Abstract
Purpose of Review
Severe-acute respiratory coronavirus 2 (SARS-CoV-2) causing corona virus disease 2019 (COVID-19) has been the single most important pathogen driving health care delivery system for the last one and half years. Now, as the time is passing, many issues related to co-infections/secondary infections/superinfections in COVID-19 patients are emerging. The literature is getting enriched everyday by addition of reports from all over the world for the same. The purpose of this review is to decipher the plethora of fungal infections in COVID-19.
Recent Findings
COVID-19 infection along with it brought many risk factors namely lung injury, immunosuppression, need for oxygen therapy, monoclonal antibodies, steroid therapy, etc. which are known predisposing factors for fungal infections. Rather the extent and severity of fungal pathogens has been so much that it has led to new terminologies like CAC (COVID-19-associated Candida), CAPA (COVID-19-associated pulmonary aspergillosis) and CAM (COVID-19-associated mucormycosis). There is increase in invasiveness of Candida, prevalence of aspergillosis in COVID-19 damaged lung and outbreak of mucormycosis in COVID-19 patients resulting in “double trouble,” keeping laboratory personnel, clinicians, and intensivists on their toes in managing these patients.
Summary
Awareness and understanding regarding these possible complications is necessary to decrease the morbidity and mortality among patients. The COVID-19 and fungal coinfections may bring more insight into ways of pathogenesis of fungal infections, need for better antifungal agents, quick diagnostic modalities, and better management policies in the near future.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The World Health Organization (WHO) for the sixth time declared severe-acute respiratory coronavirus 2 (SARS-CoV-2) a public health emergency of international concern (pandemic) on January 30, 2020 [1]. As per the WHO corona virus disease 2019 (COVID-19) dashboard, the number of confirmed cases is 220,904,838 worldwide with 4,570,946 reported deaths, as of September 07, 2021 [2]. The clinical spectrum of SARS-CoV-2 infection has a wide range from being asymptomatic/pre-symptomatic to having mild, moderate, severe, or critical illness [3]. Severe illness is defined by an SpO2 < 94% on room air at sea level, a ratio of arterial partial pressure of oxygen to fraction of inspired oxygen (PaO2/FiO2) < 300 mm Hg, respiratory frequency > 30 breaths/min, or lung infiltrates > 50%. Persons with respiratory failure, septic shock, and/or multiple organ dysfunction are diagnosed as critically ill. Individuals with comorbid conditions like age > 65 years, cardiovascular disease, chronic lung disease, diabetes, obesity, chronic kidney disease, malignancy, etc., are likely to progress to severe/critical illness.
Coinfections or secondary infections are known to exist with viral pneumonia. A systematic review revealed that 1 in 4 patients with H1N1 infection had bacterial/fungi infection, during 2009 pandemic [4]. COVID-19 is no exception. A plethora of bacterial and fungal coinfections/superinfections/secondary infections have been reported in COVID-19 patients. It is not uncommon to have viral coinfections reports namely influenza A, respiratory syncytial virus, and dengue viral infection associated with COVID-19 patients [5••]. The course of disease is unpredictable with high individual variations. COVID-19 is known to act on angiotensin-converting enzyme 2 (ACE 2) receptors leading to involvement of not only lungs, but pancreas, endothelium, and especially platelets driving pro thrombotic activities. There is immune dysregulation in the form of derangement in pro inflammatory markers, cytokine levels, interferon (IFN) gamma expression, alteration in cluster of differentiation 4 (CD4) CD8 levels, in turn, affecting the natural innate immunity [6]. Considering the background, it is understandable that there will be a chance for other pathogens to co-infect. Hereby, we are discussing fungal pathogens-associated coinfection in brief.
COVID-19-Associated Candidiasis (CAC)
Fungal coinfection with Candida in COVID-19 patients is still underreported, and the risk factors associated are not directly linked to the SARS-CoV-2 infection. These are general risk factors like diabetes mellitus, abdominal surgery, renal failure requiring hemodialysis, triple lumen catheters, indwelling central venous catheters, parenteral nutrition, multiple antibiotics, etc., which make the patients in intensive care unit (ICU) and those on mechanical ventilation more vulnerable to develop fungal coinfections [7, 8]. Furthermore, need for extracorporeal membrane oxygenation (ECMO) consequent upon severe respiratory failure associated with COVID-19 is another predisposing factor [9]. Recently, it has been shown that C. albicans infection in users of removable dentures can upscale the morbidity and mortality associated with COVID-19 [10]. In COVID-19, it is postulated that disruption of intestinal mucosal barrier (enterocytes have increased expression of angiotensin converting enzyme-2 receptor to which SARS-CoV-2 binds) open doors for the translocation of Candida species from the gut lumen to the blood causing candidemia [11]. Gut mycobiota dysbiosis has been established in COVID-19 with significant lowering of gut fungal α-diversity and the relative abundance of the most altered gut fungal taxa [12]. The complete pathogenesis and immune dysregulation in COVID-19 patients harboring Candida is yet to see the light of day, noteworthy are the findings of impaired monocyte CD80 upregulation and nullified release of IL-6, tumor necrosis factor (TNF), interleukin (IL)-1a, and IL-1b signalling towards increased susceptibility for Candida albicans infection [13].
