Abstract
Purpose of Review
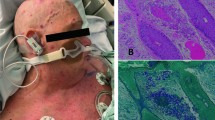
This review summarizes epidemiological risk factors, clinical manifestations, diagnosis, and treatment of common emerging fungal infections that are associated with cutaneous manifestations, in immunocompromised patients including solid organ transplant and hematopoietic cell transplant recipients.
Recent Findings
Immunocompromised patients including transplant recipients are at an increased risk of invasive fungal disease due to emerging fungi, such as mucormycetes and Scedosporium spp. Although cutaneous involvement is common, there is a great degree of variation in clinical manifestations, diagnostic techniques, and more importantly, treatment with antifungals.
Summary
The cutaneous manifestations of emerging fungal pathogens in immunocompromised patients can be localized or part of a disseminated disease. These fungal infections are remarkable for their varying resistance to antifungals. It is essential for clinicians to be knowledgeable about these infections as early treatment might improve outcomes including survival.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Wisplinghoff H, Bischoff T, Tallent SM, Seifert H, Wenzel RP, Edmond MB. Nosocomial bloodstream infections in US hospitals: analysis of 24,179 cases from a prospective nationwide surveillance study. Clin Infect Dis. 2004;39:309–17.
Low CY, Rotstein C. Emerging fungal infections in immunocompromised patients. F1000 Med Rep. 2011;3:14. https://doi.org/10.3410/M3-14.
Murray PR. Manual of Clinical Microbiology. 7th ed. Washington, DC: ASM Press; 1999. p. 1173.
Crissey JT, Lang H, Parrish LC. Manual of Medical Mycology. Cambridge: Blackwell Scientific; 1995. p. 263.
•• Shoham S, Dominguez EA, AST infectious diseases Community of Practice. Emerging fungal infections in solid organ transplant recipients: guidelines of the American Society of Transplantation infectious diseases Community of Practice. Clin Transpl. 2019;33:e13525 Most recently updated set of guidelines from Transplant Infectious Disease physicians about diagnosis and management of emerging fungal infections in solid organ transplant recipients.
• Castrejón-Pérez AD, Welsh EC, Miranda I, Ocampo-Candiani J, Welsh O. Cutaneous mucormycosis. An Bras Dermatol. 2017;92:304–11 Review summarizing clinical manifestations and diagnosis of cutaneous involvement in mucormycosis.
Kontoyiannis DP. Decrease in the number of reported cases of zygomycosis among patients with diabetes mellitus: a hypothesis. Clin Infect Dis. 2007;44:1089–90.
Pagano L, Caira M, Candoni A, Offidani M, Fianchi L, Martino B, et al. The epidemiology of fungal infections in patients with hematologic malignancies: the SEIFEM-2004 study. Haematologica. 2006;91:1068–75.
Pagano L, Offidani M, Fianchi L, Nosari A, Candoni A, Picardi M, et al. Mucormycosis in hematologic patients. Haematologica. 2004;89:207–14.
•• Bays DJ, Thompson GR 3rd. Fungal infections of the stem cell transplant recipient and hematologic malignancy patients. Infect Dis Clin N Am. 2019;33:545–66 Updated clinical review of invasive fungal infections as seen in patients with hematological malignancies and hematopoietic transplant recipients.
Devauchelle P, Jeanne M, Fréalle E. Mucormycosis in Burn Patients. J Fungi (Basel). 2019;5:E25.
Warkentien T, Rodriguez C, Lloyd B, Wells J, Weintrob A, Dunne JR, et al. Infectious disease clinical research program trauma infectious disease outcomes study group. Invasive mold infections following combat-related injuries. Clin Infect Dis. 2012;55:1441–9.
Neblett-Fanfair R, Benedict K, Bos J, et al. Necrotizing cutaneous mucormycosis after a tornado in Joplin, Missouri, in 2011. N Engl J Med. 2012;367:2214–25.
•• Roden MM, Zaoutis TE, Buchanan WL, et al. Epidemiology and outcome of zygomycosis: a review of 929 reported cases. Clin Infect Dis. 2005;41:634–53 First comprehensive literature review describing epidemiology and outcomes in all reported cases of Mucormycosis since 1885.
