Abstract
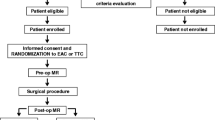
The role of aortic clamping techniques on the occurrence of neurological complications after right mini-thoracotomy mitral valve surgery is still debated. Brain injuries can occur also as silent cerebral micro-embolizations (SCM), which have been linked to significant deficits in physical and cognitive functions. Aims of this study are to evaluate the overall rate of SCM and to compare endoaortic clamp (EAC) with trans-thoracic clamp (TTC). Patients enrolled underwent a pre-operative, a post-operative, and a follow-up MRI. Forty-three patients were enrolled; EAC was adopted in 21 patients, TTC in 22 patients. Post-operative SCM were reported in 12 cases (27.9%). No differences between the 2 groups were highlighted (23.8% SCM in the EAC group versus 31.8% in the TTC). MRI analysis showed post-operative SCM in nearly 30% of selected patients after right mini-thoracotomy mitral valve surgery. Subgroup analysis on different types of aortic clamping showed comparable results.
Clinical Relevance
The rate of SCM reported in the present study on patients undergoing minimally invasive MVS and RAP is consistent with data in the literature on patients undergoing cardiac surgery through median sternotomy and antegrade arterial perfusion. Moreover, no differences were reported between EAC and TTC: both the aortic clamping techniques are safe, and the choice of the surgical setting to adopt can be really done according to the patient’s characteristics.

Similar content being viewed by others
Abbreviations
- SCM:
-
Silent cerebral micro-embolizations
- MVS:
-
Mitral valve surgery
- RAP:
-
Retrograde arterial perfusion
- EAC:
-
Endoaortic clamp
- TTC:
-
Trans-thoracic clamp
- MRI:
-
Magnetic resonance imaging
- 3 T:
-
3 Tesla
- DWI:
-
Diffusion-weighted imaging
- DTI:
-
Diffusion tensor imaging
References
Newman, M. F., Grocott, H. P., Mathew, J. P., et al. (2001). Report of the substudy assessing the impact of neurocognitive function on quality of life 5 years after cardiac surgery. Stroke, 32, 2874–2881.
Newman, M. F., Mathew, J. P., Grocott, H. P., et al. (2006). Central nervous system injury associated with cardiac surgery. Lancet, 368, 694–703.
Taggart, D. P., & Westaby, S. (2001). Neurological and cognitive disorders after coronary artery bypass grafting. Current Opinion in Cardiology, 16, 271–276.
Taggart, D. P., Browne, S. M., Wade, D. T., & Halligan, P. W. (2003). Neuroprotection during cardiac surgery: A randomised trial of a platelet activating factor antagonist. Heart, 89, 897–900.
Fearn, S. J., Pole, R., Burgess, S. G., Ray, T. L., Hooper, C. N., & McCollum, C. N. (2001). Cerebral embolization during modern cardiopulmonary bypass. European Journal of Cardio-Thoracic Surgery, 20, 1163–1167.
Gammie, J. S., Sheng, S., Griffith, B. P., et al. (2009). Trends in mitral valve surgery in the United States: Results from the Society of Thoracic Surgeons Adult Cardiac Database. Annals of Thoracic Surgery, 87, 1431–1439.
Selnes, O. A., Goldsborough, M. A., Borowicz, L. M., & McKhann, G. M. (1999). Neurobehavioural sequelae of cardiopulmonary bypass. Lancet, 353, 1601–1606.
Stolz, E., Gerriets, T., Kluge, A., Klovekorn, W. P., Kaps, M., & Bachmann, G. (2004). Diffusion-weighted magnetic resonance imaging and neurobiochemical markers after aortic valve replacement: Implications for future neuroprotective trials? Stroke, 35, 888–892.
Indja, B., Woldendorp, K., Vallely, M. P., & Grieve, S. M. (2019). Silent brain infarcts following cardiac procedures: A systematic review and meta-analysis. J Am Heart Assoc, 8, e010920.
Vermeer, S. E., Hollander, M., van Dijk, E. J., et al. (2003). Silent brain infarcts and white matter lesions increase stroke risk in the general population: The Rotterdam Scan Study. Stroke, 34, 1126–1129.
Barbero, C., Marchetto, G., Ricci, D., et al. (2016). Minimal access mitral valve surgery: Impact of tailored strategies on early outcome. Annals of Thoracic Surgery, 102, 1989–1994.
Casselman, F., Aramendi, J., Bentala, M., et al. (2015). Endoaortic clamping does not increase the risk of stroke in minimal access mitral valve surgery: A multicenter experience. Annals of Thoracic Surgery, 100, 1334–1339.
Barbero, C., Krakor, R., Bentala, M., et al. (2018). Comparison of endoaortic and trans-thoracic aortic clamping in less-invasive mitral valve surgery. Annals of Thoracic Surgery, 105, 794–798.
Barbero, C., Marchetto, G., Ricci, D., & Rinaldi, M. (2017). Temporary neurological dysfunction after minimal invasive mitral valve surgery: Influence of type of perfusion and aortic clamping technique. Annals of Thoracic Surgery, 103(2), 691–692.
Grossi, E. A., Loulmet, D. F., Schwartz, C. F., et al. (2011). Minimally invasive valve surgery with antegrade perfusion strategy is not associated with increased neurologic complications. Annals of Thoracic Surgery, 92, 1346–1350.