The most frequent fungal pathogen (in about 6 to 10% cases) recovered in this setting is Candida with an estimated mortality with invasive candidiasis being 19–40% [14, 15]. The non-albicans Candida (NAC) species including C. glabrata and C. auris either have inherent resistance to antifungals or soon acquire antifungal resistance are the real troublemakers [16]. COVID-19-associated candidiasis (CAC) can either be superficial or invasive with infection rates ranging from 0.7 to 23.5% [17,18,19,20,21,22]. C. albicans is the most rampant among invasive yeast infections in critically ill COVID-19 patients followed by C. auris, C. glabrata, C. parapsilosis, C. tropicalis, and others [16]. Heavy mortality has been seen with C. glabrata and C. auris. In a recent study, exceedingly high mortality to the tune of 83.3% despite antifungal treatment was seen in patients with candidaemia with C. auris and COVID-19 pneumonia [23].
Candida auris is a new emergent threat to global health because of its resistance to fluconazole and amphotericin B and limited availability of antifungals such as echinocandins in resource limited countries. In COVID-19 patients, its transmission by healthcare personnel can occur in case of erroneous and prolonged use of personal protective equipment which can lead to self-contamination and further transmission [21].
COVID-19-Associated Pulmonary Aspergillosis (CAPA)
Aspergillus is a ubiquitous fungus present in the soil and decaying vegetations. The most common Aspergillus species causing coinfection in COVID-19 patients is A. fumigatus followed by A. flavus [24]. There is a huge spectrum of infections caused by this fungus in human beings which includes invasive pulmonary aspergillosis (IPA), allergic bronchopulmonary aspergillosis (ABPA), chronic pulmonary aspergillosis (CPA), fungal asthma, chronic rhinosinusitis, and bronchitis. Of these, IPA is the most worrisome. As per our current understanding, danger-associated molecular patterns (DAMP) released during severe COVID-19 cause epithelial damage in the lungs and a cascade of inflammatory reactions [25]. Targeting of DAMP is believed to be a significant immunomodulatory strategy. Aspergillus cleaves fibrinogen and activates Toll-like receptor 4 (TLR4)/MyD88/Toll/interleukin-1 receptor (TIR)-domain-containing adapter-inducing interferon-β (TRIF) which results in activation of overlapping signalling pathways generating cytokines including IL-1 and IL-6.
The cardinal risk factor for developing CAPA is structural lung damage caused by chronic obstructive pulmonary disease (COPD) or asthma besides the use of corticosteroids, broad-spectrum antibiotics in severe COVID patients [25]. Interstitial pulmonary fibrosis is not a direct risk factor but some of these patients post COVID may need long-term steroids, which is another predisposing factor. In a recent study, influenza infection was established as an independent risk factor for IPA with a mortality of 45% in patients with influenza-associated IPA [26]. Efforts should be made to distinguish aspergillosis developing after severe COVID-19 pneumonia from that in patients with underlying chronic respiratory diseases [27]. The tsunami of COVID-19 forced conversion of general hospital wards into COVID facilities not truly meeting ICU specifications for adequate room ventilation, and air changes thereby increased the risk of Aspergillus exposure [28].
In a single-center prospective case series from Netherlands, a higher percentage of patients with COVID-19 were diagnosed with CAPA during the second wave of the pandemic as compared to the first wave (24.2% vs 15.2%) [29]. Many recent studies report high rates of CAPA in COVID-19 patients with ARDS to the tune of 20–35% with mortality ranging from 44.5 to 66.7% [30,31,32,33]. Azole resistance especially with Aspergillus fumigatus contributes to higher mortality rates making antifungal susceptibility testing (AFST) of utmost importance particularly in zones with high azole resistance [34]. AFST helps in initiating appropriate antifungal treatment and can be either phenotypic or genotypic using molecular techniques for detecting mutations associated with triazole resistance [35].
CAPA can be classified as possible/probable/proven aspergillosis according to the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) in an immunocompromised setting [36]. For proven diagnosis, fungal invasion needs histopathologic confirmation. A constellation of host factors, clinical features, and positive mycology diagnosis constitutes probable IPA. Existence of host factors and clinical features albeit histopathologic/mycology evidence makes the diagnosis as, possible IPA. These cannot be applied directly to the non-neutropenic patients in the ICU setup for whom Aspergillus ICU algorithm was established which could differentiate invasive pulmonary aspergillosis from mere colonization by aspergillus [37]. It is further stated that many patients who survive without treatment could just represent colonizations than being truly coinfections [38]. Proposed case definitions for influenza-associated pulmonary aspergillosis (IAPA) that may be considered for classifying of CAPA patients in ICU patients were given by an international team of experts where an entry criterion was proposed and not host factors [39]. The European Confederation for Medical Mycology and the International Society for Human and Animal Mycology (ECMM/ISHAM) has recently proposed consensus criteria for defining and grading CAPA into three grades: possible, probable, and proven and has also provided updated management recommendations [40].
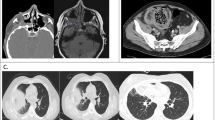
Diagnosing CAPA is a great challenge. The radiological features are not absolute. Radiology is varied showing irregular airways to centrilobular nodules to cavitary nodules and consolidation [41]. Galactomannan (GM) testing of bronchoalveolar lavage (BAL) fluids may not be available in many cases for the fear of aerosol-generation [42]. Tracheal aspirates and non-bronchoscopic lavage (NBL) specimens which are upper respiratory tract samples can be procured with ease; however, validation of GM testing on these samples is a concern [43]. Lahmer et al. believe that NBL obtained through deep bronchial suction in mechanical ventilated patients can serve as an alternative to BAL fluid for GM testing [44].