Hata DJ, Buckwalter SP, Pritt BS, Roberts GD, Wengenack NL. Real-time PCR method for detection of Zygomycetes. J Clin Microbiol. 2008;46:2353–8.
Chamilos G, Lewis RE, Kontoyiannis DP. Delaying amphotericin B-based frontline therapy significantly increases mortality among patients with hematologic malignancy who have zygomycosis. Clin Infect Dis. 2008;47:503–9.
Marty FM, Ostrosky-Zeichner L, Cornely OA, Mullane KM, Perfect JR, Thompson GR 3rd, et al. Isavuconazole treatment for mucormycosis: a single-arm open-label trial and case-control analysis. Lancet Infect Dis. 2016;16:828–37.
Heath CH, Slavin MA, Sorrell TC, Handke R, Harun A, Phillips M, et al. Population-based surveillance for scedosporiosis in Australia: epidemiology, disease manifestations and emergence of Scedosporium aurantiacum infection. Clin Microbiol Infect. 2009;15:689–93.
•• Cortez KJ, Roilides E, Quiroz-Telles F, et al. Infections caused by Scedosporium spp. Clin Microbiol Rev. 2008;21:157–97 Comprehensive review of history, pathogenesis, clinical manifestations, and treatment of different types of invasiveScedosporiuminfections.
Rougeron A, Giraud S, Alastruey-Izquierdo A, Cano-Lira J, Rainer J, Mouhajir A, et al. Ecology of Scedosporium species: present knowledge and future research. Mycopathologia. 2018;183:185–200.
Neofytos D, Fishman J, Horn D, et al. Epidemiology and outcome of invasive fungal infections in solid organ transplant recipients. Transpl Infect Dis. 2010;12:220–9.
Lamaris GA, Chamilos G, Lewis RE, Safdar A, Raad II, Kontoyiannis DP. Scedosporium infection in a tertiary care cancer center: a review of 25 cases from 1989-2006. Clin Infect Dis. 2006;43:1580–4.
Husain S, Munoz P, Forrest G, Alexander BD, Somani J, Brennan K, et al. Infections due to Scedosporium apiospermum and Scedosporium prolificans in transplant recipients: clinical characteristics and impact of antifungal agent therapy on outcome. Clin Infect Dis. 2005;40:89–99.
Caston JJ, Linares MJ, Rivero A, Casal M, Torre-Cisneros J. Clinical differences between invasive pulmonary infection by Scedosporium apiospermum and invasive pulmonary aspergillosis. Mycoses. 2011;54:e468–73.
Marr KA, Carter RA, Crippa F, Wald A, Corey L. Epidemiology and outcome of mould infections in hematopoietic stem cell transplant recipients. Clin Infect Dis. 2002;34:909–17.
Miyamoto T, Sasaoka R, Kawaguchi M, Ishioka S, Inoue T, Yamada N, et al. Scedosporium apiospermum skin infection: a case report and review of the literature. J Am Acad Dermatol. 1998;39:498–500.
Uenotsuchi T, Moroi Y, Urabe K, Tsuji G, Koga T, Matsuda T, et al. Cutaneous Scedosporium apiospermum infection in an immunocompromised patient and a review of the literature. Acta Derm Venereol. 2005;85:156–9.
Bower CP, Oxley JD, Campbell CK, Archer CB. Cutaneous Scedosporium apiospermum infection in an immunocompromised patient. J Clin Pathol. 1999;52:846–8.
Bosma F, Voss A, van Hamersvelt HW, de Sévaux RGL, Biert J, Kullberg BJ, et al. Two cases of subcutaneous Scedosporium apiospermum infection treated with voriconazole. Clin Microbiol Infect. 2003;9:750–3.
Gillum PS, Gurswami A, Taira JW. Localized cutaneous infection by Scedosporium prolificans (inflatum). Int J Dermatol. 1997;36:297–9.
Rüchel R, Margraf S. Rapid microscopical diagnosis of deep-seated mycoses following maceration of fresh specimens and staining with optical brighteners. Mycoses. 1993;36:239–42.
Idigoras P, Garcia-Arenzana JM, Saenz JR, Pineiro L, Marin J. Isolation of Scedosporium prolificans from the air in the room of a patient with leukemia and disseminated infection with this fungus. Enferm Infecc Microbiol Clin. 2000;18:426–7.
