Abstract
Thorax computed tomography in patients with thoracic trauma is undeniably a highly beneficial method. However, it also has disadvantages such as difficulties in transferring critical patients to computed tomography, delays in diagnosis, the risk of radiation exposure, and higher costs. On the other hand, ultrasonography can be rapidly performed at the bedside and is a non-invasive technique that poses no risk of radiation exposure. These advantages make it a valuable method in the early diagnosis of thoracic trauma. Therefore, this study aimed to provide insights into the sensitivity and accuracy of bedside ultrasonography in diagnosing pneumothorax in patients presenting with thorax trauma in an emergency department. The study sample comprised 132 patients over 18 years of age who were transferred with thorax trauma to the Emergency Clinic of Bakırköy Dr. Sadi Konuk Training and Research Hospital between January 30, 2015, and June 30, 2015. Ultrasonographic examinations were performed before thoracic computed tomography in all patients for whom a thorax computed tomography was indicated based on the clinical examination by the emergency room physician. The thoracic computed tomography reports, interpreted by a radiologist who was blinded to the ultrasonographic and clinical findings of the patients, were accepted as the gold standard. All 132 patients included in the study underwent Thorax ultrasonography. The average age of the patients was 76.5%, with the youngest patient being 18 years old and the oldest one being 90 years old. Of the patients, 45.38% (n = 101) were men. The results of Thorax ultrasonography showed that 19 patients had pneumothorax. These findings were then compared with the Thorax computed tomography results accepted as the gold standard. The results revealed that Thorax ultrasonography had a sensitivity of 56.2% and a specificity of 99% in detecting pneumothorax. According to the grading on CT, our observation revealed that the sensitivity of ultrasonography to detect pneumothorax increased proportionally with the severity of pneumothorax detected on thoracic computed tomography. The sensitivity of ultrasonography in patients with a grade 2 pneumothorax and those with a grade 3 pneumothorax, according to Thorax computed tomography, was found to be 70% and 100%, respectively. Thorax ultrasonography is a useful technique with high specificity in diagnosing pneumothorax, but its sensitivity decreases significantly when the size is below 1 cm.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Trauma is one of the leading causes of death during the first four decades of life, with thorax trauma accounting for 20 to 25% of these fatalities [1, 2]. Thorax traumas can result in injuries to vital organs, necessitating prompt treatment and the rapid restoration of cardiorespiratory function [3, 4]. Among the intrathoracic pathologies commonly observed in cases of thorax trauma are pneumothorax, hemothorax, and hemopneumothorax [5, 6]. The gold standard radiological method for diagnosing pneumothorax is thorax computerized tomography (CT) [7,8,9]. Thorax CT in patients with thoracic trauma is undoubtedly a highly beneficial method. However, it also has disadvantages such as difficulties in transferring critical patients to CT, delays in diagnosis, risk of radiation exposure, and higher costs [10, 11]. On the other hand, ultrasonography (USG) can be rapidly performed at the bedside and is a non-invasive technique that carries no risk of radiation exposure. These advantages make it a valuable method for early evaluation [12].
Bedside diagnosis of pneumothorax in patients with thorax trauma using USG is important for initiating early treatment. USG examination of the thorax in trauma cases has emerged as a promising technique for detecting pneumothorax. Research has been published that have shown that USG is also more sensitive than posteroanterior chest radiography in detecting pneumothoraces of small size that can easily go unnoticed (hidden cases) [13]. In another series of studies, USG has been validated as a reliable technique through comparison with thorax CT [14]. The objective of this study was to provide insights into the sensitivity and accuracy of bedside USG in diagnosing pneumothorax in patients presenting with thorax trauma in an emergency department.
Patients and Methods
Study Design
The study was conducted in a prospective design at the Emergency Clinic of Bakırköy Dr. Sadi Konuk Training and Research Hospital. Prior to commencing the study, ethical clearance was obtained from the Ethics Board of Bakırköy Dr. Sadi Konuk Training and Research Hospital (consent obtained on 26.01.2015 with reference number 2015/02/01 and protocol number 2015–09). The study sample comprised 132 patients over 18 years of age who were transferred to the Emergency Clinic of Bakırköy Dr. Sadi Konuk Training and Research Hospital between 30 January 2015 and 30 June 2015 due to thorax trauma and underwent thorax CT. The inclusion and exclusion criteria for the study were as follows:
Criteria of Inclusion in the Study
-
Patients with thorax trauma
Patients who underwent Thorax CT
Patients over 18 years of age
Those who agreed to participate in the study
Criteria of Exclusion from the Study
-
Patients with an indication for an emergency intervention
Patients who could not be examined through USG due to the absence of USG physician
Study Population
In the study, 132 patients over 18 years of age who had presented with thorax trauma to the Emergency Clinic of Bakırköy Dr. Sadi Konuk Training and Research Hospital between January 30, 2015, and June 30, 2015, were included. These patients had been recorded in the Medin® system, which is the information processing system used by the hospital's data processing unit.
