Abstract
Minimal residual disease (MRD) has become an essential tool in the management of B-cell acute lymphoblastic leukemia (B-ALL) and aids in tailoring treatment strategies to suit specific patient needs. Although much progress has been made in this area, there is limited data on the use of MRD in the Indian context. Our objective was to identify relevant literature that discusses the utility of MRD in the management of B-cell ALL in adolescents and young adults (AYA) and adults in Indian settings. A systematic search and screening of articles were performed using the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines. The primary data source was PubMed followed by Google Scholar for articles and conference proceedings. Of the 254 records screened, 24 records were retained for analysis. MRD monitoring had a significant role in the management of AYA/adult B-cell ALL patients. Variability of results was observed across these studies with respect to methods, techniques, and use. However, these studies evidenced and validated the importance of MRD assessment in risk-adapted management of B-cell ALL and highlighted the need for optimization. The advances in MRD diagnostics and applications are yet to be tested and adopted in Indian settings. Hence, there is a need for in-depth research to develop and optimize approaches for calibrating country-specific management strategies. The potential role of MRD assessments in anticipating relapse or treatment failures warrants more attention for the preemptive positioning of novel strategies involving immunotherapies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute lymphoblastic leukemia (ALL) has a varied clinical presentation, with precursor B-cell ALL (B-ALL) being one of its most common immunological subtypes and affecting almost 75% of adult ALL cases. The most frequently observed genetic aberration in B-cell ALL is the Philadelphia chromosome-positive ALL (Ph + ve ALL) [1, 2]. The American Cancer Society estimates the occurrence of 6600 new cases of ALL in their population in the year 2022 [3], whereas the incidence rate of ALL in India has been estimated to be 101.4 per million and 62.3 per million, across all age groups and genders, respectively [2]. Minimal residual disease (MRD) has emerged as a robust prognostic indicator in B-cell ALL [4]. MRD can be described as the presence of a very low number of cancerous/malignant cells after chemotherapy or following a hematopoietic stem cell transplantation (HSCT) [5, 6].
MRD detection in ALL dates to the 1980s when immunofluorescence microscopy was used [7]. The use of MRD diagnostics in clinical trials as a surrogate endpoint for evaluating the efficacy of novel agents has also been observed. It was initially used for T-cell ALL because a highly specific immunophenotype for B-cell ALL had not been identified [8, 9]. The limitation of two- or three-color immunofluorescence microscopy made the detection of minor differences in marker expressions challenging, hence many new techniques emerged [8, 9]. Polymerase chain reaction (PCR), flow cytometry (FCM), next-generation sequencing (NGS), and next-generation flow cytometry are the molecular techniques used currently for MRD assessment [10, 11].
MRD assessments are very time-point specific [10]; hence, they are a critical prognostic indicator in very high-risk B-cell ALL patients. Among these patients, the subset that fails to achieve the end-of-induction (EOI) MRD positivity displays inferior outcomes [12, 13]. In addition, patients displaying very early MRD clearance have significantly better outcomes [14]. Studies have shown a direct strong correlation between MRD and the risk of relapse in ALL patients, thereby highlighting the prognostic value of MRD [10, 15]. Results from a meta-analysis reflect that pretransplant MRD positivity is a significant negative predictor of relapse-free survival (RFS), event-free survival (EFS), and overall survival (OS) [16]. Such results emphasize the importance of MRD evaluation before transplant, especially when treatment intensification is needed.
There is a paucity of data on MRD from an Indian context, and a complete understanding of MRD assessments and their correlation with outcomes among B-cell ALL patients is also lacking [17]. The primary objective of this review was to survey the available literature that discusses different aspects of MRD testing in the Indian context, specifically focusing on adolescent and young adults (AYA) and adult B-cell ALL patients. The insights gathered from studies specific to Indian settings are presented in this systematic literature review and discussed considering the global research landscape.
Methods
Literature Search
A systematic literature search was done using the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) reporting guidelines [18]. After the finalization of objectives, specific research questions were framed to guide the search process. Search queries were designed and reviewed independently for coverage and accuracy. The review of queries was based on the Peer Review for Electronic Search Strategies (PRESS) Guidelines. The components of the search string used in combinations are listed in Table 1.
Data Sources
The primary source of literature was PubMed. Additional searches were performed on Google Scholar, and the first 200 results were considered for preliminary screening [19]. From this subset, only articles not indexed in PubMed were included. Articles published within the last ten years from the date of query execution (April 3, 2022) were selected. Other data sources where the search was extended included original abstracts presented at the annual meetings of (1) the American Society of Hematology (ASH); (2) the American Society of Clinical Oncology (ASCO); (3) the European Society for Medical Oncology (ESMO); (4) the Indian Society of Hematology and Blood Transfusion (ISHBT); and the European Hematology Association (EHA) during the period 2019–2021.