Ruiz-Díez B, Martín-Díez F, Rodríguez-Tudela JL, Alvárez M, Martínez-Suárez JV. Use of random amplification of polymorphic DNA (RAPD) and PCR-fingerprinting for genotyping a Scedosporium prolificans (inflatum) outbreak in four leukemic patients. Curr Microbiol. 1997;35:186–90.
Sitterlé E, Giraud S, Leto J. Matrix-assisted laser desorption ionization-time of flight mass spectrometry for fast and accurate identification of Pseudallescheria/Scedosporium species. Clin Microbiol Infect. 2014;20:929–35.
• McCarthy MW, Katragkou A, Iosifidis E, Roilides E, Walsh TJ. Recent advances in the treatment of Scedosporiosis and Fusariosis. J Fungi (Basel). 2018;4:1–16 Summary of newer diagnostic techniques and updates in management including evidence for newer triazoles.
Rodriguez MM, Calvo E, Serena C, Marine M, Pastor FJ, Guarro J. Effects of double and triple combinations of antifungal drugs in a murine model of disseminated infection by Scedosporium prolificans. Antimicrob Agents Chemother. 2009;53:2153–5.
Meletiadis J, Mouton JW, Meis JF, Verweij PE. In vitro drug interaction modeling of combinations of azoles with terbinafine against clinical Scedosporium prolificans isolates. Antimicrob Agents Chemother. 2003;47:106–17.
Troke P, Aguirrebengoa K, Arteaga C, Ellis D, Heath CH, Lutsar I, et al. Treatment of scedosporiosis with voriconazole: clinical experience with 107 patients. Antimicrob Agents Chemother. 2008;52:1743–50.
Nelson PE, Dignani MC, Anaissie EJ. Taxonomy, biology, and clinical aspects of Fusarium species. Clin Microbiol Rev. 1994;7:479–504.
Elvers K, Leeming K, Moore C, Lappin-Scott H. Bacterial-fungal biofilms in flowing water photo-processing tanks. J Appl Microbiol. 1998;84:607–18.
• Kontoyiannis DP, Marr KA, Park BJ, et al. Prospective surveillance for invasive fungal infections in hematopoietic stem cell transplant recipients, 2001-2006: overview of the transplant-associated infection surveillance network (TRANSNET) database. Clin Infect Dis. 2010;50:1091–100 Large nationwide prospective surveillance study with epidemiological information about invasive fungal infections in hematopoietic transplant patients.
Nucci M, Marr KA, Queiroz-Telles F, Martins CA, Trabasso P, Costa S, et al. Fusarium infection in hematopoietic stem cell transplant recipients. Clin Infect Dis. 2004;38:1237–42.
Nucci M, Anaissie EJ, Queiroz-Telles F, Martins CA, Trabasso P, Solza C, et al. Outcome predictors of 84 patients with hematologic malignancies and Fusarium infection. Cancer. 2003;98:315–9.
•• Nucci M, Anaissie E. Cutaneous infection by Fusarium species in healthy and immunocompromised hosts: implications for diagnosis and management. Clin Infect Dis. 2002;35:909–20 Large study with 259 patients describing cutaneous involvement inFusarium, contrasting manifestations in immunocompetent and immunocompromised patients.
Bodey GP. Dermatologic manifestations of infections in neutropenic patients. Infect Dis Clin North Am. 1994;8:655–75.
Prins C, Chavaz P, Tamm K, Hauser C. Ecthyma grangrenosum-like lesions: a sign of disseminated Fusarium infection in the neutropenic patient. Clin Exp Dermatol. 1995;20:428–30.
Nucci M, Anaissie E. Fusarium infections in immunocompromised patients. Clin Microbiol Rev. 2007;20:695–704.
Ooi SP, Chen TT, Huang TH, Chang HS, Hsieh HY. Granuloma annulare-like skin lesion due to Fusarium roseum: therapy with ketoconazole [letter]. Arch Dermatol. 1987;123:167–8.
Benjamin RP, Callaway L, Conant NF. Facial granuloma associated with Fusarium infection. Arch Dermatol. 1970;101:598–600.
Girardi M, Glusac EJ, Imaeda S. Subcutaneous Fusarium foot abscess in a renal transplant patient. Cutis. 1999;63:267–70.
