Abstract
Background
Although arm lymphedema is a well-known complication following breast cancer surgery, previous studies involving a small population showed inconsistent results regarding the risk. Therefore, we examined the risk factors using a Japanese nationwide database.
Methods
Female patients who underwent breast cancer surgery from April, 2016, to March, 2020, were identified from a Japanese nationwide database. Multivariable survival analyses for 19 baseline factors (12 patient characteristics, four tumor characteristics, and three surgical procedures) were conducted to investigate risk factors associated with treatments for postoperative lymphedema (such as lymphatic bypass, compositive drainage therapy, hospitalization, and Kampo use) with a multilevel model to adjust for within-hospital clustering. We also conducted multivariable analysis for five postoperative factors (two local complications and three postoperative therapies) with adjustment for 19 baseline factors.
Results
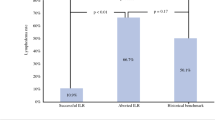
The study included 84,022 patients; 1547 (1.8%) received treatments for lymphedema during a median follow-up of 119 weeks (interquartile range, 59–187 weeks). Young age, obesity, smoking, collagen diseases, advanced cancer stage, total mastectomy, axillary dissection, postoperative bleeding, chemotherapy, and radiotherapy were identified as risk factors. Postoperative chemotherapy (hazard ratio, 3.78 [95% confidence interval, 3.35–4.26]) and axillary dissection (2.46 [1.95–3.11]) showed the highest odds ratio among the risk factors. The cumulative probabilities in high-risk patients reached approximately 3% at 1 year and 6% at 4 years after surgery.
Conclusions
This study identified several risk factors for postoperative lymphedema in breast cancer surgery. The treatment initiation increased markedly within the first year and gradually after 1 year post-surgery.

Similar content being viewed by others
References
Rockson SG. Lymphedema after breast cancer treatment. N Engl J Med. 2018;379:1937–44. https://doi.org/10.1056/NEJMcp1803290.
Disipio T, Rye S, Newman B, Hayes S. Incidence of unilateral arm lymphoedema after breast cancer: a systematic review and meta-analysis. Lancet Oncol. 2013;14:500–15. https://doi.org/10.1016/S1470-2045(13)70076-7.
Abouelazayem M, Elkorety M, Monib S. Breast lymphedema after conservative breast surgery: an up-to-date systematic review. Clin Breast Cancer. 2021;21:156–61. https://doi.org/10.1016/j.clbc.2020.11.017.
Committee E. The diagnosis and treatment of peripheral lymphedema: 2016 consensus document of the international society of lymphology. Lymphology. 2016;49:170–84.
Casley-Smith JR. Alterations of untreated lymphedema and it’s grades over time. Lymphology. 1995;28:174–85.
Harris SR, Hugi MR, Olivotto IA, Levine M, Steering Committee for Clinical Practice Guidelines for the Care and Treatment of Breast Cancer. Clinical practice guidelines for the care and treatment of breast cancer: 11. Lymphedema CMAJ. 2001;164:191–9.
Shaitelman SF, Cromwell KD, Rasmussen JC, Stout NL, Armer JM, Lasinski BB, et al. Recent progress in the treatment and prevention of cancer-related lymphedema. CA Cancer J Clin. 2015;65:55–81. https://doi.org/10.3322/caac.21253.
Mclaughlin SA, Desnyder SM, Klimberg S, Alatriste M, Boccardo F, Smith ML, et al. Considerations for clinicians in the diagnosis, prevention, and treatment of breast cancer-related lymphedema, recommendations from an expert panel: part 2: Preventive and therapeutic options. Ann Surg Oncol. 2017;24:2827–35. https://doi.org/10.1245/s10434-017-5964-6.
Nagai A, Shibamoto Y, Ogawa K. Therapeutic effects of saireito (Chai-Ling-Tang), a traditional Japanese herbal medicine, on lymphedema caused by radiotherapy: a case series study. Evid Based Complement Alternat Med. 2013;2013: 241629. https://doi.org/10.1155/2013/241629.