Study Screening and Data Extraction
Based on objectives and research questions, the inclusion/exclusion criteria were outlined. The titles and abstracts of the articles retrieved were screened. Two independent reviewers performed the screening process, and disagreements were resolved by agreement based on discussion. Full-text versions of the articles that met the inclusion criteria were retrieved. These articles were selected for the next round of screening based on the full-text review. Articles that met the screening criteria were further considered for the extraction of study-relevant data. A predefined structured template was used for capturing data.
Screening Criteria
To minimize the risk of bias, all screening and evaluation steps were carried out independently by two individuals. Final decisions were made after resolving the disagreements based on discussion among reviewers. In addition, the inclusion/exclusion criteria were predefined based on which a template was designed to collect data. The risk of bias assessment of studies using standardized checklists (e.g., Newcastle–Ottawa scale) was not carried out as the primary goal was to survey the MRD-specific methodological aspects and application areas, and the number of articles retrieved was limited.
Results
Summary of Search
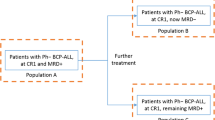
We identified and screened 205 studies from PubMed. An additional two articles were identified by searching Google Scholar for articles not indexed in PubMed. A total of 47 studies (range 2019–2021) were retrieved from annual meetings of ASH, ASCO, EHA, ESMO, and ISHBT. Of the total 254 studies, 24 articles were shortlisted according to the inclusion/exclusion criteria and after the removal of redundant articles by two independent reviewers. The detailed search strategy adopted during the systematic review is shown in Fig. 1. The list of final articles included after screening is given in Table 2.
MRD Assessment: Current Status
The Hematology Cancer Consortium maintains a database (Indian Acute Leukemia Research Database) that stores retrospective data from nine centers across India. Our search identified only one study exploring this database. The data published by Ganesan et al. [21] reflected that MRD assessment was available for only 47% of patients in the AYA group. Of the 1383 patients registered, 1141 (82.5%) underwent treatment, and MRD status was available for 654 patients. After induction, 76% of patients achieved complete remission (CR), and MRD was positive in 240 of 654 (37%) patients. Both univariate and multivariate analyses highlighted that inferior EFS and OS were associated with MRD positivity [21].
Timing of MRD Assessment
Regarding the timings for assessment, five studies followed EOI assessments on days 29–33 [22,23,24,25,26], except for studies by Chatterjee et al. [32] and Das et al. [33] that made assessments between days 35 and 40 and 30 and 35, respectively [27]. Individual studies (n = 2) that evaluated at mid-induction on day 21 or after phase 1a induction were also identified [27, 28]. Only three studies included end-of-consolidation (EOC) evaluations and subsequent follow-ups [24, 29, 32].
Samples and MRD Detection Methods
A majority of studies (n = 10) included in this systematic review used bone marrow aspirate, with a few (n = 3) using peripheral blood as well. Data comparing outcomes between these two samples were not available. Of the 24 studies, 22 studies used FCM using multicolored panels and multiparametric flow cytometry (MFC) for MRD assessments, whereas two used real-time quantitative PCR (RQ-PCR) [25, 29]. MFC methods with 5-color [30], 8-color [27, 42], 10-color [23, 24, 26, 28, 32, 33, 40], and 12-color [38] panels were observed in 12 studies. The panel of markers identified in these studies includes CD10, CD13, CD19, CD20, CD23, CD34, CD66c, CD123, CD200, and CD304 for the FCM analysis, and RQ-PCR was used for the BCR-ABL1 transcript characterization. A study by Chatterjee et al.[32] evaluated the expression pattern of CD304 in a cohort of adult B-cell ALL patients and reported that CD304 was found to be positive in a significant percentage of EOI (62/129 [48%]) and EOC (26/50 [52%]) MRD-positive, B-cell ALL samples. CD123 has also received consideration as a marker for residual disease assessment and response evaluation in acute myeloid leukemia and B-ALL. CD123 expression at diagnosis was shown to be associated with post-induction MRD-positive status in B-ALL (p < 0.001) [23, 33]. The Leukemia-associated aberrant immunophenotype (LAIP) and Difference from Normal (DFN) approach was found to be a reliable tool for MRD assessment at the diagnostic and MRD time points in the study by Das et al. [33]. Changes in at least one of the nine immunophenotypic markers in B-ALL post-induction was observed in 94.04% cases. The utility of other markers such as CD44, CD73, CD304, and CD200 was assessed in those cases requiring review of baseline IPT. Out of 18 cases, the information was useful in 8 cases (44.4%). The study emphasized the need for better markers for distinguishing leukemic blasts from hematogones. Additionally, MRD assessment in B-ALL is complicated by changes in IPT after induction chemotherapy, necessitating pattern recognition and simultaneous analysis of multiple IPT markers. [33]. Arunachalam et al. [29] analyzed the prognostic relevance of MRD based on BCR-ABL1 copy numbers in Ph-positive ALL patients. BCR-ABL1 copy numbers were evaluated using RQ-PCR. The cost-effectiveness of the MRD method was analyzed in three studies [25, 31, 38]. Patkar et al. [31] proposed a relatively cost-effective MRD panel applicable to over 90% of patients. Using their approach, they detected MRD in 60% and 47% of patients at mid- and end-induction time points, respectively. Another two studies focused on the optimization of MRD panels with the goal of cost-effectiveness and reduction in the number of LAIPs [22, 37].