Ghoreishi, M., Thourani, V. H., Badhwar, V., et al. (2021). Less-invasive aortic valve replacement: Trends and outcomes from the Society of Thoracic Surgeons database. Annals of Thoracic Surgery, 111, 1216–1224.
Je, H. G., Min, H. J., Chee-Hoon, L., et al. (2019). Incidence and distribution of cerebral embolism after cardiac surgery according to the systemic perfusion strategy-A diffusion-weighted magnetic resonance imaging study. Circulation J, 84, 54–60.
Barbero, C., Ricci, D., El Qarra, S., Marchetto, G., Boffini, M., & Rinaldi, M. (2015). Aortic cannulation system for minimally invasive mitral valve surgery. Journal of Thoracic and Cardiovascular Surgery, 149, 1669–1672.
Gammie, J. S., Zhao, Y., Peterson, E. D., et al. (2010). Less-invasive mitral valve operations: Trends and outcomes from the society of thoracic surgeons adult cardiac surgery database. Annals of Thoracic Surgery, 90, 1401–1410.
Grant, S. W., Hickey, G. L., Modi, P., et al. (2019). Propensity-matched analysis of minimally invasive approach versus sternotomy for mitral valve surgery. Heart, 105, 783–789.
Paparella, D., Fattouch, K., Moscarelli, M., et al. (2020). Current trends in mitral valve surgery: A multicenter national comparison between full-sternotomy and minimally-invasive approach. International Journal of Cardiology, 306, 147–151.
Mazine, A., Pellerin, M., Lebon, J. S., Dionne, P. O., Jeanmart, H., & Bouchard, D. (2013). Minimally invasive mitral valve surgery: Influence of aortic clamping technique on early outcomes. Annals of Thoracic Surgery, 96(6), 2116–2122.
Nishimura, R. A., Otto, C. M., Bonow, R. O., Carabello, B. A., et al. (2017). 2017 AHA/ACC focused update of the 2014 AHA/ACC guideline for the management of patients with valvular heart disease: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation, 135, 1159–1195.
Nakamura, H., Yamada, K., Kizu, O., et al. (2005). Effect of thin-section diffusion-weighted MR imaging on stroke diagnosis. AJNR. American Journal of Neuroradiology, 26, 560–565.
Mullins, M. E., Schaefer, P. W., Sorensen, A. G., et al. (2002). CT and conventional and diffusion-weighted MR imaging in acute stroke: Study in 691 patients at presentation to the emergency department. Radiology, 224, 353–360.
Ozsunar, Y., & Sorensen, A. G. (2000). Diffusion- and perfusion-weighted magnetic resonance imaging in human acute ischemic stroke: Technical considerations. Topics in Magnetic Resonance Imaging, 11, 259–272.
Barbero, C., Ricci, D., Cura Stura, E., et al. (2017). Magnetic resonance imaging for cerebral lesions during minimal invasive mitral valve surgery: Study protocol for a randomized controlled trial. Trials, 17, 76.
Barbero, C., Marchetto, G., Ricci, D., et al. (2019). Steps forward in minimal invasive cardiac surgery: 10-year experience. Annals of Thoracic Surgery, 108(6), 1822–1829.
Falk, V., Cheng, D. C., Martin, J., et al. (2011). Minimally invasive versus open mitral valve surgery: A consensus statement of the International Society of Minimally Invasive Coronary Surgery (ISMICS) 2010. Innovations (Phila), 6(2), 66–76.
Knipp, S. C., Matatko, N., Schlamann, M., et al. (2005). Small ischemic brain lesions after cardiac valve replacement detected by diffusion-weighted magnetic resonance imaging: Relation to neurocognitive function. European Journal of Cardio-Thoracic Surgery, 28, 88–96.
Barber, P. A., Hach, S., Tippett, L. J., Ross, L., Merry, A. F., & Milsom, P. (2008). Cerebral ischemic lesions on diffusion-weighted imaging are associated with neurocognitive decline after cardiac surgery. Stroke, 39, 1427–1433.
Fiebach, J. B., Schellinger, P. D., Jansen, O., et al. (2002). CT and diffusion-weighted MR imaging in randomized order: Diffusion-weighted imaging results in higher accuracy and lower interrater variability in the diagnosis of hyperacute ischemic stroke. Stroke, 33, 2206–2210.
Lansberg, M. G., Albers, G. W., Beaulieu, C., & Marks, M. P. (2000). Comparison of diffusion-weighted MRI and CT in acute stroke. Neurology, 54, 1557–1561.
Floyd, T. F., Shah, P. N., Price, C. C., et al. (2006). Clinically silent cerebral ischemic events after cardiac surgery: Their incidence, regional vascular occurrence, and procedural dependence. Annals of Thoracic Surgery, 81, 2160–2166.
Blazek, S., Lurz, P., Mangner, N., et al. (2015). Incidence, characteristics and functional implications of cerebral embolic lesions after the MitraClip procedure. EuroIntervention, 10, 1195–1203.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
The study protocol was reviewed and approved by the Institutional Ethics Committee (protocol 0063123).
Conflict of Interest
The authors declare no competing interests.
Additional information
Associate Editor Angela Taylor oversaw the review of this article
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Barbero, C., Rinaldi, M., Marchetto, G. et al. Magnetic Resonance Imaging for Cerebral Micro-embolizations During Minimally Invasive Mitral Valve Surgery. J. of Cardiovasc. Trans. Res. 15, 828–833 (2022). https://doi.org/10.1007/s12265-021-10188-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12265-021-10188-8