Abstract
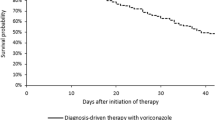
Current guidelines recommend computed tomography (cCT) scans of the chest in children with leukemia following 96 h of the onset of idiopathic neutropenia to eliminate pulmonary invasive fungal infections (IFIs). However, cCT exposes some children who are at a very high risk of developing secondary cancers to radiation. We aimed to determine the effect of antifungal prophylaxis (AFP) with voriconazole (VCZ) on the need for cCT scans in children with acute lymphoblastic leukemia (ALL) to eliminate pulmonary IFIs during chemotherapy. We retrospectively screened all patients’ data from their electronic charts. Children who were diagnosed as having ALL before February 2013 and did (AFP group) or did not (NoP group) receive AFP were divided into two groups and compared regarding cCT scans and relapse-mortality rates. Ninety-six children were diagnosed before February 2013 and did not receive primary AFP and 146 children were administered VCZ following a diagnosis of ALL. There were no significant demographic differences between the groups. A total of 128 cCTs had been required in 62 children in the NoP group, compared with 64 cCTs in 52 children in the AFP group. The percentage of the patients who had required at least one chest CT scan and the mean number of cCT scans in the NoP group were significantly higher compared with the AFP group. Proven-probable IFIs and relapse-mortality rates were higher in the NoP group compared with the AFP group. Mold-active AFP revealed a significant decrease in the need for cCT scans in children with ALL.


Similar content being viewed by others

Abbreviations
- ALL:
-
Acute lymphoblastic leukemia
- AFP:
-
Antifungal prophylaxis
- cCT:
-
Chest computed tomography
- IFI:
-
Invasive fungal infection
- NoP:
-
No prophylaxis
- PAP:
-
Primary antifungal prophylaxis
- VCZ:
-
Voriconazole
References
Siopi, M. Karakatsanis S, Roumpakis C, Korantanis K, Sambatakou H, Sipsas NV, Tsirigotis P, Pagoni M, Meletiadis J (2021) A Prospective multicenter cohort surveillance study of ınvasive aspergillosis in patients with hematologic malignancies in Greece: Impact of the Revised EORTC/MSGERC 2020 Criteria. J Fungi (Basel) 7(1). Epub 2021 Jan 5.
Ullmann AJ, Aguado JM, Arikan-Akdagli S, Denning DW, Groll AH, Lagrou K, Lass-Flörl C, Lewis RE, Munoz P, Verweij PE, Warris A, Ader F, Akova M, Arendrup MC, Barnes RA, Beigelman-Aubry C, Blot S, Bouza E, Brüggemann RJM, Buchheidt D, Cadranel J, Castagnola E, Chakrabarti A, Cuenca-Estrella M, Dimopoulos G, Fortun J, Gangneux JP, Garbino J, Heinz WJ, Herbrecht R, Heussel CP, Kibbler CC, Klimko N, Kullberg BJ, Lange C, Lehrnbecher T, Löffler J, Lortholary O, Maertens J, Marchetti O, Meis JF, Pagano L, Ribaud P, Richardson M, Roilides E, Ruhnke M, Sanguinetti M, Sheppard DC, Sinkó J, Skiada A, Vehreschild MJGT, Viscoli C, Cornely OA (2018) Diagnosis and management of Aspergillus diseases: executive summary of the 2017 ESCMID-ECMM-ERS guideline. Clin Microbiol Infect 24(Suppl 1):e1–e38 (Epub 2018 May 01)
Lass-Flörl C (2019) How to make a fast diagnosis in invasive aspergillosis. Med Mycol 57:S155–S160
Groll AH, Castagnola E, Cesaro S, Dalle JH, Engelhard D, Hope W, Roilides E, Styczynski J, Warris A, Lehrnbecher T (2014) Fourth European Conference on infections in Leukemia (ECIL-4): guidelines for diagnosis, prevention, and treatment of invasive fungal diseases in paediatric patients with cancer or allogeneic haematopoietic stem cell transplantation. Lancet Oncol 15:e327–e340.