MRD and Treatment Outcomes
Only five articles focused on evaluating specific treatment regimens with MRD as a measure of post-induction response [24, 27, 28, 35, 36]. The outcomes of patients treated with different regimens were presented as combined results in most studies. Only one study was identified, where post-induction MRD was used as one of the indications for stem cell transplantation (SCT) in the first complete remission (CR1) [34]. A phase 2 study evaluating the combination of bortezomib, rituximab, and a pediatric-inspired ALL regimen showed post-induction persistent MRD to be associated with inferior OS and EFS [24]. Outcomes among MRD-based, risk-stratified patients show that patients with poor-risk status were associated with inferior OS and EFS [29]. The impact of MRD on OS was studied in pediatric and AYA groups treated with a modified multicenter protocol (MCP) 841 [27]. The results outline that MRD-negative patients responded better than MRD-positive patients (p = 0.03). Post-induction MRD was acknowledged as a useful prognostic tool for ALL patients treated with the modified MCP 841 protocol. Furthermore, in a study assessing the outcomes associated with Berlin–Frankfurt–Münster-90 among AYA, post-induction MRD persistence emerged as the only factor predictive of poor outcomes [28].
Risk Category and MRD Status
A study conducted by Arunachalam et al. [29] assessed the prognostic relevance of MRD based on BCR-ABL1 copy numbers in Ph-positive ALL patients. In this study, the MRD status was assessed at three different time points. Patients having persistent MRD-positive status at all three measured time points or having an increasing BCR-ABL1/ABL1 copy number ratio with an increase in their MRD-positive status by the third measurement were categorized as MRD poor-risk status. Those patients having MRD negativity and decreasing BCR-ABL1/ABL1 copy number ratio with a strong MRD-negative status by the third assessment were categorized as MRD good risk. MRD poor-risk patients had adverse outcomes when compared to MRD good-risk patients in terms of OS (p = 0.031) and EFS (p ≤ 0.001). Patients with high-risk diseases and those with EOI MRD positivity are at higher risk of adverse events [22]. CD304 positivity has also been shown to be associated with BCR-ABL1 fusion, with a significant percentage of EOI and EOC MRD positivity [32]. Results from a smaller cohort indicate that patients with P2Y receptor family member 8-cytokine receptor-like factor 2 (P2RY8-CRLF2) translocation who underwent EOI MRD testing showed positivity [26].
Discussion
The primary objective of this study was to survey the available literature that discusses different aspects of MRD testing in the Indian context, specifically focusing on AYA and adult B-cell ALL patients, as B-cell ALL studies done so far have been limited to the pediatric population and have been done on smaller cohorts. A systematic search was carried out, which indicated limited data on the use and impact of MRD assessment among AYA and adult B-cell ALL patients in Indian settings. Available data on samples, timings, techniques, and outcomes were gathered. This review presents and discusses the limitations and aspects that need further investigation. The MRD assessment status was available only from one study [21].
The aspects of sensitivity of MRD assessment and its implications have not been discussed in the identified studies. Samples, sensitivity, and timings can be critical factors in leveraging maximum benefits from MRD assessment. An important point to consider is the timing of MRD measurement, which can help in taking treatment decisions. Different insights can be provided by MRD, depending upon the timing of assessment: very early, after induction/consolidation, and before and after SCT. Although early response assessment (days 8 and 15) has been discussed in the literature, the review of articles selected for this study did not reveal any discussion on such aspects. Evidence supports early MRD testing [1]. Negative MRD status at very early time points during the induction phase correlates with better outcomes both in adult and in childhood B-ALL [43, 44]. Our results also suggest that MRD was a critical prognostic indicator strongly associated with RFS and EFS [29]. The focus of most studies identified in the review was on assessment at EOI and/or EOC. The importance of EOI MRD assessment was highlighted in one study [42]. Different treatment protocols have established informative checkpoints, which aid in monitoring outcomes appropriately. However, such sequential monitoring was not observed in most studies identified in Indian settings.
The majority of studies identified from Indian settings have used bone marrow samples, with some studies using peripheral blood. However, no comparison of utility has been studied. Several clinical studies have evaluated MRD status in bone marrow samples and blood in B-cell ALL and T-cell ALL [33, 45,46,47]. The use of peripheral blood MRD can serve as a noninvasive technique to monitor systemic relapse and might have additional clinical and diagnostic value in patients with a high risk of extramedullary disease [48]. There is a paucity of data on studies evaluating the application of MRD assessment. Typically, MRD assessments are done using a single aspirate sample, which can vary due to sampling error and/or collection techniques [49]. Inaccuracies resulting from a sample that is diluted or has an unequal distribution of disease involvement in the bone marrow can pose limitations.