A total of 124,598 patients presented to our Emergency Clinic during the study period. Among these patients, 9,777 had trauma, and 1,070 of them had thorax trauma. Out of the 1,070 patients, 184 who were under 18 years of age were excluded from the study. Additionally, 135 patients who did not agree to participate, 3 patients with unstable conditions, and 616 patients who did not undergo USG due to the unavailability of a USG physician at the time of transfer were also excluded. As a result, the final sample consisted of 132 patients with thorax trauma who met the inclusion criteria (Fig. 1).
Measurement Methods
To ensure standardization in the study, the physician who performed the USG examination received training in "Basic and Advanced Ultrasonography" organized by "The Association of Emergency Medicine of Turkey." The patients included in the study underwent Thorax USG using a 10 MHz superficial probe and a 3 S Sector probe of 3.5–5 MHz from an ultrasonography device of the Vivid e model, manufactured by General Electric. The examinations were conducted following the Lichtenstein BLUE (Bedside Lung Ultrasound in Emergency) protocol [15]. Each hemithorax was examined at three points. All USG examinations were performed before Thorax CT scans to blind the physicians conducting the USG. The trauma mechanism, vital findings of patients, physical examination findings, USG findings, and Thorax CT results, as reported by an independent radiology physician, were all recorded.
All patients included in the study underwent Thorax CT scanning, and the results were subsequently compared with those observed in USG imaging. Thorax CT scans, interpreted by radiology physicians who were unaware of the study, were considered the gold standard. The severity of pneumothorax in patients diagnosed with pneumothorax on Thorax CT was classified using the Uz et al. grading system, which was based on the classification proposed by Wolfman et al. [16, 17] (Table 1). The grading was based on Thorax CT scans taken in slices with a thickness of 10 mm.
Data Analysis
Software called "Statistical Package for Social Sciences for Windows 16.0" was used to record the data that were acquired for the study. In a previous study, the sensitivity of ultrasonography in detecting pneumothorax was found to be 92%, while the specificity was 99.4%. The estimated prevalence of the disease was 23% [18]. Using these figures, the minimum sample size required for our study, with a 95% confidence interval and 10% precision, was determined to be 123 patients.Based on the measurements, continuous variables were estimated as mean standard deviation (SD). The related likelihood ratios were used to assess the sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) for both USG and Thorax CT. The mean and standard deviation (SD) for continuous variables and the numbers and percentages (%) for qualitative variables were used to report patient data. The means of two groups with a normal distribution of categorical data were compared using independent t-tests. To compare categorical variables with nominal values, chi-squared tests were used. The Mann–Whitney U test was employed to compare the differences between two variables for small groups or those with non-normal distributions. The significance level for the statistical tests was set at p 0.05, and a 95% confidence interval was employed.
Results
Demographic and Clinical Information Regarding Patients
The average age of the patients, of whom 101 (76.5%) were men and 31 (23.5%) were women, was 45.38 SD19.12 years. The youngest patient in the study was 18 years old, while the oldest patient was 90 years old. The vital signs of the 132 patients were recorded as follows: the average systolic blood pressure was 124.41 SD20.66 mmHg (with a minimum of 71 and a maximum of 220), the average diastolic blood pressure was 72.21 SD11.36 mmHg (with a minimum of 40 and a maximum of 120), the average pulse rate was 87.88 SD16.07 beats per minute (with a minimum of 56 and a maximum of 155), and the average oxygen saturation level was 97.24 SD3.10% (with a minimum of 80 and a maximum of 100).