Mellinghoff SC, Panse J, Alakel N, Behre G, Buchheidt D, Christopeit M, Hasenkamp J, Kehl M, Koldehoff M, Krause SW, Lehners N, Lilienfeld-Toall MV, Löhnert AY, Maschmeyer G, Teschner D, Ullmann AJ, Penack O, Ruhnke M, Mayer K, Ostermann H, Wolf HH, Cornely OA (2018) Primary prophylaxis of invasive fungal infections in patients with haematological malignancies: 2017 update of the recommendations of the Infectious Diseases Working Party (AGIHO) of the German Society for Haematology and Medical Oncology (DGHO). Ann Hematol 97:197–207
Lehrnbecher T, Fisher BT, Phillips B, Beauchemin M, Carlesse F, Castagnola E, Duong N, L Dupuis L, Fioravantti V, Groll AH, Haeusler GM, Roilides E, Science M, Steinbach WJ, Tissing W, Warris A, Patel P , Robinson PD, Sung Ll (2020) Clinical practice guideline for systemic antifungal prophylaxis in pediatric patients with cancer and hematopoietic stem-cell transplantation recipients. J Clin Oncol 38:3205–3216.
Tissot F, Agrawal S, Pagano L, Petrikkos G, Groll AH, Skiada A, LASS Fröll c, Calandra T, Viscoli C, Herbrecht R (2017) ECIL-6 guidelines for the treatment of invasive candidiasis, aspergillosis and mucormycosis in leukemia and hematopoietic stem cell transplant patients. Haematologica 102:433–444.
Warris A, Lehrnbecher T, Roilides E, Castagnola E, Brüggemann RJM, Groll AH (2019) ESCMID-ECMM guideline: diagnosis and management of invasive aspergillosis in neonates and children. Clin Microbiol Infect 25:1096–1113
Ferreras- Antolin L, Sharland M, Warris A (2019) Management of invasive fungal disease in neonates and children. Pediatr Infect Dis J 38:S2–S6
Lehrnbecher T, Robinson P, Fisher B, Alexander S, Ammann RA, Beauchemin M, Carlesse F, Groll AH, Haeusler GM, Santolaya M, Steinbach WJ, Castagnola E, Davis BL, Dupuis LL, Gaur AH, Tissing WJE, Zaoutis T, Phillips R, Sung L (2017) Guideline for the management of fever and neutropenia in children with cancer and hematopoietic stem cell transplantation recipients: 2017 update. J Clin Oncol 18:2082–2094
Krille L, Dreger S, Schindel R, Albrecht T, Asmussen M (2015) Risk of cancer incidence before the age of 15 years after exposure to ionizing radiation from computed tomography: results from a German cohort study. Radiation Environ Biophys 54:1–12
Miglioretti DL, Johnson E, Williams A, Greenlee RT, Weinmann S, Solberg LI, Feigelson HS, Roblin D, Flynn MJ, Vanneman N, Rebecca S-B (2013) Pediatric computed tomography and associated radiation exposure and estimated cancer risk. JAMA Pediatr 167:700–707
Mathews JD, Forsythe AV, Brady Z, Butler MW, Goergen SK, Byrnes GB, Giles GG, Wallace AB, Anderson PR, Guiver TA, McGale P, Cain TM, Dowty JG, Adrian Bickerstaffe C, Darby SC (2013) Cancer risk in 680 000 people exposed to computed tomography scans in childhood or adolescence: data linkage study of 11 million Australians. BMJ 346:f2360
Meulepas JM, Ronckers CM, Smets AMJB, Nievelstein RAJ, Lee C, Kieft M, Lameris JS, Herk MV, Greuter MJW, Jeukens CRLPN, Straten MV, Visser O, Leeuwen FEV, Hauptmann M (2014) Leukemia and brain tumors among children after radiation exposure from CT scans: design and methodological opportunities of the Dutch Pediatric CT Study. Eur J Epidemiol 29:293–301.
Rieger C, Herzog P, Eibel R, Fiegl M, Ostermann H (2008) Pulmonary MRI—a new approach for the evaluation of febrile neutropenic patients with malignancies. Support Care Cancer 16:599–606
Attenberger UI, Morelli JN, Henzler T, Buchheidt D, Fink C, Schoenberg SO, Reichert M (2014) 3 Tesla proton MRI for the diagnosis of pneumonia/lung infiltrates in neutropenic patients with acute myeloid leukemia: Initial results in comparison to HRCT. Eur J Radiol 83:e61–e66
Journy N, Ancelet S, Rehel JL, Mezzarobba M, Aubert B, Laurier D, Bernier MO (2014) Predicted cancer risks induced by computed tomography examinations during childhood, by a quantitative risk assessment approach. Radiat Environ Biophys 53:39–54
Pana ZD, Kourti M, Vikelouda A, Katzilakis N, Papageorgiou M, Doganis D, Petrikkos L, Paisiou A, Koliouskas D, Kattamis A, Stiakaki E, Chatzistilianou M, Vasilatou-Kosmidis H, Polychronopoulou S, Grafakos S, Roilides E (2018) Voriconazole antifungal prophylaxis in children with malignancies: a nationwide study. J Pediatr Hematol Oncol 40:22–26
Tragiannidis A, Dokos C, Lehrnbecher T, Groll AH (2012) Antifungal chemoprophylaxis in children and adolescents with haematological malignancies and following allogeneic haematopoietic stem cell transplantation: review of the literature and options for clinical practice. Drugs 72:685–704
Meryk A, Kropshofer G, Hutter J, Fritz J, Salvador C, Lass-Flörl C, Crazzolara R (2020) Benefits of risk-adapted and mould-specific antifungal prophylaxis in childhood leukemia. Br J Haematol 191:816–824
Fisher BT, Kavcic M, Li Y, Seif AE, Bagatell R, Huang YS, Zaoutis T, Torp K, Leckerman KH, Aplenc R (2014) Antifungal prophylaxis associated with decreased induction mortality rates and resources utilized in children with new onset acute myeloblastic leukemia. Clin Infect Dis 58(4):502–508. Epub 2013 Nov 23.