The use of > 10−4 or > 5 × 10−4 as a threshold has been suggested for poor MRD responders with poor prognoses [4]. The acceptable level of sensitivity of MRD assays remains unresolved [1]. MFC and quantitative PCR are the most frequently used MRD detection techniques/methods in clinical practice. MRD-based risk stratification can be further refined by using NGS like sensitive assays. Accurate identification of patients with persistent MRD who are at the highest risk of relapse will allow the design of reasonable post-remission therapies using novel agents [50]. Our results suggested that CD304 was a stable MRD marker that could be useful in detecting MFC-based MRD monitoring, especially in high-sensitivity MRD assay [32]. Even though LAIP and DFN approach combination is one of the best for MRD assessment, its utility could be affected by the immunophenotypic patterns of leukemia blasts mimicking hematogones and in CD10 dim to negative cases. Hence, every case with a hematogone pattern and dim to negative CD10 expression at diagnosis is recommended to have a statement in the diagnostic flow cytometry report so that the hemato-pathologist viewing the report is aware of this. More immunophenotypic markers should be evaluated which can help in differentiating between hematogones and leukemia blasts, thereby improving the reliability of the MFC-based MRD assays. Changes in immunophenotypic markers in B-ALL post- induction are frequent and may be useful but such changes could possibly compromise the MRD assessment in certain cases [33].
MRD assessment for monitoring treatment outcomes was one of the objectives defined for this review. The Programa Español de Tratamientos en Hematología (PETHEMA) ALL-AR03 trial used MRD to guide treatment decisions at the EOC and found that HSCT could be avoided in patients who reached MRD negativity without adversely affecting their prognosis [51]. MRD can play a role in sparing patients from risks associated with transplantation without negatively affecting survival outcomes [52]. Patients who are at a high risk of leukemia relapse after allogeneic SCT can be identified by the kinetics of MRD clearance. Patients who have not been able to achieve early molecular remission after transplantation might require prompt and appropriate preventive treatments [53]. The role of MRD in the management of Ph-positive B-cell ALL has also been established and can be important in in-patient stratification [14]. The percentage of MRD reduction corresponds with superior disease-free survival (DFS), irrespective of the tyrosine kinase inhibitor (TKI) used [54]. MRD persistence and/or reappearance can be indicative of resistant mutations (e.g., T315I). Such cases may warrant alternative approaches, including novel TKIs and/or combinations of TKI with immunotherapy [55]. The early achievement of MRD negativity in the treatment of adults with Ph-negative B-cell ALL is a strong predictor of survival [56]. Ph-negative patients in this study were classified as B-cell ALL patients who had achieved MRD-negative status at the end of induction at two different time points and were also observed to be early MRD responders. MRD also has the potential to guide the selection of patients for treatment de-intensification. However, the appropriate way to utilize MRD results for treatment de-intensification is yet to be defined.
The value of having achieved MRD negativity is significant in pediatric and adult ALL patients [15]. In adult B-ALL patients, achieving MRD negativity is consistently associated with better survival outcomes than those of patients with MRD-positive status [1]. Such results have been consistent across methods, therapies, times of MRD assessment, cutoff levels, and disease subtypes [1]. Relatively few reports are available on the significance of MRD in patients with relapsed disease. Such status was also evident from the search carried out for this study. In adults with ALL, the prognostic significance of MRD in relapsed/refractory ALL has been primarily reported in individual studies using novel salvage treatments [57]. In a study of inotuzumab as salvage therapy, achieving MRD negativity was associated with a longer remission duration [58]. A retrospective analysis of 78 patients showed a differential impact of MRD negativity according to salvage (S) status in patients with relapsed/refractory B-ALL [57]. Patients with relapsed/refractory ALL who achieved MRD negativity in S1 had long-term survival, whereas patients in S2 generally had poor outcomes regardless of MRD status. Patients in S1 who achieved MRD negativity and subsequently underwent SCT had the best outcomes, with a 2-year OS rate of 65%. Assessment of the prognostic value of MRD negativity at the end of inotuzumab treatment shows that patients in first salvage who achieved MRD negativity experienced significantly improved survival vs. that seen in MRD-positive patients. This observation was significant, particularly among those patients who proceeded to SCT. Among patients with relapsed/refractory ALL treated with inotuzumab, the MRD-negative complete remission/complete remission with incomplete count recovery (CR/CRi) group had the best survival outcomes [59]. The benefit of achieving MRD negativity highlights its relevance for assessing prognosis and measuring treatment efficacy.
Although studies identified in the search reveal minimal data on applications of MRD, there is a broader research landscape with extended scope of utility. MRD response has been considered in drug development as an early marker of efficacy in clinical studies. It has potential use as a surrogate endpoint in the registration of studies for accelerated drug approval [60, 61]. MRD status warrants consideration as an early measure of disease response for evaluating new therapies, improving the efficiency of clinical trials, accelerating drug development, and regulatory approval [15]. However, approval of such findings based on an intermediate endpoint would require confirmation using traditional efficacy endpoints.