A large study was conducted from over 700 critically ill COVID-19 patients across the UK involving fungal biomarker testing on serum and respiratory samples and mycological examination of respiratory secretions [43]. Regular and repeat testing of serum and respiratory samples with a multitude of testing modalities was recommended for detecting CAPA. Gangneux et al. [45] have proposed to combine Aspergillus detection (culture and real-time quantitative polymerase chain reaction, PCR) in respiratory samples and serological detection of anti-Aspergillus antibody (enzyme-linked immunosorbent assay, ELISA, and immunoelectrophoresis) to distinguish chronic colonization from acute massive colonization. On a cohort of 45 COVID-19 patients, intubated and mechanically ventilated patients for ARDS, modified AspICU algorithm (incorporating PCR, serology, and angioinvasion biomarkers) was used for categorization into no infection, colonization, putative invasive aspergillosis (IA), probable IA, and proven IA.
For accurately establishing the incidence of invasive pulmonary aspergillosis in COVID-19 patients, there is a dire need for autopsy studies or those evaluating targeted post-mortem lung biopsies [46].
COVID-19-Associated Mucormycosis (CAM)
As we sail through the current pandemic coming in waves, cases of COVID-19-associated mucormycosis (CAM) are being frequently added to the literature. The incidence definitely increased enormously during the second wave in comparison with the first wave [47]. CAM can occur any time after the detection of COVID or within a short time frame usually within 2 weeks of post COVID recovery [48]. In fact, combined pulmonary aspergillosis and mucormycosis as secondary complications of COVID-19 are on record.
Mucormycosis is a potentially fatal infection [49]. The fungus is well known to cause tissue gangrene due to its angioinvasive nature leading to vessel thrombosis. This renders blackish discoloration imparting it the name of black fungus which is actually a misnomer as phaeoid fungi are true black fungi containing melanin pigment. The organisms isolated have their origin from the Mucorales order and comprise of Mucor, Rhizopus, Abdidia, Rhizomucor, Apophysomyces, Cunninghumella, and Saksenaea [50, 51]. The most common clinical isolate is Rhizopus [52, 53]. Mucormycosis is classified as rhinocerebral/sino-orbital, pulmonary, cutaneous, gastrointestinal, and disseminated according to the affected site [54]. Mucormycosis can have deleterious complications like cavernous sinus thrombosis, osteomyelitis, multisystem involvement, and mortality [55].
A plethora of risk factors for mucormycosis includes uncontrolled diabetes mellitus, immunocompromised host, prolonged medication with glucocorticoids, hematological malignancies, hematopoietic stem cell transplantation, human immunodeficiency virus-acquired immunodeficiency syndrome (HIV-AIDS), etc. [56]. In a single-center, retrospective study of 70 patients with CAM presenting to the emergency department with acute or recent COVID-19, 70% of the patients were diabetic [57]. Diabetic ketoacidosis and ketonemia and ketoacidosis in patients with COVID-19 sans diabetes predispose to CAM [58]. Use of corticosteroids blunts the action of insulin leading to hyperglycemia and ketoacidosis [59]. SARS-CoV-2 is well-known to induce a diabetogenic state by binding to the beta cells of the pancreatic islets which have ACE2 receptors for which the virus has affinity. In fact, the SARS-CoV-2 has tropism for many systems including respiratory system, gastrointestinal tract, cardiovascular system, liver, nervous system, ocular system, etc. [58]. The Indian tropical and humid climate serves as an icing on the cake having a huge load of mucor spores in the environment [56]. India has the highest number of cases of mucormycosis reported worldwide [60]. Use of humidifiers in the ICUs has also been linked to CAM; on the contrary, some authors believe humidifier bottled water undergoes incessant agitation due to passage of oxygen; and in this situation, even if the water is contaminated with mucor, the fungus cannot produce spores, and hyphae are not the inoculating medium [56]. Increased pathogenicity of Mucormycetes has also been linked to the use of voriconazole for suspected invasive aspergillosis [61].
Blood acidosis in severe form of COVID-19 and raised serum ferritin also cause susceptibility to mucormycosis [62]. This along with hyperglycemia, low pH, and high iron decrease the phagocytic activity of leucocytes. There is enhancement in the expression of GRP-78 (glucose receptor protein-78) present on endothelial cells and fungal ligand spore-coating homolog protein (CotH) on mucor whose interaction propels Mucormycetes-induced angioinvasion and tissue necrosis [63]. Furthermore, the GRP-78 binding is common to both the new variants of SARS-CoV2 (B.1.1.7 and B.6.117) and Mucor [64].
Immune dysregulation seen in COVID makes the host neutrophils incompetent to release a burst of oxy-free radicals which destroy the hyphae in an immunocompetent person [56]. Although there is neutrophilia, the neutrophils are immature as they are released prematurely from the bone marrow in COVID-19. Increased expression of inflammatory cytokines and decrease in CD4 and CD8 T cells causing impaired cell-mediated immune response also increases the susceptibility for CAM [65, 66]. A significant decrease in lymphocyte count and increase in neutrophil count with imposed cytokine storm has invariably been observed in individuals with severe COVID-19 and coinfections [67].
A large multicenter retrospective study across India revealed a CAM prevalence of 0.27% among hospitalized COVID-19 patients and a prevalence of 1.6% in the ICUs [68••]. There was a 2.1-fold rise in mucormycosis during the study period (September–December 2020) compared with September–December 2019. Uncontrolled diabetes mellitus was found to be the most common risk factor with newly detected diabetes mellitus being more frequent. Compatible clinical and radiologic manifestations of mucormycosis with direct microscopic visualization of hyphae or isolation of Mucorales in the tissue or sterile body fluids of the patient established mucormycosis.