Yoshikawa N, Kajiyama H, Otsuka N, Tamauchi S, Ikeda Y, Nishino K, et al. The therapeutic effects of Goreisan, a traditional Japanese herbal medicine, on lower-limb lymphedema after lymphadenectomy in gynecologic malignancies: a case series study. Evid Based Complement Alternat Med. 2020;2020:6298293. https://doi.org/10.1155/2020/6298293.
Kitamura K, Iwase S, Komoike Y, Ogawa Y, Utsugi K, Yamamoto D, et al. Evidence-based practice guideline for the management of lymphedema proposed by the Japanese Lymphedema Society. Lymph Res Biol Publ Online. 2022. https://doi.org/10.1089/lrb.2021.0032.
Rupp J, Hadamitzky C, Henkenberens C, Christiansen H, Steinmann D, Bruns F. Frequency and risk factors for arm lymphedema after multimodal breast- conserving treatment of nodal positive breast Cancer—a long-term observation. Radiat Oncol. 2019;14:39. https://doi.org/10.1186/s13014-019-1243-y.
Desnyder SM, Yi M, Boccardo F, Feldman S, Klimberg VS, Smith M, et al. American Society of Breast Surgeons’ practice patterns for patients at risk and affected by breast cancer-related lymphedema. Ann Surg Oncol. 2021;28:5742–51. https://doi.org/10.1245/s10434-021-10494-0.
Zou L, Liu FH, Shen PP, Hu Y, Liu XQ, Xu YY, et al. The incidence and risk factors of related lymphedema for breast cancer survivors post-operation: a 2-year follow-up prospective cohort study. Breast Cancer. 2018;25:309–14. https://doi.org/10.1007/s12282-018-0830-3.
Nguyen TT, Hoskin TL, Habermann EB, Cheville AL, Boughey JC. Breast cancer-related lymphedema risk is related to multidisciplinary treatment and not surgery alone: results from a large cohort study. Ann Surg Oncol. 2017;24:2972–80. https://doi.org/10.1245/s10434-017-5960-x.
Shaitelman SF, Chiang YJ, Griffin KD, Desnyder SM, Smith BD, Schaverien MV, Kate YjC, Sarah DG. Radiation therapy targets and the risk of breast cancer-related lymphedema: a systematic review and network meta-analysis. Breast Cancer Res Treat. 2017;162:201–15. https://doi.org/10.1007/s10549-016-4089-0.
Bevilacqua JL, Kattan MW, Changhong Y, Koifman S, Mattos IE, Koifman RJ, et al. Nomograms for predicting the risk of arm lymphedema after axillary dissection in breast cancer. Ann Surg Oncol. 2012;19:2580–9. https://doi.org/10.1245/s10434-012-2290-x.
Basta MN, Fox JP, Kanchwala SK, Wu LC, Serletti JM, Kovach SJ, et al. Complicated breast cancer–related lymphedema: evaluating health care resource utilization and associated costs of management. Am J Surg. 2016;211:133–41. https://doi.org/10.1016/j.amjsurg.2015.06.015.
Mclaughlin SA, Wright MJ, Morris KT, Giron GL, Sampson MR, Brockway JP, et al. Prevalence of lymphedema in women with breast cancer 5 years after sentinel lymph node biopsy or axillary dissection: objective measurements. J Clin Oncol. 2008;26:5213–9. https://doi.org/10.1200/JCO.2008.16.3725.
Society for Ambulatory Anesthesia. Society for Ambulatory Anesthesia (SAMBA) statement on intravenous catheter placement, venipuncture and blood pressure measurements in the ipsilateral upper extremity after breast cancer surgery with and without axillary lymph node dissection; 2021. https://samba.memberclicks.net/assets/docs/SAMBA_Statements/SAMBA_Statement_IV-Breast-Surg.pdf. Accessed 3 Mar 2022.