Conclusion
The systematic search carried out as a part of this study revealed limited data on applications of MRD in the management of B-cell ALL among AYA and adult populations. The existing data suggest its applicability in facilitating improved treatment outcomes. The comparison of results from included studies with the scope of published evidence from literature databases highlights the need for more research specific to Indian settings. Aspects related to cost, resource limitations, and differences in biology have been pointed out. These may be important considerations in designing future research investigations. Current evidence suggests that MRD is an essential tool to facilitate the optimal course of management of B-cell ALL by assisting in critical clinical decisions. Such assessments can effectuate the distinctness of situations where the use of conventional options has higher chances of treatment failure and identify patients who can benefit the most from novel agents.
References
Bassan R, Brüggemann M, Radcliffe H-S et al (2019) A systematic literature review and meta-analysis of minimal residual disease as a prognostic indicator in adult B-cell acute lymphoblastic leukemia. Haematologica 104:2028–2039. https://doi.org/10.3324/haematol.2018.201053
Agrwal S, Sahi PK (2020) National comprehensive cancer network guidelines for pediatric acute lymphoblastic leukemia. Indian Pediatr 57:561–564. https://doi.org/10.1007/s13312-020-1855-1
Key Statistics for Acute Lymphocytic Leukemia (ALL). https://www.cancer.org/cancer/acute-lymphocytic-leukemia/about/key-statistics.html. Accessed 14 Sept 2022
Van Dongen JJM, Van der Velden VHJ, Brüggemann M et al (2015) Minimal residual disease diagnostics in acute lymphoblastic leukemia: Need for sensitive, fast, and standardized technologies. Blood 125:3996–4009. https://doi.org/10.1182/blood-2015-03-580027
Porwit A, Béné M-C (2011) CHAPTER 19: acute lymphoblastic leukemia/lymphoma and mixed phenotype acute leukemias. In: Porwit A, McCullough J, Erber WN (eds) Blood and bone marrow pathology. Second Edition, pp 289–01
Overbergh L, Vig S, Coun F, et al. (2017) Chapter 4: quantitative polymerase chain reaction. In: Patrinos GP (ed) Molecular diagnostics. Third Edition, pp 41–58
Bradstock KF, Janossy G, Tidman N et al (1981) Immunological monitoring of residual disease in treated thymic acute lymphoblastic leukaemia. Leuk Res 5:301–309. https://doi.org/10.1016/0145-2126(81)90002-3
Greaves M, Delia D, Janossy G et al (1980) Acute lymphoblastic leukaemia associated antigen: IV: expression on non-leukaemic “lymphoid” cells. Leuk Res 4:15–32. https://doi.org/10.1016/0145-2126(80)90044-2
van Wering ER, van der Linden-Schrever BE, Szczepański T et al (2000) Regenerating normal B-cell precursors during and after treatment of acute lymphoblastic leukaemia: implications for monitoring of minimal residual disease. Br J Haematol 110:139–146. https://doi.org/10.1046/j.1365-2141.2000.02143.x
Patil PP, Jafa E, Aggarwal M (2021) Minimal residual disease in acute lymphoblastic leukemia. Indian J Med Paediatr Oncol 42:71–76. https://doi.org/10.1055/s-0041-1729730
Della Starza I, Chiaretti S, De Propris MS et al (2019) Minimal residual disease in acute lymphoblastic leukemia: technical and clinical advances. Front Oncol 9:726. https://doi.org/10.3389/fonc.2019.00726
Salzer WL, Burke MJ, Devidas M et al (2021) Minimal residual disease at end of induction and consolidation remain important prognostic indicators for newly diagnosed children and young adults with very high-risk (VHR) B-lymphoblastic leukemia (B-ALL): Children’s Oncology Group AALL1131. JCO 39:10004–10104. https://doi.org/10.1200/JCO.2021.39.15_suppl.10004
Mortuza FY, Papaioannou M, Moreira IM et al (2002) Minimal residual disease tests provide an independent predictor of clinical outcome in adult acute lymphoblastic leukemia. J Clin Oncol 20:1094–1104. https://doi.org/10.1200/JCO.2002.20.4.1094
Lee S, Kim D-W, Cho B-S et al (2012) Impact of minimal residual disease kinetics during imatinib-based treatment on transplantation outcome in Philadelphia chromosome-positive acute lymphoblastic leukemia. Leukemia 26:2367–2374. https://doi.org/10.1038/leu.2012.164
Berry DA, Zhou S, Higley H et al (2017) Association of minimal residual disease with clinical outcome in pediatric and adult acute lymphoblastic leukemia: a meta-analysis. JAMA Oncol 3:e170580. https://doi.org/10.1001/jamaoncol.2017.0580
Shen Z, Gu X, Mao W et al (2018) Influence of pre-transplant minimal residual disease on prognosis after Allo-SCT for patients with acute lymphoblastic leukemia: systematic review and meta-analysis. BMC Cancer 18:755. https://doi.org/10.1186/s12885-018-4670-5
Panda SS, Radhakrishnan V, Ganesan P et al (2020) Flow cytometry based MRD and its impact on survival outcome in children and young adults with ALL: a Prospective Study from a Tertiary Cancer Centre in Southern India. Indian J Hematol Blood Transfus 36:300–308. https://doi.org/10.1007/s12288-019-01228-0