Rhino‑orbital‑cerebral mucormycosis (ROCM) is the most frequently observed manifestation of CAM [69]. Eighty-one percent of ROCM-CAM occurred in the Indian subcontinent [70]. Proposed staging and customized management approach for possible, probable, and proven COVID‑19‑associated ROCM based upon ECMM-MSG ERC guidelines have been given [71•]. A large Indian study encompassing 2826 ROCM-CAM patients (Collaborative OPAI‑IJO Study on Mucormycosis in COVID‑19–COSMIC study) found majority of the patients were diagnosed at stage 3 with orbit being involved with ROCM symptoms occurring between day 10 and day 15 post COVID diagnosis; however delayed presentation up to 3 months can be seen [70].
Symptomatology of CAM comprises of sinusitis—nasal blockade or congestion, nasal discharge (blackish/bloody), blurred vision or diplopia, localized pain on the cheek bone, unilateral facial pain, numbness or swelling, blackish discoloration over bridge of nose/palate, toothache, loosening of teeth, jaw involvement, fever, skin lesions—thrombosis and necrosis (eschar), chest pain, pleural effusion, hemoptysis, and worsening of respiratory symptoms [72]. Gastrointestinal (GI) tract involvement in CAM although unusual can present with fever, nausea, abdominal pain, GI bleeding and perforation [73].
Biomarkers like beta-d-glucan and galactomannan, which are useful diagnostic aids for invasive aspergillosis are not that reliable for diagnosing mucormycosis [74]. The diagnosis relies upon microscopic observation of characteristic broad ribbon like hyphae with right angle branching or microbiology culture or molecular techniques. When pulmonary-CAM is suspected, lung biopsy can be done but is invasive and often deferred in high-risk ICU patients on mechanical ventilation in whom BAL is a good option [75]. Routine tests like vision, pupil, ocular motility, and sinus tenderness can be helpful in picking up ROCM early [52]. MRI is a useful modality for diagnosing possible intracranial extension in ROCM [76].
Basic fundamentals for managing CAM effectively are rapid diagnosis, reversal of underlying predisposing factors wherever possible, surgical debridement, and appropriate antifungal therapy [77]. Surgical debridement of the infected tissue must be undertaken as soon as possible, and aggressive surgical approach, once the diagnosis of mucormycosis is confirmed, is associated with good outcomes [78]. Amphotericin-B deoxycholate/liposomal amphotericin is the antifungal therapy of choice [79]. Control of diabetes and diabetic ketoacidosis with discontinuation or dose reduction of steroids are helpful measures. The patient needs to be monitored clinically and by radioimaging for assessment of response.
In randomized evaluation of Covid-19 therapy (RECOVERY) trial of dexamethasone in hospitalized patients with Covid-19, survival benefit was observed among those requiring supplemental oxygen at enrolment vis-a-vis those patients who did not require oxygen wherein no benefit rather possible harm was noted [80]. Erratic use of glucocorticoids for mild disease or in doses and durations above standard recommendations is a threat to development of CAM which needs to be curbed.
Other Opportunist Fungi in COVID-19
The COVID-19 pandemic has witnessed patients with coinfection with other fungal pathogens like Cryptococcus, Histoplasma, and Pneumocystis.
Cryptococcosis is a fungal infection caused by opportunistic fungal pathogen Cryptococcus, species C. neoformans and C. gattii. Cryptococcus neoformans is known to cause fatal meningoencephalitis in immunocompromised patients with disseminated infection. Recently, cases of cryptococcal meningoencephalitis in patients with SARS-CoV-2 infection have been reported [81, 82]. Heller et al. [82] reported cryptococcal meningoencephalitis in a young male who was HIV-positive. They emphasized that CD4:CD8 T cell ratio tends to be preserved in patients with COVID-19-associated lymphopenia while a fall in the ratio is observed in patients with advanced HIV infection. Cryptococcemia has been reported in a COVID-19 patient with several comorbidities who received tocilizumab and corticosteroids [83]. Cryptoccocus can cause cutaneous, pulmonary, or CNS involvement. A patient with ulcero-necrotic cutaneous lesions and neurological symptoms due to Cryptococcus with bone metastasis due to prostate cancer is on record [84]. This patient died during the outbreak of SARS-CoV-2 in Lombardy, Italy where the largest epidemic outbreak developed.
Macedo et al. [85] reported two cases of acute pulmonary histoplasmosis who had COVID-19 before the onset of histoplasmosis symptoms. The diagnosis was challenging in these cases where the authors resorted to western blot and PCR to clinch the diagnosis of histoplasmosis. The clinicians should have a high index of suspicion especially in patients hailing from endemic areas with fever and cough post COVID-19 recovery. Disseminated histoplasmosis associated with COVID-19 in patient with HIV has been documented [86, 87]. Isavuconazole has shown to be effective in cases of invasive fungal infection due to Cryptococcus and Histoplasma [88].
Isolated cases with SARS-CoV-2 and Pneumocystis jirovecii coinfection are on record [89]. They highlight the challenges associated with diagnosis of Pneumocystis pneumonia as the clinical features may be common thus reiterating additional diagnostic testing for P. jirovecii especially in patients with elevated lactate dehydrogenase, cystic findings on chest-computed tomography which indicate coinfection. Alanio et al. [90] found a surprisingly high percentage (10/108 patients, 9.3%) of critically ill COVID-19 patients coinfected with P. jirovecii. Other than these, bloodstream infections due to Saccharomyces cerevisiae have been described in two COVID-19 patients in ICU settings. Both the patients were receiving probiotic yeast supplementation [91].