Schisterman EF, Cole SR, Platt RW. Overadjustment bias and unnecessary adjustment in epidemiologic studies. Epidemiology. 2009;20:488–95. https://doi.org/10.1097/EDE.0b013e3181a819a1.
Yasunaga H. Real world data in Japan: chapter II the diagnosis procedure combination database. Ann Clin Epidemiol. 2019;1:76–9.
Konishi T, Fujiogi M, Sato A, Michihata N, Kumazawa R, Matsui H, et al. Short-Term outcomes following breast cancer surgery with and without neoadjuvant chemotherapy: A nationwide administrative database study in Japan. Ann Surg Oncol. 2022. https://doi.org/10.1245/s10434-021-11212-6.
Konishi T, Fujiogi M, Michihata N, Kumazawa R, Ohbe H, Matsui H, et al. Interstitial lung disorders following postoperative radiotherapy with concurrent or sequential hormonal therapy for breast cancer: a nationwide database study in Japan. Breast Cancer Publ Online. 2022. https://doi.org/10.1007/s12282-022-01346-0.
Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370:1453–7. https://doi.org/10.1016/S0140-6736(07)61602-X.
Yamana H, Moriwaki M, Horiguchi H, Kodan M, Fushimi K, Yasunaga H. Validity of diagnoses, procedures, and laboratory data in Japanese administrative data. J Epidemiol. 2017;27:476–82. https://doi.org/10.1016/j.je.2016.09.009.
Konishi T, Yoshimoto T, Michimasa F, Yamana H, Tanabe M, Seto Y, Yasunaga H. Validity of operative information in Japanese administrative data: a chart review-based analysis of 1221 cases at a single institution. Surg Today. 2022. https://doi.org/10.1007/s00595-022-02521-8 (Online ahead of print).
Shigemi D, Morishima T, Yamana H, Yasunaga H, Miyashiro I. Validity of initial cancer diagnoses in the Diagnosis Procedure Combination data in Japan. Cancer Epidemiol. 2021;74: 102016. https://doi.org/10.1016/j.canep.2021.102016.
Sato I, Yagata H, Ohashi Y. The accuracy of Japanese claims data in identifying breast cancer cases. Biol Pharm Bull. 2015;38:53–7. https://doi.org/10.1248/bpb.b14-00543.
Konishi T, Fujiogi M, Michihata N, Tanaka-Mizutani H, Morita K, Matsui H, et al. Breast cancer surgery in patients with schizophrenia: short-term outcomes from a nationwide cohort. Br J Surg. 2021;108:168–73. https://doi.org/10.1093/bjs/znaa070.
Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130–9. https://doi.org/10.1097/01.mlr.0000182534.19832.83.
Austin PC. A tutorial on multilevel survival analysis: methods, models and applications. Int Stat Rev. 2017;85:185–203. https://doi.org/10.1111/insr.12214.
Crowther MJ. Multilevel mixed-effects parametric survival analysis: estimation, simulation, and application. Stand Genomic Sci. 2019;19:931–49. https://doi.org/10.1177/1536867X19893639.
Komoike Y, Inokuchi M, Itoh T, Kitamura K, Kutomi G, Sakai T, Jinno H, Wada N, Ohsumi S, Mukai H, Japanese Breast Cancer Society. Japan Breast Cancer Society clinical practice guideline for surgical treatment of breast cancer. Breast Cancer. 2015;22:37–48. https://doi.org/10.1007/s12282-019-01030-w.
Thompson B, Gaitatzis K, de Janse de Jonge XJ, Blackwell R, Koelmeyer LA. Manual lymphatic drainage treatment for lymphedema: a systematic review of the literature. J Cancer Surviv. 2021;15:244–58. https://doi.org/10.1007/s11764-020-00928-1.