English MP. Invasion of the skin by filamentous non-dermatophyte fungi. Br J Dermatol. 1968;80:282–6.
Hennequin C, Ranaivoarimalala C, Chouaki T, Tazerout M, Ancelle T, Cabaud JJ, et al. Comparison of aerobic standard medium with specific fungal medium for detecting Fusarium spp in blood cultures. Eur J Clin Microbiol Infect Dis. 2002;21:748–50.
Bushelman SJ, Callen JP, Roth DN, Cohen LM. Disseminated Fusarium solani infection. J Am Acad Dermatol. 1995;32:346–51.
Odabasi Z, Mattiuzzi G, Estey E, Kantarjian H, Saeki F, Ridge RJ, et al. β-D-glucan as a diagnostic adjunct for invasive fungal infections: validation, cutoff development, and performance in patients with acute myelogenous leukemia and myelodysplastic syndrome. Clin Infect Dis. 2004;39:199–205.
Hue FX, Huerre M, Rouffault MA, de Bievre C. Specific detection of Fusarium species in blood and tissues by a PCR technique. J Clin Microbiol. 1999;37:2434–8.
• Cuenca-Estrella M, Gomez-Lopez A, Mellado E, Buitrago MJ, Monzon A, Rodriguez-Tudela JL. Head-to-head comparison of the activities of currently available antifungal agents against 3,378 Spanish clinical isolates of yeasts and filamentous fungi. Antimicrob Agents Chemother. 2006;50:917–21 Results of susceptibility testing for antifungals including triazoles providing useful clinical data for frequently multidrug-resistant filamentous fungi includingFusarium, Scedosporium, andScopulariopsisamong others.
Lortholary O, Obenga G, Biswas P, Caillot D, Chachaty E, Bienvenu AL, et al. International retrospective analysis of 73 cases of invasive fusariosis treated with voriconazole. Antimicrob Agents Chemother. 2010;54:4446–50.
Raad II, Hachem RY, Herbrecht R, Graybill JR, Hare R, Corcoran G, et al. Posaconazole as salvage treatment for invasive fusariosis in patients with underlying hematologic malignancy and other conditions. Clin Infect Dis. 2006;42:1398–403.
Cornely OA, Ostrosky-Zeichner L, Rahav G, et al. Outcomes in patients with invasive mold disease caused by Fusarium or Scedosporium spp treated with isavuconazole: experience from the VITAL and SECURE trials. (Abstract M-1760). In: Program and abstracts of the 54th Interscience Conference on Antimicrobial Agents and Chemotherapy. Washington, DC; 2014.
Perfect JR. Treatment of non-Aspergillus moulds in immunocompromised patients, with amphotericin B lipid complex. Clin Infect Dis. 2005;40:S401–S8.
Córdoba S, Rodero L, Vivot W, Abrantes R, Davel G, Vitale RG. In vitro interactions of antifungal agents against clinical isolates of Fusarium spp. Int J Antimicrob Agents. 2008;31:171–4.
Ortoneda M, Capilla J, Javier Pastor F, Pujol I, Guarro J. In vitro interactions of licensed and novel antifungal drugs against Fusarium spp. Diagn Microbiol Infect Dis. 2004;48:69–71.
De Hoog GS, Guarro J, Gené J, Figueras MJ. Atlas of clinical fungi. 2nd ed. Baarn: Centraalbureau Voor Schimmelcultures; 2000. p. 794–809.
• Pastor FJ, Guarro J. Clinical manifestations, treatment, and outcome of Paecilomyces lilacinus infections. Clin Microbiol Infect. 2006;12:948–60 Comprehensive literature review of 119 cases ofPaecilomyces lilanicusincluding clinical presentations and review of treatment for this frequently multidrug resistant fungus.
Itin PH, Frei R, Lautenschlager S, et al. Cutaneous manifestations of Paecilomyces lilacinus infection induced by a contaminated skin lotion in patients who are severely immunosuppressed. J Am Acad Dermatol. 1998;39:401–9.
Jade KB, Lyons MF, Gnann JW. Paecilomyces lilacinus cellulitis in an immunocompromised patient. Arch Dermatol. 1986;122:1169–70.
