Abstract
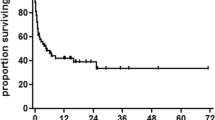
Outcomes of patients with hematologic malignancies requiring ICU care for critical illness are suboptimal and represent a major unmet need in this population. We present data from a dedicated haematology oncology setting including 63 patients with a median age of 60 years admitted to the ICU for critical illness with organ dysfunction. The most common underlying diagnosis was multiple myeloma (30%) followed by acute myeloid leukemia (25%). Chemotherapy had been initiated for 90.7% patients before ICU admission. The most common indication for ICU care was respiratory failure (36.5%) and shock (17.5%) patients. Evidence of sepsis was present in 44 (69%) patients. After shifting to ICU, 32 (50%) patients required inotropic support and 18 (28%) required invasive mechanical ventilation. After a median of 5 days of ICU stay, 43.1% patients had died, most commonly due to multiorgan dysfunction. Risk of mortality was higher with involvement of more than two major organs (p = .001), underlying AML (p = .001), need for mechanical ventilation (p = .001) and high inotrope usage (p = .004). Neutropenia was not associated with mortality. Our study indicates high rates of short term mortality and defines prognostic factors which can be used to prognosticate patients and establish goals of care.




Similar content being viewed by others
References
Taccone FS, Artigas AA, Sprung CL, Moreno R, Sakr Y, Vincent J-L (2009) Characteristics and outcomes of cancer patients in European ICUs. Crit Care 13(1):R15
Lloyd-Thomas AR, Wright I, Lister TA, Hinds CJ (1988) Prognosis of patients receiving intensive care for lifethreatening medical complications of haematological malignancy. Br Med J (Clin Res Ed) 296(6628):1025–1029
Manjappachar NK, Cuenca JA, Ramírez CM, Hernandez M, Martin P, Reyes MP et al (2022) Outcomes and predictors of 28-day mortality in patients with hematologic malignancies and septic shock defined by sepsis-3 criteria. J Natl Compr Canc Netw 20(1):45–53
Buchman TG, Simpson SQ, Sciarretta KL, Finne KP, Sowers N, Collier M et al (2020) Sepsis among medicare beneficiaries: 1. The burdens of sepsis, 2012-2018. Crit Care Med 48(3):276–88
Hawari FI, Nazer LH, Addassi A, Rimawi D, Jamal K (2016) Predictors of ICU admission in patients with cancer and the related characteristics and outcomes: a 5-year registry-based study. Crit Care Med 44(3):548–553
Kubihal V, Chandrashekhara SH, Triveni GS (2022) Clinical imaging in oncological ICU. In: Kumar V, Gupta N, Mishra S (eds) Onco-critical care: an evidence-based approach. Springer Nature Singapore, Singapore, pp 37–50
Williams MD, Braun LA, Cooper LM, Johnston J, Weiss RV, Qualy RL et al (2004) Hospitalized cancer patients with severe sepsis: analysis of incidence, mortality, and associated costs of care. Crit Care (London, England) 8(5):R291–R298
Brunet F, Lanore JJ, Dhainaut JF, Dreyfus F, Vaxelaire JF, Nouira S et al (1990) Is intensive care justified for patients with haematological malignancies? Intensive Care Med 16(5):291–297
Evison J, Ritz R, Elsasser S (2001) Intensive care unit admission in patients with hematological disease: incidence, outcome and prognostic factors. Swiss Med Wkly 131(4748):681–686
Owczuk R, Wujtewicz MA, Sawicka W, Wadrzyk A, Wujtewicz M (2005) Patients with haematological malignancies requiring invasive mechanical ventilation: differences between survivors and non-survivors in intensive care unit. Support Care Cancer: Off J Multinatl Assoc Support Care Cancer 13(5):332–338
Gordon AC, Oakervee HE, Kaya B, Thomas JM, Barnett MJ, Rohatiner AZ et al (2005) Incidence and outcome of critical illness amongst hospitalised patients with haematological malignancy: a prospective observational study of ward and intensive care unit based care. Anaesthesia 60(4):340–347
Senapati J, Dhawan R, Aggarwal M, Kumar P, Kumar Vishwanathan G, Dass J et al (2021) Venetoclax and azacitidine (VenAZA) combination therapy in young unfit patients with AML: a perspective from a developing country. Leuk Lymphoma 62(6):1514–1517
Jobanputra KN, Nayak L, Jain H, Sengar DM (2021) Diffuse large B-cell lymphoma in the elderly: retrospective analysis from a single tertiary cancer center in India. Blood 138:2515
Shaikh MRMA, Mehta P, Mirgh SP, Halder R, Agrawal N, Khushoo V et al (2021) Individualized AML induction with venetoclax based therapy in unfit treatment naïve patients aged ≤ 60 years: a real world perspective from India. Blood 138:4417