Weisskopf MG, Sparrow D, Hu H, Power MC. Biased exposure-health effect estimates from selection in cohort studies: are environmental studies at particular risk? Environ Health Perspect. 2015;123:1113–22. https://doi.org/10.1289/ehp.1408888.
Anton MM, Cortez-Cooper MY, DeVan AE, Neidre DB, Cook JN, Tanaka H. Cigarette smoking, regular exercise, and peripheral blood flow. Atherosclerosis. 2006;185:201–5. https://doi.org/10.1016/j.atherosclerosis.2005.05.034.
Zhu W, Li D, Li X, Ren J, Chen W, Gu H, et al. Association between adjuvant docetaxel-based chemotherapy and breast cancer-related lymphedema. Anticancer Drugs. 2017;28:350–5. https://doi.org/10.1097/CAD.0000000000000468.
Hayashi N, Kumamaru H, Isozumi U, Aogi K, Asaga S, Iijima K, Kadoya T, Kojima Y, Kubo M, Miyashita M, Miyata H, Nagahashi M, Niikura N, Ogo E, Tamura K, Tanakura K, Yamamoto Y, Yoshida M, Imoto S, Jinno H. Annual report of the Japanese Breast Cancer Registry for 2017. Breast Cancer. 2020;27:803–9. https://doi.org/10.1007/s12282-020-01139-3.
Sawaki M, Yamada A, Kumamaru H, Miyata H, Nakayama K, Shimizu C, Miyashita M, Honma N, Taira N, Saji S. Clinicopathological characteristics, practical treatments, prognosis, and clinical issues of older breast cancer patients in Japan. Breast Cancer. 2021;28:1–8. https://doi.org/10.1007/s12282-020-01188-8.
Yotsumoto D, Sagara Y, Kumamaru H, Niikura N, Miyata H, Kanbayashi C, Tsuda H, Yamamoto Y, Aogi K, Kubo M, Tamura K, Hayashi N, Miyashita M, Kadoya T, Saji S, Toi M, Imoto S, Jinno H. Trends in adjuvant therapy after breast-conserving surgery for ductal carcinoma in situ of breast: a retrospective cohort study using the National Breast Cancer Registry of Japan. Breast Cancer. 2022;29:1–8. https://doi.org/10.1007/s12282-021-01307-z.
Ferguson CM, Swaroop MN, Horick N, Skolny MN, Miller CL, Jammallo LS, et al. Impact of ipsilateral blood draws, injections, blood pressure measurements, and air travel on the risk of lymphedema for patients treated for breast cancer. J Clin Oncol. 2016;34:691–8. https://doi.org/10.1200/JCO.2015.61.5948.
Sibaud V, Lebœuf NR, Roche H, Belum VR, Gladieff L, Deslandres M, et al. Dermatological adverse events with taxane chemotherapy. Eur J Dermatol. 2016;26:427–43. https://doi.org/10.1684/ejd.2016.2833.
Lucci A, McCall LM, Beitsch PD, Whitworth PW, Reintgen DS, Blumencranz PW, et al. Surgical complications associated with sentinel lymph node dissection (SLND) plus axillary lymph node dissection compared with SLND alone in the American College of Surgeons Oncology Group trial Z0011. J Clin Oncol. 2007;25:3657–63. https://doi.org/10.1200/JCO.2006.07.4062.
Funding
This work was supported by grants from the Ministry of Health, Labour and Welfare, Japan (21AA2007 and 20AA2005) and the Ministry of Education, Culture, Sports, Science and Technology, Japan (20H03907).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
NM is an employee of the Department of Health Services Research in the Graduate School of Medicine at The University of Tokyo, which is supported by Tsumura & Co. The other authors have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Konishi, T., Tanabe, M., Michihata, N. et al. Risk factors for arm lymphedema following breast cancer surgery: a Japanese nationwide database study of 84,022 patients. Breast Cancer 30, 36–45 (2023). https://doi.org/10.1007/s12282-022-01395-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12282-022-01395-5