Summerbell R. Ascomycetes, Aspergillus, Fusarium, Sporothrix, Piedraia, and their relatives. In: Howard DH, editor. Pathogenic fungi in humans and animals. 2nd ed. New York: Dekker; 2003. p. 237–498.
Liu K, Howell DN, Perfect JR, Schell WA. Morphologic criteria for the preliminary identification of Fusarium, Paecilomyces, and Acremonium species by histopathology. Am J Clin Pathol. 1998;109:45–54.
Aguilar C, Pujol I, Sala J, Guarro J. Antifungal susceptibilities of Paecilomyces species. Antimicrob Agents Chemother. 1998;42:1601–4.
Espinel-Ingroff A, Chaturvedi V, Fothergill A, Rinaldi MG. Optimal testing conditions for determining MICs and minimum fungicidal concentrations of new and established antifungal agents for uncommon moulds: NCCLS collaborative study. J Clin Microbiol. 2002;40:3776–81.
Feldman R, Cockerham L, Buchan BW, Lu Z, Huang AM. Treatment of Paecilomyces variotii pneumonia with posaconazole: case report and literature review. Mycoses. 2016;59:746–50.
Yehia M, Thomas M, Pilmore H, et al. Subcutaneous black fungus (phaeohyphomycosis) infection in renal transplant recipients: three cases. Transplantation. 2004;15:140–2.
Revankar SG, Sutton DA. Melanized fungi in human disease. Clin Microbiol Rev. 2010;23:884–928.
Caviedes MP, Torre AC, Eliceche ML, Valdivia Monteros DC, Volonteri VI, Galimberti RL. Cutaneous phaeohyphomycosis. Int J Dermatol. 2017;56:415–20.
• McCarty TP, Baddley JW, Walsh TJ, et al. Phaeohyphomycosis in transplant recipients: results from the transplant associated infection surveillance network (TRANSNET). Med Mycol. 2015;53:440–6 Review of 56 clinical cases in literature including both solid organ transplants and hematopoietic cell transplants providing useful information about cutaneous presentations and antifungal treatment used in clinical cases.
Shoham S, Marr KA. Invasive fungal infections in solid organ transplant recipients. Future Microbiol. 2012;7:639–55.
Boyce RD, Deziel PJ, Otley CC, Wilhelm MP, Eid AJ, Wengenack NL, et al. Phaeohyphomycosis due to Alternaria species in transplant recipients. Transpl Infect Dis. 2010;12:242–50.
Ben-Ami R, Lewis RE, Raad II, Kontoyiannis DP. Phaeohyphomycosis in a tertiary care cancer center. Clin Infect Dis. 2009;48:1033–41.
Essabbah N, Gorsane I, Youssef M, Hadhri R, Aloui S, Gorcii M, et al. Cutaneous alternariosis in a renal transplant recipient. Cutis. 2014;93:237–40.
Cunhaa D, Amaroa C, Vieiraa MR, et al. Phaeohyphomycosis caused by Alternaria infectoria presenting as multiple vegetating lesions in a renal transplant patient. Rev Iberoam Micol. 2012;29:44–6.
Rinaldi MG. Phaeohyphomycosis. Dermatol Clin. 1996;14:147–53.
Cuétara MS, Alhambra A, Moragues MD, et al. Detection of (1-->3)-beta-D-glucan as an adjunct to diagnosis in a mixed population with uncommon proven invasive fungal diseases or with an unusual clinical presentation. Clin Vaccine Immunol. 2009;16:423–6.
Hsu C, Chang S, Lee P, et al. Cutaneous alternariosis in a renal transplant recipient: a case report and literature review. Asian J Surg. 2015;38:47–57.
Revankar SG, Baddley JW, Chen SC, et al. A mycoses study group international prospective study of phaeohyphomycosis: an analysis of 99 proven/probable cases. Open Forum Infect Dis. 2017;4(4):ofx200.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Fungal Infections of Skin and Subcutaneous Tissue
Rights and permissions
About this article
Cite this article
Chandorkar, A., Simkins, J. Emerging Fungal Cutaneous Infections in Immunocompromised Patients. Curr Fungal Infect Rep 14, 217–224 (2020). https://doi.org/10.1007/s12281-020-00395-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12281-020-00395-2