The etiological examination of the cases revealed that the highest rate among the causes was attributed to simple falls, with 42 patients (31.8%). This was followed by traffic accidents with injuries occurring inside the vehicles involved, accounting for 20 patients (15.2%). Falls from a higher place accounted for 15 patients (11.4%), while traffic accidents with injuries occurring outside the vehicles involved accounted for 11 patients (8.3%). Other causes included sharp object injuries (9 patients, 6.8%), assaults (9 patients, 6.8%), falls down stairs (9 patients, 6.8%), motorcycle accidents (5 patients, 3.8%), crush injuries (5 patients, 3.8%), contact with a hard object (4 patients, 3%), gunshot injuries (2 patients, 1.5%), and iatrogenic injuries (1 patient, 0.8%).
The thorax examination of 132 patients by USG revealed that 12 patients (9.1%) had an open wound, with 7 in the right hemithorax and 5 in the left hemithorax. Additionally, 8 patients (6%) had ecchymosis, with 6 in the right hemithorax and 2 in the left hemithorax. Dermabrasion was detected in 7 patients (5.3%), with 4 in the right hemithorax and 3 in the left hemithorax. Furthermore, 1 patient (0.8%) was found to have traumatic flail chest, specifically in the left hemithorax. There were 16 patients (12.1%) who exhibited decreased sounds in auscultation in one of the hemithoraces compared to the other. Among these patients, 12 had decreased sounds in the right hemithorax, while 4 had decreased sounds in the left hemithorax (Table 2).
Ultrasonography Findings
All 132 patients were subjected to USG imaging without exception to investigate whether they had pneumothorax. The USG examination focused on detecting pneumothorax by assessing the movement of the pleural shift, B line, seashore sign, lung pulse, A line, barcode finding, and lung point. The USG results revealed that 19 patients (14.4%) had pneumothorax, with 11 patients in the right hemithorax and 8 patients in the left hemithorax. These USG findings were compared with the Thorax CT results, which were accepted as the gold standard. The Thorax CT scans were interpreted by radiology physicians who were unaware of the study (Table 3).
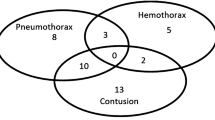
Thorax CT results indicated that out of the 132 patients, 32 (24.2%) had pneumothorax, with 16 in the right hemithorax, 13 in the left hemithorax, and 3 bilateral cases. Additionally, 20 patients (15.2%) had hemothorax, with 11 in the right hemithorax, 8 in the left hemithorax, and 1 bilateral case. Lung contusion was observed in 25 patients (18.9%), with 17 in the right hemithorax and 8 in the left hemithorax. Hemopneumothorax was detected in 13 patients. In the right hemithorax, 113 patients (85.6%) had grade 0 pneumothorax, 5 patients (3.8%) had grade 1 pneumothorax, 13 patients (9.8%) had grade 2 pneumothorax, and 1 patient (0.8%) had grade 3 pneumothorax. In the left hemithorax, 116 patients (87.9%) had grade 0 pneumothorax, 7 patients (5.3%) had grade 1 pneumothorax, 8 patients (6.1%) had grade 2 pneumothorax, and 1 patient (0.8%) had grade 3 pneumothorax. None of the 132 patients had a shift or total pneumothorax.
From the USG findings of pneumothorax, various indicators such as the absence of pleural shift, absence of B line, absence of seashore sign, absence of pulmonary pulse sign, absence of A line, barcode finding, and lung point finding were evaluated separately. The sensitivity of the lung point finding was significantly lower compared to the sensitivity of the other findings. However, there was no significant difference observed in the specificity of these findings (Table 4). Among the 19 patients in whom pneumothorax was detected in their USG examination, 18 patients (94.7%) also had pneumothorax detected in their Thorax CT. However, 1 patient (5.3%) did not show pneumothorax in the Thorax CT. On the other hand, out of the 113 patients in whom no pneumothorax was detected in the USG examination, 14 patients (12.4%) were found to have pneumothorax in the Thorax CT, while 99 patients (87.6%) did not have pneumothorax in the Thorax CT. The sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of USG in detecting pneumothorax were calculated as 56.2%, 99%, 94.7%, and 87.6% respectively (Table 4).