Page MJ, McKenzie JE, Bossuyt PM, The PRISMA et al (2020) statement: an updated guideline for reporting systematic reviews. BMJ. https://doi.org/10.1136/bmj.n71
Haddaway NR, Collins AM, Coughlin D, Kirk S (2015) The role of google scholar in evidence reviews and its applicability to grey literature searching. PLoS ONE 10:e0138237. https://doi.org/10.1371/journal.pone.0138237
Bommannan BKK, Arumugam JR, Sundersingh S et al (2019) CD19 negative and dim precursor B-lineage acute lymphoblastic leukemias: real-world challenges in a targeted-immunotherapy era. Leuk Lymphoma 60:3154–3160. https://doi.org/10.1080/10428194.2019.1625043
Ganesan P, Jain H, Bagal B et al (2021) Outcomes in adolescent and young adult acute lymphoblastic leukaemia: a report from the Indian Acute Leukaemia Research Database (INwARD) of the Hematology Cancer Consortium (HCC). Br J Haematol 2021:193. https://doi.org/10.1111/bjh.17268
Bommannan K, Arumugam JR, Radhakrishnan V et al (2022) Precursor B-lineage acute lymphoblastic leukemia patients with aberrant natural killer cell and T cell - lineage antigen expression: experience from a tertiary cancer care center. Hematol Transfus Cell Ther 44:143–150. https://doi.org/10.1016/j.htct.2020.08.012
Das N, Gupta R, Gupta SK et al (2020) A real-world perspective of CD123 expression in acute leukemia as promising biomarker to predict treatment outcome in B-ALL and AML. Clin Lymphoma Myeloma Leuk 20:e673–e684. https://doi.org/10.1016/j.clml.2020.05.004
Jain H, Sengar M, Goli VB et al (2021) Bortezomib and rituximab in de novo adolescent/adult CD20-positive, Ph-negative pre-B-cell acute lymphoblastic leukemia. Blood Adv 5:3436–3444. https://doi.org/10.1182/bloodadvances.2020003368
Jain P, Korula A, Deshpande P et al (2018) Adult acute lymphoblastic leukemia: limitations of intensification of therapy in a developing country. J Glob Oncol 4:1–12. https://doi.org/10.1200/JGO.17.00014
Virk H, Rana S, Sharma P et al (2021) Hematological characteristics, cytogenetic features, and post-induction measurable residual disease in thymic stromal lymphopoietin receptor (TSLPR) overexpressed B-cell acute lymphoblastic leukemia in an Indian cohort. Ann Hematol 100:2031–2041. https://doi.org/10.1007/s00277-021-04574-0
Pandey A, Ahlawat S, Singh A et al (2020) Outcomes and impact of minimal residual disease (MRD) in pediatric, adolescent and young adults (AYA) with acute lymphoblastic leukemia treated with modified MCP 841 protocol. Cancer Res Stat Treat 3:183. https://doi.org/10.4103/CRST.CRST_85_20
Rajendra A, Jain H, Bonda VNA et al (2021) Outcomes and prognostic factors in adolescents and young adults with ALL treated with a modified BFM-90 protocol. Blood Adv 5:1178–1193. https://doi.org/10.1182/bloodadvances.2020003526
Arunachalam AK, Janet NB, Korula A et al (2020) Prognostic value of MRD monitoring based on BCR-ABL1 copy numbers in Philadelphia chromosome positive acute lymphoblastic leukemia. Leuk Lymphoma 61:3468–3475. https://doi.org/10.1080/10428194.2020.1811272
Garg N, Gupta R, Kotru M (2021) CD34 is not expressed by blasts in a Tthird of B-ALL patients and its negativity is associated with aberrant marker expression: a retrospective analysis. Asian Pac J Cancer Prev 22:919–925. https://doi.org/10.31557/APJCP.2021.22.3.919
Patkar N, Alex AAB et al (2012) Standardizing minimal residual disease by flow cytometry for precursor B lineage acute lymphoblastic leukemia in a developing country. Cytometry B Clin Cytom 82:252–258. https://doi.org/10.1002/cyto.b.21017
Chatterjee G, Dudakia V, Ghogale S et al (2021) Expression of CD304/neuropilin-1 in adult b-cell lymphoblastic leukemia/lymphoma and its utility for the measurable residual disease assessment. Int J Lab Hematol 43:990–999. https://doi.org/10.1111/ijlh.13456
Das N, Gupta R, Gupta SK et al (2021) Critical evaluation of the utility of pre- and post-therapy immunophenotypes in assessment of measurable residual disease in B-ALL. Ann Hematol 100(10):2487–2500. https://doi.org/10.1007/s00277-021-04580-2
Aboobacker F, Korula A, Devasia A, et al (2019) Allogeneic stem cell transplantation for acute lymphoblastic leukemia: A single centre experience. In: 60th annual conference of indian society of hematology & blood transfusion (ISHBT) October 2019. Indian J Hematol Blood Transfus, vol 35, pp 1–51. https://doi.org/10.1007/s12288-019-01207-5
Lakshmy CV, George B, Korula A, et al (2021) Utility of a low intensity bortezomib based regimen to induce remission in patients with relapsed acute lymphoblastic leukemia. In: 62nd annual conference of indian society of hematology & blood transfusion (ISHBT). Indian J Hematol Blood Transfus, vol 37, pp 1–172. https://doi.org/10.1007/s12288-021-01510-0.