Conclusion
There have been concerns regarding existence of real threat related to increase in number of secondary infections, i.e., whether they are due to COVID-19 or just due to increased hospitalizations, ICU admissions, intensive care, or due to compromised hospital infection control practices considering COVID-19 exigency. Whatever the reason, the existence or increase in number of fungal infections associated with COVID-19 pandemic cannot be ignored. Challenges do exist especially related to diagnosis of secondary infections in COVID-19. It is the right time to develop a standardized methodology for diagnosing these infections. There is need for clinicians to be aware of complications such infections can cause, and also, there is need to strengthen pathology and microbiology laboratories. There is need to formulate effective practical guidelines for healthcare workers processing samples while doing direct examination, culture, or serological analysis especially related to aerosol-generating steps. Increased workload along with biosafety, appropriate training of its personnel, and logistic workout should be considered a priority to deal with the pandemic infections in future.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
World Health Organization. Available at: https://www.who.int/director-general/ speeches/detail/who-director-general-s-opening-remarks-at-the -media-briefing-on-covid-19–27-July-2020.
World Health Organization. WHO Coronavirus Disease (COVID-19) Dashboard 2020. https://covid19.who.int/ [accessioned September 7th, 2021].
National Institutes of Health. Clinical spectrum of SARS-CoV-2 infection. Available at: https://www.covid19treatmentguidelines.nih.gov/overview/clinical-spectrum [accessioned July 3, 2021].
MacIntyre CR, Chughtai AA, Barnes M, Ridda I, Seale H, Toms R, et al. The role of pneumonia and secondary bacterial infection in fatal and serious outcomes of pandemic influenza a(H1N1)pdm09. BMC Infect Dis. 2018;18:637.
Lansbury L, Lim B, Baskaran V, Lim WS. Co-infections in people with COVID-19: a systematic review and meta-analysis. J Infect. 2020;81(2):266–75. This article evaluates the burden of co-infections in patients with COVID-19.
Pemán J, Ruiz-Gaitán A, García-Vidal C, Salavert M, Ramírez P, Puchades F, García-Hita M, Alastruey-Izquierdo A, Quindós G. Fungal co-infection in COVID-19 patients: should we be concerned? Rev Iberoam Micol. 2020;37(2):41–6.
Al-Hatmi AMS, Mohsin J, Al-Huraizi A, Khamis F. COVID-19 associated invasive candidiasis. J Infect. 2021;82(2):e45–6.
Pappas PG, Lionakis MS, Arendrup MC, Ostrosky-Zeichner L, Kullberg BJ. Invasive candidiasis. Nat Rev Dis Primers. 2018;4:18026.
Cavayas YA, Yusuff H, Porter R. Fungal infections in adult patients on extracorporeal life support. Crit Care. 2018;22(1):98.
Jerônimo LS Esteves Lima RP Suzuki TYU Discacciati JAC Bhering CLB. Oral candidiasis and COVID-19 in users of removable dentures: is special oral care needed? Gerontology 2021:1–6.
Nucci M, Barreiros G, Guimarães LF, Deriquehem VAS, Castiñeiras AC, Nouér SA. Increased incidence of candidemia in a tertiary care hospital with the COVID-19 pandemic. Mycoses. 2021;64(2):152–6.
Lv L, Gu S, Jiang H, Yan R, Chen Y, Chen Y, et al. Gut mycobiota alterations in patients with COVID-19 and H1N1 infections and their associations with clinical features. Commun Biol. 2021;4(1):480.
Moser D, Biere K, Han B, Hoerl M, Schelling G, Choukér A, Woehrle T. COVID-19 impairs immune response to Candida albicans. Front Immunol. 2021;12:640644.
Lortholary O, Renaudat C, Sitbon K, Madec Y, Denoeud-Ndam L, Wolff M, et al. Worrisome trends in incidence and mortality of candidemia in intensive care units (Paris area, 2002–2010). Intensive Care Med. 2014;40(9):1303–12.
Kullberg BJ, Arendrup MC. Invasive candidiasis. N Engl J Med. 2015;373(15):1445–56.
Arastehfar A, Carvalho A, Nguyen MH, Hedayati MT, Netea MG, Perlin DS, et al. COVID-19-associated candidiasis (CAC): an underestimated complication in the absence of immunological predispositions? J Fungi (Basel). 2020;6(4):211.
Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–13.
Salehi M, Ahmadikia K, Mahmoudi S, Kalantari S, Jamalimoghadamsiahkali S, Izadi A, et al. Oropharyngeal candidiasis in hospitalised COVID-19 patients from Iran: species identification and antifungal susceptibility pattern. Mycoses. 2020;63(8):771–8.
White PL Dhillon R Cordey A Hughes H Faggian F Soni S et al. A national strategy to diagnose COVID-19 associated invasive fungal disease in the ICU. Clin Infect Dis 2020:ciaa1298.
Antinori S, Bonazzetti C, Gubertini G, Capetti A, Pagani C, Morena V, et al. Tocilizumab for cytokine storm syndrome in COVID-19 pneumonia an increased risk for candidemia. Autoimmun Rev. 2020;19(7):102564.
Chowdhary A Tarai B Singh A Sharma A. Multidrug-resistant Candida auris infections in critically Ill coronavirus disease patients, India, April-July 2020. Emerg Infect Dis 2020;26(11):2694–6. The paper highlights the role of hospital acquired Candida auris blood stream infections in patients with COVID-19.
Garcia-Vidal C, Sanjuan G, Moreno-García E, Puerta-Alcalde P, Garcia-Pouton N, Chumbita M, et al. Incidence of co-infections and superinfections in hospitalized patients with COVID-19: a retrospective cohort study. Clin Microbiol Infect. 2021;27(1):83–8.
Villanueva-Lozano H, Treviño-Rangel RJ, González GM, Ramírez-Elizondo MT, Lara-Medrano R, Aleman-Bocanegra MC, et al. Outbreak of Candida auris infection in a COVID-19 hospital in Mexico. Clin Microbiol Infect. 2021;27(5):813–6.