Hammond NE, Kumar A, Kaur P, Tirupakuzhi Vijayaraghavan BK, Ghosh A, Grattan S et al (2022) Estimates of sepsis prevalence and outcomes in adult patients in the ICU in India: a cross-sectional study. Chest 161(6):1543–1554
Chaudhry D, Prajapat B (2017) Intensive care unit bugs in India: How do they differ from the western world? J Assoc Chest Phys 5(1):10–17
Philip C, George B, Ganapule A, Korula A, Jain P, Alex AA et al (2015) Acute myeloid leukaemia: challenges and real world data from India. Br J Haematol 170(1):110–117
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M et al (2016) The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 315(8):801–810
Peerapornratana S, Manrique-Caballero CL, Gómez H, Kellum JA (2019) Acute kidney injury from sepsis: current concepts, epidemiology, pathophysiology, prevention and treatment. Kidney Int 96(5):1083–1099
Cheung AK, Chang TI, Cushman WC, Furth SL, Hou FF, Ix JH et al (2021) KDIGO 2021 clinical practice guideline for the management of blood pressure in chronic kidney disease. Kidney Int 99(3):S1–S87
Franco L, Becattini C, Beyer-Westendorf J, Vanni S, Nitti C, Re R et al (2020) Definition of major bleeding: prognostic classification. J Thromb Haemost 18(11):2852–2860
Zimmer AJ, Freifeld AG (2019) Optimal management of neutropenic fever in patients with cancer. J Oncol Pract 15(1):19–24
Donnelly JP, Chen SC, Kauffman CA, Steinbach WJ, Baddley JW, Verweij PE et al (2019) Revision and update of the consensus definitions of invasive fungal disease from the European organization for research and treatment of cancer and the mycoses study group education and research consortium. Clin Infect Dis 71(6):1367–1376
Belletti A, Lerose CC, Zangrillo A, Landoni G (2021) Vasoactive-inotropic score: evolution, clinical utility, and pitfalls. J Cardiothorac Vasc Anesth 35(10):3067–3077
Ferreyro BL, Scales DC, Wunsch H, Cheung MC, Gupta V, Saskin R et al (2021) Critical illness in patients with hematologic malignancy: a population-based cohort study. Intensive Care Med 47(10):1104–1114
de Vries VA, Müller MCA, Arbous MS, Biemond BJ, Blijlevens NMA, Kusadasi N et al (2019) Long-term outcome of patients with a hematologic malignancy and multiple organ failure admitted at the intensive care. Crit Care Med 47(2):e120–e128
Tridente A, Dempsey NC, Khalifa M, Goddard J, Shuker K, Hall J et al (2023) Predicting outcomes of hematological malignancy patients admitted to critical care. Front Hematol 2. https://doi.org/10.3389/frhem.2023.1127322
Siddiqui SS, Prabu NR, Chaudhari HK, Narkhede AM, Sarode SV, Dhundi U et al (2021) Epidemiology, clinical characteristics, and prognostic factors in critically ill patients with hematolymphoid malignancy. Indian J Crit Care Med: Peer-reviewed, Off Publ Indian Soc Crit Care Med 25(1):56–61
Moreno-Sanchez F, Gomez-Gomez B (2022) Antibiotic management of patients with hematologic malignancies: from prophylaxis to unusual infections. Curr Oncol Rep 24(7):835–842
Azoulay E, Recher C, Alberti C, Soufir L, Leleu G, Le Gall JR et al (1999) Changing use of intensive care for hematological patients: the example of multiple myeloma. Intensive Care Med 25(12):1395–1401
Hampshire PA, Welch CA, McCrossan LA, Francis K, Harrison DA (2009) Admission factors associated with hospital mortality in patients with haematological malignancy admitted to UK adult, general critical care units: a secondary analysis of the ICNARC case mix programme database. Crit Care (London, England) 13(4):R137
van Mourik N, Oomen JJ, van Vught LA, Biemond BJ, van den Bergh WM, Blijlevens NM et al (2023) The predictive value of the modified early warning score for admission to the intensive care unit in patients with a hematologic malignancy–a multicenter observational study. Intensive Crit Care Nurs 79:103486
Yoo J-W, Lee JR, Jung YK, Choi SH, Son JS, Kang BJ et al (2015) A combination of early warning score and lactate to predict intensive care unit transfer of inpatients with severe sepsis/septic shock. Korean J Intern Med 30(4):471
Lee JR, Jung YK, Kim HJ, Koh Y, Lim CM, Hong SB et al (2020) Derivation and validation of modified early warning score plus SpO2/FiO2 score for predicting acute deterioration of patients with hematological malignancies. Korean J Intern Med 35(6):1477–1488
Mato A, Fuchs BD, Heitjan DF, Mick R, Halpern SD, Shah PD et al (2009) Utility of the systemic inflammatory response syndrome (SIRS) criteria in predicting the onset of septic shock in hospitalized patients with hematologic malignancies. Cancer Biol Ther 8(12):1095–1100