Özcan M, Cassaday RD, Singh P et al (2021) The efficacy and safety of low-dose inotuzumab ozogamicin in patients with relapsed or refractory acute lymphoblastic leukemia: Interim results of a phase 4 study. Blood 138:1208–1308. https://doi.org/10.1182/blood-2021-15000
Bhandary C, Prabhu M, Kar R, Basu D (2020) Expression of leukemia associated immunophenotype markers at diagnosis by 10 color flow cytometry in B cell precursor acute lymphoblastic leukemia for optimization of minimal residual disease panel. In: 61st Annual Conference of Indian Society of Hematology & Blood Transfusion (ISHBT) November 2020. Indian J Hematol Blood Transfus, vol 36, pp 1–229. https://doi.org/10.1007/s12288-020-01384-8
Meganathan D, Aakif M, Priyanka M, et al (2021) Advantages of 12 colour panel for acute leukemia diagnosis: data from a single centre in adolescent and adult population. In: 62nd annual conference of indian society of hematology & blood transfusion (ISHBT). Indian J Hematol Blood Transfus, vol 37, pp 1–172. https://doi.org/10.1007/s12288-021-01510-0
Vatsala BK, Sridevi BH, Nirupama M, et al (2020) Diagnostic role of flow cytometry in immunophenotyping of adult acute lymphoblastic leukemia. In: 61st annual conference of indian society of hematology & blood transfusion (ISHBT) November 2020. Indian J Hematol Blood Transfus, vol 36, pp 1–229. https://doi.org/10.1007/s12288-020-01384-8
Mazumder S, Manivannan P, Kar R, et al (2021) Optimization of a ten-colour antibody panel for measurable residual disease detection in B cell precursor acute lymphoblastic leukemia based on leukemia associated immunophenotype at diagnosis. In: 62nd annual conference of indian society of hematology & blood transfusion (ISHBT). Indian J Hematol Blood Transfus, vol 37, pp 1–172. https://doi.org/10.1007/s12288-021-01510-0
Dhar L, Singh S, Tanwar P, et al (2021) Significance of expression of CD38, CD58, CD49D AND CD66C in acute lymphoblastic leukemia. In: 62nd annual conference of indian society of hematology & blood transfusion (ISHBT). Indian J Hematol Blood Transfus, vol 37, pp 1–172. https://doi.org/10.1007/s12288-021-01510-0
Arunachalam AK, Kathirvel K, Kamruddin F, et al (2019) Clinical significance of end induction MRD monitoring in B Cell ALL: A single centre experience. In: 60th annual conference of indian society of hematology & blood transfusion (ISHBT) October 2019. Indian J Hematol Blood Transfus, vol 35, pp 1–151. https://doi.org/10.1007/s12288-019-01207-5
Brüggemann M, Gökbuget N, Kneba M (2012) Acute lymphoblastic leukemia: monitoring minimal residual disease as a therapeutic principle. Semin Oncol 39:47–57. https://doi.org/10.1053/j.seminoncol.2011.11.009
Gökbuget N, Dombret H, Giebel S et al (2019) Minimal residual disease level predicts outcome in adults with Ph-negative B-precursor acute lymphoblastic leukemia. Hematology 24:337–348. https://doi.org/10.1080/16078454.2019.1567654
Brisco MJ, Sykes PJ, Hughes E et al (1997) Monitoring minimal residual disease in peripheral blood in B-lineage acute lymphoblastic leukaemia. Br J Haematol 99:314–319. https://doi.org/10.1046/j.1365-2141.1997.3723186.x
van der Velden VHJ, Cazzaniga G, Schrauder A et al (2007) Analysis of minimal residual disease by Ig/TCR gene rearrangements: guidelines for interpretation of real-time quantitative PCR data. Leukemia 21:604–611. https://doi.org/10.1038/sj.leu.2404586
Coustan-Smith E, Sancho J, Hancock ML et al (2002) Use of peripheral blood instead of bone marrow to monitor residual disease in children with acute lymphoblastic leukemia. Blood 100:2399–2402. https://doi.org/10.1182/blood-2002-04-1130
Keegan A, Charest K, Schmidt R et al (2018) Flow cytometric minimal residual disease assessment of peripheral blood in acute lymphoblastic leukaemia patients has potential for early detection of relapsed extramedullary disease. J Clin Pathol 71:653–658. https://doi.org/10.1136/jclinpath-2017-204828
Shalabi H, Yuan CM, Kulshreshtha A et al (2020) Disease detection methodologies in relapsed B-cell acute lymphoblastic leukemia: opportunities for improvement. Pediatr Blood Cancer. https://doi.org/10.1002/pbc.28149