Lai CC, Yu WL. COVID-19 associated with pulmonary aspergillosis: a literature review. J Microbiol Immunol Infect. 2021;54(1):46–53.
Arastehfar A, Carvalho A, van de Veerdonk FL, Jenks JD, Koehler P, Krause R, et al. COVID-19-associated pulmonary aspergillosis (CAPA)-from immunology to treatment. J Fungi (Basel). 2020;6(2):91.
Schauwvlieghe AFAD, Rijnders BJA, Philips N, Verwijs R, Vanderbeke L, Van Tienen C, et al. Invasive aspergillosis in patients admitted to the intensive care unit with severe influenza: a retrospective cohort study. Lancet Respir Med. 2018;6(10):782–92.
Fekkar A, Poignon C, Blaize M, Lampros A. Fungal infection during COVID-19: does aspergillus mean secondary invasive aspergillosis? Am J Respir Crit Care Med. 2020;202(6):902–3.
Armstrong-James D, Youngs J, Bicanic T, Abdolrasouli A, Denning DW, Johnson E, et al. Confronting and mitigating the risk of COVID-19 associated pulmonary aspergillosis. Eur Respir J. 2020;56(4):2002554.
Meijer EFJ, Dofferhoff ASM, Hoiting O, Meis JF. COVID-19-associated pulmonary aspergillosis: a prospective single-center dual case series. Mycoses. 2021;64(4):457–64.
van Arkel ALE, Rijpstra TA, Belderbos HNA, van Wijngaarden P, Verweij PE, Bentvelsen RG. COVID-19-associated pulmonary aspergillosis. Am J Respir Crit Care Med. 2020;202(1):132–5.
Koehler P, Cornely OA, Böttiger BW, Dusse F, Eichenauer DA, Fuchs F, et al. COVID-19 associated pulmonary aspergillosis. Mycoses. 2020;63(6):528–34.
Alanio A, Dellière S, Fodil S, Bretagne S, Mégarbane B. Prevalence of putative invasive pulmonary aspergillosis in critically ill patients with COVID-19. Lancet Respir Med. 2020;8(6):e48–9.
Rutsaert L, Steinfort N, Van Hunsel T, Bomans P, Naesens R, Mertes H, et al. COVID-19-associated invasive pulmonary aspergillosis. Ann Intensive Care. 2020;10(1):71.
Lestrade PPA, Meis JF, Melchers WJG, Verweij PE. Triazole resistance in Aspergillus fumigatus: recent insights and challenges for patient management. Clin Microbiol Infect. 2019;25(7):799–806.
Mohamed A, Rogers TR, Talento AF. COVID-19 associated invasive pulmonary aspergillosis: diagnostic and therapeutic challenges. J Fungi (Basel). 2020;6(3):115.
Donnelly JP, Chen SC, Kauffman CA, Steinbach WJ, Baddley JW, Verweij PE, et al. Revision and update of the consensus definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer and the Mycoses Study Group Education and Research Consortium. Clin Infect Dis. 2020;71(6):1367–76.
Blot SI, Taccone FS, Van den Abeele AM, Bulpa P, Meersseman W, Brusselaers N, et al. A clinical algorithm to diagnose invasive pulmonary aspergillosis in critically ill patients. Am J Respir Crit Care Med. 2012;186(1):56–64.
Machado M, Valerio M, Álvarez-Uría A, Olmedo M, Veintimilla C, Padilla B, et al. Invasive pulmonary aspergillosis in the COVID-19 era: an expected new entity. Mycoses. 2021;64(2):132–43.
Verweij PE, Rijnders BJA, Brüggemann RJM, Azoulay E, Bassetti M, Blot S, et al. Review of influenza-associated pulmonary aspergillosis in ICU patients and proposal for a case definition: an expert opinion. Intensive Care Med. 2020;46(8):1524–35.
Koehler P, Bassetti M, Chakrabarti A, Chen SCA, Colombo AL, Hoenigl M, et al. Defining and managing COVID-19-associated pulmonary aspergillosis: the 2020 ECMM/ISHAM consensus criteria for research and clinical guidance. Lancet Infect Dis. 2021;21(6):e149–62.
Marr KA, Platt A, Tornheim JA, Zhang SX, Datta K, Cardozo C, et al. Aspergillosis complicating severe coronavirus disease. Emerg Infect Dis. 2021;27(1):18–25.
Wahidi MM, Lamb C, Murgu S, Musani A, Shojaee S, Sachdeva A, et al. Statement on the use of bronchoscopy and respiratory specimen collection in patients with suspected or confirmed COVID-19 infection. J Bronchology Interv Pulmonol. 2020;27(4):e52–4.
Borman AM, Palmer MD, Fraser M, Patterson Z, Mann C, Oliver D, et al. COVID-19-associated invasive aspergillosis: data from the UK National Mycology Reference Laboratory. J Clin Microbiol. 2020;59(1):e02136-e2220.
Lahmer T, Kriescher S, Herner A, Rothe K, Spinner CD, Schneider J, et al. Invasive pulmonary aspergillosis in critically ill patients with severe COVID-19 pneumonia results from the prospective AspCOVID-19 study. PLoS One. 2021;16(3):e0238825.
Gangneux JP, Reizine F, Guegan H, Pinceaux K, Le Balch P, Prat E, et al. Is the COVID-19 pandemic a good time to include aspergillus molecular detection to categorize aspergillosis in ICU patients? A monocentric experience. J Fungi (Basel). 2020;6(3):105.