Mato AR, Luger SM, Heitjan DF, Mikkelson ME, Olson E, Ujjani C et al (2010) Elevation in serum lactate at the time of Febrile Neutropenia (FN) in hemodynamically-stable patients with Hematologic Malignancies (HM) is associated with the development of septic shock within 48 hours. Cancer Biol Ther 9(8):585–589
Nathan N, Sculier JP, Ameye L, Paesmans M, Bogdan-Dragos G, Meert AP (2021) Sepsis and septic shock definitions in patients with cancer admitted in ICU. J Intensive Care Med 36(3):255–261
Yeo CD, Kim JW, Kim SC, Kim YK, Kim KH, Kim HJ et al (2012) Prognostic factors in critically ill patients with hematologic malignancies admitted to the intensive care unit. J Crit Care 27(6):739.e1-739.e6
Cetintepe T, Cetintepe L, Solmaz S, Calık S, Ugur MC, Gediz F et al (2021) Determination of the relationship between mortality and SOFA, qSOFA, MASCC scores in febrile neutropenic patients monitored in the intensive care unit. Support Care Cancer 29(7):4089–4094
Al-Zubaidi N, Shehada E, Alshabani K, ZazaDitYafawi J, Kingah P, Soubani AO (2018) Predictors of outcome in patients with hematologic malignancies admitted to the intensive care unit. Hematol Oncol Stem Cell Ther 11(4):206–218
Wang T, Zhang L, Luo K, He J, Ma Y, Li Z et al (2016) Noninvasive versus invasive mechanical ventilation for immunocompromised patients with acute respiratory failure: a systematic review and meta-analysis. BMC Pulm Med 16(1):129
Liu J, Bell C, Campbell V, DeBacker J, Tamberg E, Lee C et al (2019) Noninvasive ventilation in patients with hematologic malignancy: a retrospective study. J Intensive Care Med 34(3):197–203
Amado-Rodríguez L, Bernal T, López-Alonso I, Blázquez-Prieto J, García-Prieto E, Albaiceta GM (2016) Impact of initial ventilatory strategy in hematological patients with acute respiratory failure: a systematic review and meta-analysis. Crit Care Med 44(7):1406–1413
Wise MP, Barnes RA, Baudouin SV, Howell D, Lyttelton M, Marks DI et al (2015) Guidelines on the management and admission to intensive care of critically ill adult patients with haematological malignancy in the UK. Br J Haematol 171(2):179–188
Huaringa AJ, Francis WH (2019) Outcome of invasive mechanical ventilation in cancer patients: Intubate or not to intubate a patient with cancer. J Crit Care 50:87–91
Hakim H, Flynn PM, Knapp KM, Srivastava DK, Gaur A (2009) Etiology and clinical course of febrile neutropenia in children with cancer. J Pediatr Hematol Oncol 31(9):623
Choudhari S, Gawande R, Watchmaker J, Bamnote P, Mishra P, Dwivedi P (2023) Bloodstream infections in cancer patients in central India: trend over five years. Access Microbiol 000673. https://doi.org/10.1099/acmi.0.000673.v1
Kumar K, Subash C, Prabhu D, Pulikkal D, Basker D (2021) Pattern of bacterial infections in Indian bone marrow transplant patients-experience from Chennai India. Blood 138:4855
Chauhan P, Gupta A, Gopinathan M, Sanjeev GA, Khanna S et al (2022) Real-world challenges in the management of acute myeloid leukemia: a single-center experience from North India. Ann Hematol 101(6):1261–73
Ghosh S, Chakraborty M, Samanta S, Sinha N, Saha S, Chattopadhyay A et al (2021) Analysis of blood stream infections, antibiograms and clinical outcomes in haematological patients with febrile neutropenia: data from a tertiary care haematology institute in India. Ann Hematol 100(2):395–403
Peter JV, Thomas K, Jeyaseelan L, Yadav B, Sudarsan TI, Christina J et al (2016) Cost of intensive care in India. Int J Technol Assess Health Care 32(4):241–245
Singh S, Lionel S, Jain H, Nayak L, Selvarajan S, Samuel P et al (2022) Real world data on unique challenges and outcomes of older patients with AML from resource limited settings: Indian acute leukemia research database (INwARD) of the hematology cancer consortium (HCC). Blood 140(Supplement 1):6096–6098
Acknowledgements
SS and VG designed the research study and protocols. SS, RS and GK performed the research and data entry. SS, JS and KJ performed literature search and statistical analysis. SS and PG analyzed and verified the data. SS, JS and PG wrote the paper and reviewed the final version. The authors thank Ms Namita Bansal for performing statistical analysis for this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Singh, S., Sharma, R., Singh, J. et al. Clinical Outcomes and Determinants of Survival in Patients with Hematologic Malignancies Admitted to Intensive Care Units with Critical Illness. Indian J Hematol Blood Transfus (2024). https://doi.org/10.1007/s12288-024-01757-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12288-024-01757-3