Short NJ, Jabbour E (2017) Minimal residual disease in acute lymphoblastic leukemia: How to recognize and treat it. Curr Oncol Rep 19:6. https://doi.org/10.1007/s11912-017-0565-x
Ribera J-M, Oriol A, Morgades M et al (2014) Treatment of high-risk Philadelphia chromosome–negative acute lymphoblastic leukemia in adolescents and adults according to early cytologic response and minimal residual disease after consolidation assessed by flow cytometry: final results of the PETHEMA ALL-AR-03 trial. JCO 32:1595–1604. https://doi.org/10.1200/JCO.2013.52.2425
Hoelzer D, Bassan R, Dombret H et al (2016) Acute lymphoblastic leukaemia in adult patients: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 27:v69–v82. https://doi.org/10.1093/annonc/mdw025
Spinelli O, Peruta B, Tosi M et al (2007) Clearance of minimal residual disease after allogeneic stem cell transplantation and the prediction of the clinical outcome of adult patients with high-risk acute lymphoblastic leukemia. Haematologica 92:612–618. https://doi.org/10.3324/haematol.10965
Chiaretti S, Vitale A, Vignetti M et al (2016) A sequential approach with imatinib, chemotherapy and transplant for adult Ph+ acute lymphoblastic leukemia: final results of the GIMEMA LAL 0904 study. Haematologica 101:1544–1552. https://doi.org/10.3324/haematol.2016.144535
Martinelli G, Boissel N, Chevallier P et al (2017) Complete hematologic and molecular response in adult patients with relapsed/refractory Philadelphia chromosome-positive B-precursor acute lymphoblastic leukemia following treatment with blinatumomab: results from a Phase II, single-arm, multicenter study. J Clin Oncol 35:1795–1802. https://doi.org/10.1200/JCO.2016.69.3531
Yilmaz M, Kantarjian H, Wang X et al (2019) The early achievement of measurable residual disease negativity in the treatment of adults with Philadelphia-negative B-cell acute lymphoblastic leukemia is a strong predictor for survival. Clin Lymphoma Myeloma Leuk 19:S193–S194. https://doi.org/10.1016/j.clml.2019.07.040
Jabbour E, Short NJ, Jorgensen JL et al (2017) Differential impact of minimal residual disease negativity according to the salvage status in patients with relapsed/refractory B-cell acute lymphoblastic leukemia: MRD in Relapsed/Refractory ALL. Cancer 123:294–302. https://doi.org/10.1002/cncr.30264
Kantarjian H, Thomas D, Jorgensen J et al (2013) Results of inotuzumab ozogamicin, a CD22 monoclonal antibody, in refractory and relapsed acute lymphocytic leukemia: results of Inotuzumab in ALL. Cancer 119:2728–2736. https://doi.org/10.1002/cncr.28136
Jabbour E, Gökbuget N, Advani A et al (2020) Impact of minimal residual disease status in patients with relapsed/refractory acute lymphoblastic leukemia treated with inotuzumab ozogamicin in the phase III INO-VATE trial. Leukemia Res 88:106283. https://doi.org/10.1016/j.leukres.2019.106283
MRD in MM guidelines. In: European Medicine Agency. https://www.ema.europa.eu/documents/scientific-guideline/draft-guideline-use-minimal-residual-disease-clinical-endpoint-multiple-myeloma-studies_en.pdf. Accessed 21 Sep 2022
Research C for DE and (2022) Guidances (Drugs). In: FDA. https://www.fda.gov/drugs/guidance-compliance-regulatory-information/guidances-drugs. Accessed 21 Sep 2022
Acknowledgements
We thank BioQuest Solutions for providing editorial assistance.
Funding
The study was funded by Pfizer, India for manuscript development and editorial assistance.
Author information
Authors and Affiliations
Contributions
All authors have contributed equally to the study conception, design, drafting, review, and finalization of the manuscript.
Corresponding author
Ethics declarations
Conflict of interests
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Menon, H., Singh, P.K., Bagal, B. et al. Minimal Residual Disease in the Management of B-Cell Acute Lymphoblastic Leukemia: A Systematic Review of Studies from Indian Settings. Indian J Hematol Blood Transfus 40, 1–11 (2024). https://doi.org/10.1007/s12288-023-01641-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12288-023-01641-6