Yusuf E, Vonk A, van den Akker JPC, Bode L, Sips GJ, Rijnders BJA, et al. Frequency of positive aspergillus tests in COVID-19 patients in comparison to other patients with pulmonary infections admitted to the intensive care unit. J Clin Microbiol. 2021;59(3):e02278-e2320.
Raut A, Huy NT. Rising incidence of mucormycosis in patients with COVID-19: another challenge for India amidst the second wave? Lancet Respir Med. 2021;S2213–2600(21):00265–74.
Johnson AK, Ghazarian Z, Cendrowski KD, Persichino JG. Pulmonary aspergillosis and mucormycosis in a patient with COVID-19. Med Mycol Case Rep. 2021;32:64–7.
Selarka L Sharma S Saini D Sharma S Batra A Waghmare VT et al. Mucormycosis and COVID-19: an epidemic within a pandemic in India. Mycoses 2021. https://doi.org/10.1111/myc.13353
Shah K, Dave V, Bradoo R, Shinde C, Prathibha M. Orbital exenteration in rhino-orbito-cerebral mucormycosis: a prospective analytical study with scoring system. Indian J Otolaryngol Head Neck Surg. 2019;71(2):259–65.
Lee AS, Lee PWY, Allworth A, Smith T, Sullivan TJ. Orbital mycoses in an adult subtropical population. Eye (Lond). 2020;34(9):1640–7.
Revannavar SM, Supriya PS, Samaga L, Vineeth VK. COVID-19 triggering mucormycosis in a susceptible patient: a new phenomenon in the developing world? BMJ Case Rep. 2021;14(4):e241663.
Maini A, Tomar G, Khanna D, Kini Y, Mehta H, Bhagyasree V. Sino-orbital mucormycosis in a COVID-19 patient: a case report. Int J Surg Case Rep. 2021;82:105957.
Sen M, Lahane S, Lahane TP, Parekh R, Honavar SG. Mucor in a viral land: a tale of two pathogens. Indian J Ophthalmol. 2021;69(2):244–52.
Bhatt K, Agolli A, Patel MH, Garimella R, Devi M, Garcia E, et al. High mortality co-infections of COVID-19 patients: mucormycosis and other fungal infections. Discoveries Craiova. 2021;9(1):e126.
Gupta A, Sharma A, Chakrabarti A. The emergence of post-COVID-19 mucormycosis in India: can we prevent it? Indian J Ophthalmol. 2021;69(7):1645–7.
Ramaswami A Sahu AK Kumar A Suresh S Nair A Gupta D et al. COVID-19 associated mucormycosis presenting to the emergency department—an observational study of 70 patients. QJM 2021:hcab190.
Pandiar D, Kumar NS, Anand R, Kamboj M, Narwal A, Shameena PM. Does COVID 19 generate a milieu for propagation of mucormycosis? Med Hypotheses. 2021;152:110613.
Dallalzadeh LO Ozzello DJ Liu CY Kikkawa DO Korn BS. Secondary infection with rhino-orbital cerebral mucormycosis associated with COVID-19. Orbit 2021:1–4.
John TM, Jacob CN, Kontoyiannis DP. When uncontrolled diabetes mellitus and severe COVID-19 converge: the perfect storm for mucormycosis. J Fungi Basel. 2021;7(4):298.
Soman R, Sunavala A. Post COVID-19 Mucormycosis—from the frying pan into the fire. J Assoc Physicians India. 2021;69(1):13–4.
Pakdel F Ahmadikia K Salehi M Tabari A Jafari R Mehrparvar G et al. Mucormycosis in patients with COVID-19: a cross-sectional descriptive multicentre study from Iran. Mycoses 2021:https://doi.org/10.1111/myc.13334. https://doi.org/10.1111/myc.13334.
Sarda R Swain S Ray A Wig N. COVID-19 associated mucormycosis: an epidemic within a pandemic. QJM 2021:hcab165. https://doi.org/10.1093/qjmed/hcab165.
Chandra S, Rawal R. The surge in Covid-related mucormycosis. J Infect. 2021;S0163–4453(21):00288–97.
Song G, Liang G, Liu W. Fungal co-infections associated with global COVID-19 pandemic: a clinical and diagnostic perspective from China. Mycopathologia. 2020;185(4):599–606.
Verma DK, Bali RK. COVID-19 and mucormycosis of the craniofacial skeleton: causal, contributory or coincidental? J Maxillofac Oral Surg. 2021;20(2):1–2.
Pasero D Sanna S Liperi C Piredda D Branca GP Casadio L et al. A challenging complication following SARS-CoV-2 infection: a case of pulmonary mucormycosis. Infection 2020:1–6.
Patel A Agarwal R Rudramurthy SM Shevkani M Xess I Sharma R, et al. Multicenter epidemiologic study of coronavirus disease-associated mucormycosis, India. Emerg Infect Dis 2021;27(9). https://doi.org/10.3201/eid2709.210934. A large multicentre retrospective study from India comparing the epidemiology and outcomes between CAM and non-CAM patients.
Mahalaxmi I, Jayaramayya K, Venkatesan D, Subramaniam MD, Renu K, Vijayakumar P, et al. Mucormycosis: an opportunistic pathogen during COVID-19. Environ Res. 2021;201:111643. https://doi.org/10.1016/j.envres.2021.111643.
Sen M, Honavar SG, Bansal R, Sengupta S, Rao R, Kim U, et al. Epidemiology, clinical profile, management, and outcome of COVID-19-associated rhino-orbital-cerebral mucormycosis in 2826 patients in India - Collaborative OPAI-IJO Study on Mucormycosis in COVID-19 (COSMIC), Report 1. Indian J Ophthalmol. 2021;69(7):1670–92.