Kobayashi R, Hori D, Sano H, Suzuki D, Kishimoto K, Kobayashi K (2018) Risk factors for invasive fungal infection in children and adolescents with hematologic and malignant diseases: a 10-year analysis in a single institute in Japan. Pediatr Infect Dis J 37:1282–1285
Pauw BD, Walsh TJ, Donnelly JP, Stevens DA, Edwards JE, Calandra T, Pappas PG, Maertens J, Lortholary O, Kauffman CA, Denning DW, Patterson TF, Maschmeyer G, Bille J, Dismukes WE, Herbrecht R, Hope WW, Kibbler CC, Kullberg BJ, Marr KA, Muñoz P, Odds FC, Perfect JR, Restrepo A, Ruhnke M, Segal BH, Sobel JD, Sorrell TC, Viscoli C, Wingard JR, Zaoutis T, Bennett JE (2008) Revised definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group. Clin Infect Dis 46:1813–1821
Sahbudak Bal Z, Yilmaz Karapinar D, Karadas N, Sen S, Onder Sivis Z, Akinci AB, Balkan C, Kavakli K, Vardar F, Aydinok Y (2015) Proven and probable invasive fungal infections in children with acute lymphoblastic leukemia: results from an university hospital, 2005–2013. Mycoses 58:225–232
Sathya C, Alali AS, Wales PW, Langer JC, Kenney BD, Burd RS, Nance ML, Nathens AB (2019) Computed tomography rates and estimated radiation-associated cancer risk among injured children treated at different trauma center types. Injury Int J Care Injured 50:142–148
Berrington de G, Kim KP, Samet JM (2007) Radiation-induced cancer risk from annual computed tomography for patients with cystic fibrosis. Am J Respir Crit Care 179:970–973.
Boice JD (2015) Radiation epidemiology and recent paediatric computed tomography studies. Ann ICRP 44:236–248
Chodick G, Ronckers CM, Shalev V, Ron E (2007) Excess lifetime cancer mortality risk attributable to radiation exposure from computed tomography examinations in children. IMAJ 9:584–587
Mathews J.D., Forsythe A.V., Brady Z., Butler MV, Georgen SV et al (2013) Cancer risk in 680 000 people exposed to computed tomography scans in childhood or adolescence: data linkage study of 11 million Australians. BMJ, 346. https://doi.org/10.1136/bmj.f2360 ).
Kuhns LR, Oliver VJ Christodoulou E, Goodsitt MM (2011) The predicted increased cancer risk associated with a single computed tomography examination for calculus detection in pediatric patients compared with the natural cancer incidence. Pediatr Emerg Care 27(4):345–350. https://doi.org/10.1097/PEC.0b013e3182132016
Chodick G, Ronckers GM,Shalev V, Ron E (2007) Excess lifetime cancer mortality risk attritutable to radiation exposure from computed tomography examinations in children. IMAJ, pp 584–587.
Brenner DJ (2002) Estimating cancer risks from pediatric CT:going from the qualitative to the quantitative. Pediatr Radiol 32:228–231
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All of the authors declare they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Karadaş, N., Özdemir, H.H., Yilmaz, Y. et al. Primary Mold-Active Antifungal Prophylaxis Decreases the Need for Chest Computed Tomography Scans in Patients with Acute Lymphoblastic Leukemia. Indian J Hematol Blood Transfus 40, 196–203 (2024). https://doi.org/10.1007/s12288-023-01697-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12288-023-01697-4