retrospective national database review. Br J Anaesth 127(1):15–22
Onizuka N, Topor LN, Schroder LK, Switzer JA (2021) Outcomes of COVID-19 negative hip fracture patients during the acute and subacute pandemic. Geriatr Orthop Surg Rehabil 12:21514593211006692
Meinberg E, Agel J, Roberts C, Karam M, Kellam J (2018) Fracture and dislocation classification compendium—2018. J Orthop Trauma 32(1):S1-10
Holt G, Smith R, Duncan K, Hutchison JD, Gregori A (2008) Outcome after surgery for the treatment of hip fracture in the extremely elderly. J Bone Joint Surg Am 90(9):1899–1905
Zhao Q, Meng M, Kumar R, Wu Y, Huang J, Lian N et al (2020) The impact of COPD and smoking history on the severity of COVID-19: A systemic review and meta-analysis. J Med Virol 92(10):1915–1921
Higham A, Mathioudakis A, Vestbo J, Singh D (2020) COVID-19 and COPD: a narrative review of the basic science and clinical outcomes. Eur Respir Rev 29(158):200199
Bader F, Manla Y, Atallah B, Starling RC (2021) Heart failure and COVID-19. Heart Fail Rev 26(1):1–10
Sheehy LM (2020) Considerations for postacute rehabilitation for survivors of COVID-19. JMIR Public Health Surveill 6(2):e19462
Shi S, Qin M, Shen B, Cai Y, Liu T, Yang F et al (2020) Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan. China JAMA Cardiol 5(7):802–810
McNeary L, Maltser S, Verduzco-Gutierrez M (2020) Navigating coronavirus disease 2019 (Covid-19) in physiatry: a CAN report for inpatient rehabilitation facilities. PM R 12(5):512–515
Wang L, He W, Yu X, Hu D, Bao M, Liu H et al (2020) Coronavirus disease 2019 in elderly patients: characteristics and prognostic factors based on 4-week follow-up. J Infect 80(6):639–645
Herridge MS, Moss M, Hough CL, Hopkins RO, Rice TW, Bienvenu OJ et al (2016) Recovery and outcomes after the acute respiratory distress syndrome (ARDS) in patients and their family caregivers. Intensive Care Med 42(5):725–738
Li YM, Wang SX, Gao HS, Wang JG, Wei CS, Chen LM et al (2004) Factors of avascular necrosis of femoral head and osteoporosis in SARS patients’ convalescence. Zhonghua yi xue za zhi 84(16):1348–1353
Menéndez-Colino R, Alarcon T, Gotor P, Queipo R, Ramírez-Martín R, Otero A et al (2018) Baseline and pre-operative 1-year mortality risk factors in a cohort of 509 hip fracture patients consecutively admitted to a co-managed orthogeriatric unit (FONDA Cohort). Injury 49(3):656–661
Guzon-Illescas O, Perez Fernandez E, CrespíVillarias N, Quirós Donate FJ, Peña M, Alonso-Blas C et al (2019) Mortality after osteoporotic hip fracture: incidence, trends, and associated factors. J Orthop Surg Res 14(1):203
Gao YD, Ding M, Dong X, Zhang JJ, KursatAzkur A, Azkur D et al (2021) Risk factors for severe and critically ill COVID-19 patients: a review. Allergy 76(2):428–455
Ahmed H, Patel K, Greenwood DC, Halpin S, Lewthwaite P, Salawu A et al (2020) Long-term clinical outcomes in survivors of severe acute respiratory syndrome and Middle East respiratory syndrome coronavirus outbreaks after hospitalisation or ICU admission: A systematic review and meta-analysis. J Rehabil Med. 52(5):jrm00063
Abramoff BA, Dillingham TR, Caldera FE, Ritchie MD, Pezzin LE (2021) Inpatient Rehabilitation Outcomes After Severe COVID-19 Infections: A Retrospective Cohort Study. Am J Phys Med Rehabil 100(12):1109–1114
Acknowledgements
Not applicable.
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare they have no conflict of interest.
Ethical approval
This retrospective chart review study involving human participants was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Human Investigation Committee (IRB) of NYU Langone approved this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Konda, S.R., Esper, G.W., Meltzer-Bruhn, A.T. et al. One year later: How outcomes of hip fractures treated during the “first wave” of the COVID-19 pandemic were affected. Musculoskelet Surg 107, 405–412 (2023). https://doi.org/10.1007/s12306-023-00784-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12306-023-00784-z