Honavar SG. Code Mucor: Guidelines for the diagnosis, staging and management of rhino-orbito-cerebral mucormycosis in the setting of COVID-19. Indian J Ophthalmol. 2021;69(6):1361–5. ROCM has implications on patient survival in COVID-19 patients and this editorial provides a complete update.
Indian Council of Medical research dashboard. https://www.icmr.gov.in/pdf/covid/techdoc/mucormycosis [accessioned July 21, 2021].
Monte Junior ESD, Santos MELD, Ribeiro IB, Luz GO, Baba ER, Hirsch BS, et al. Rare and fatal gastrointestinal Mucormycosis (Zygomycosis) in a COVID-19 patient: a case report. Clin Endosc. 2020;53(6):746–9.
Garg D, Muthu V, Sehgal IS, Ramachandran R, Kaur H, Bhalla A, et al. Coronavirus disease (Covid-19) associated mucormycosis (CAM): Case report and systematic review of literature. Mycopathologia. 2021;186(2):289–98.
Rothe K, Braitsch K, Okrojek R, Heim M, Rasch S, Verbeek M, et al. Clinical and microbiological features and outcomes of mucormycosis in critically ill patients. Int J Infect Dis. 2021;S1201–9712(21):00555–65. https://doi.org/10.1016/j.ijid.2021.06.066.
Awal SS, Biswas SS, Awal SK. Rhino-orbital mucormycosis in COVID-19 patients—a new threat? Egypt J Radiol Nucl Med. 2021;52:152.
Khatri A, Chang KM, Berlinrut I, Wallach F. Mucormycosis after Coronavirus disease 2019 infection in a heart transplant recipient - Case report and review of literature. J Mycol Med. 2021;31(2): 101125. https://doi.org/10.1016/j.mycmed.2021.101125.
Sharma S, Grover M, Bhargava S, Samdani S, Kataria T. Post coronavirus disease mucormycosis: a deadly addition to the pandemic spectrum. J Laryngol Otol. 2021;135(5):442–7.
Maini A, Tomar G, Khanna D, Kini Y, Mehta H, Bhagyasree V. Sino-orbital mucormycosis in a COVID-19 patient: a case report. Int J Surg Case Rep. 2021;82:105957. https://doi.org/10.1016/j.ijscr.2021.105957.
RECOVERY Collaborative Group Horby P Lim WS Emberson JR Mafham M, Bell JL, et al. Dexamethasone in hospitalized patients with Covid-19. N Engl J Med 2021 ;384(8):693–704
Ghanem H Sivasubramanian G. Cryptococcus neoformans meningoencephalitis in an immunocompetent patient after COVID-19 infection. Case Rep Infect Dis 2021. https://doi.org/10.1155/2021/5597473
Heller HM, Gonzalez RG, Edlow BL, Ard KL, Gogakos T. Case 40–2020: A 24-year-old man with headache and Covid-19. N Engl J Med. 2020;383(26):2572–80.
Khatib MY, Ahmed AA, Shaat SB, Mohamed AS, Nashwan AJ. Cryptococcemia in a patient with COVID-19: a case report. Clin Case Rep. 2020;9(2):853–5.
Passerini M, Terzi R, Piscaglia M, Passerini S, Piconi S. Disseminated cryptococcosis in a patient with metastatic prostate cancer who died in the coronavirus disease 2019 (COVID-19) outbreak. Cureus. 2020;12(5):e8254.
de Macedo PM, Freitas AD, Bártholo TP, Bernardes-Engemann AR, Almeida MA, Almeida-Silva F, et al. Acute pulmonary histoplasmosis following COVID-19: novel laboratorial methods aiding diagnosis. J Fungi (Basel). 2021;7(5):346.
Basso RP, Poester VR, Benelli JL, Stevens DA, Zogbi HE, Vasconcellos ICDS, et al. COVID-19-associated histoplasmosis in an AIDS patient. Mycopathologia. 2021;186(1):109–12.
Messina FA, Marin E, Caceres DH, Romero M, Depardo R, Priarone MM, et al. Coronavirus disease 2019 (COVID-19) in a patient with disseminated histoplasmosis and HIV—a case report from Argentina and literature review. J Fungi (Basel). 2020;6(4):275.
Cafardi J Haas D Lamarre T Feinberg J. Opportunistic fungal infection associated with COVID-19. Open Forum Infect Dis 2021. https://doi.org/10.1093/ofid/ofab016
Menon AA, Berg DD, Brea EJ, Deutsch AJ, Kidia KK, Thurber EG, et al. A case of COVID-19 and Pneumocystis jirovecii coinfection. Am J Respir Crit Care Med. 2020;202(1):136–8.
Alanio A, Dellière S, Voicu S, Bretagne S, Mégarbane B. The presence of Pneumocystis jirovecii in critically ill patients with COVID-19. J Infect. 2021;82(4):84–123.
Ventoulis I, Sarmourli T, Amoiridou P, Mantzana P, Exindari M, Gioula G, et al. Bloodstream infection by Saccharomyces cerevisiae in two COVID-19 patients after receiving supplementation of saccharomyces in the ICU. J Fungi. 2020;6:98.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Conflict of Interest
Reetu Kundu and Nidhi Singla declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on COVID-19 and Fungal Infections
Rights and permissions
About this article
Cite this article
Kundu, R., Singla, N. COVID-19 and Plethora of Fungal Infections. Curr Fungal Infect Rep 16, 47–54 (2022). https://doi.org/10.1007/s12281-022-00432-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12281-022-00432-2