In evaluating pneumothorax, the findings of the USG examination were compared with the pneumothorax grading in Thorax CT. The recorded pneumothorax grades in patients where pneumothorax was detected by USG were as follows: grade 0 in 1 patient (5.3%), grade 1 in 2 patients (10.5%), grade 2 in 14 patients (73.7%), and grade 3 in 2 patients (10.5%). None of the patients had grade 4 pneumothorax. Among the patients where no pneumothorax was detected by USG, the pneumothorax grades were as follows: grade 0 in 99 patients (87.6%), grade 1 in 8 patients (7.1%), and grade 2 in 6 patients (5.3%). Grades 3 and 4 were not detected in any of the patients. The specificity and negative predictive value (NPD) of USG in detecting pneumothorax were found to be 99% and 87.6% respectively. However, when considering specific pneumothorax grades, the specificity was 20% and NPD was 10.5% for detecting grade 1 pneumothorax, 70% and 73.7% for detecting grade 2 pneumothorax, and 100% and 10.5% for detecting grade 3 pneumothorax, respectively (Table 5).
While tube thoracostomy was performed on 10 (52.6%) of the 19 patients in whom pneumothorax was detected by USG, no tube thoracostomy was performed on the remaining 9 patients (47.4%). On the other hand, tube thoracostomy was performed on 2 (1.8%) of the 113 patients in whom no pneumothorax was detected by USG, while no thoracostomy was performed on the remaining 111 patients (98.2%).
Discussion
Our study has demonstrated that Thorax ultrasonography (USG) is an effective method with a high level of specificity for diagnosing pneumothorax. Additionally, the findings of our study indicate that USG exhibits a high level of sensitivity in detecting pneumothoraces with a width greater than 1 cm, as confirmed by Thorax CT.
Pneumothorax, hemothorax, and hemopneumothorax are the most commonly observed pathologies following thorax trauma, with some studies reporting a pneumothorax incidence of over 35% [19]. Even though Thorax CT has been acknowledged as the gold standard in the diagnosis of thorax pathologies [7,8,9], USG has emerged as a useful technique due to its radiation-free nature and ability to be rapidly performed at the bedside in the early period [12]. Bedside USG can be easily performed by clinicians, but the accuracy of USG in diagnosing pneumothorax largely depends on the operators' ability [20, 21].
In a study involving 109 patients with thorax trauma and multiple injuries, researchers reported a pneumothorax rate of 23%. Among the cases, 60% were located on the left side, 32% on the right side, and 8% were bilateral [18]. In our study with 132 patients, we found that 24.2% of the patients with thorax trauma had pneumothorax, with 50% occurring on the right side, 40.6% on the left side, and 9.4% bilateral.
Previous research has reported that the sensitivity of Thorax USG in detecting pneumothorax ranges between 92% and 98.1%, its specificity between 97.2% and 99.2%, its PPD between 89.3% and 98.1%, and its NPD between 96.3% and 99.2% [18, 22, 23]. Our study found the following values regarding the effectiveness of Thorax USG in detecting pneumothorax: sensitivity 56.2%, specificity 99%, PPD 94.7%, and NPD 87.6%. Among the patients diagnosed with pneumothorax by Thorax CT in our study, 31.25% had grade 1 pneumothorax. We observed lower sensitivity in diagnosing pneumothorax with Thorax USG in our study, as it is difficult to detect grade 1 pneumothorax with USG. Eventually, while the sensitivity in patients with grade 2 pneumothorax rose to 70%, it reached 100% in patients with grade 3 pneumothorax.In a study examining patients with trauma, researchers found that Extended Emergency Trauma Ultrasonography (EETU) failed to detect grade 1 pneumothoraces that were smaller than 1 cm in width or did not exceed the micro-coronal line in five out of eight patients. The USG sensitivity for a pneumothorax case of this grade was found to be 37.5% [16]. In our study, grade 1 pneumothoraces also went unnoticed in eight out of ten patients, resulting in a sensitivity of 20% for this grade. As some pneumothoraces were located next to the diaphragm or mediastinum, they could not be detected by USG. In another case, a patient who had been diagnosed with pneumothorax by USG was later reported to have no pneumothorax when examined by Thorax CT. It is suggested that this failure may have resulted from the movement of the pleural surfaces, which probably went unnoticed due to the shallow breathing of the patient. The specificity, PPD, and NPD values found in our study regarding the effectiveness of USG in detecting pneumothorax, on the other hand, were consistent with values observed in previous research.
The USG sensitivity for pneumothoraces in the right hemithorax was higher compared to those occurring in the left hemithorax. This difference can be attributed to the fact that advanced pneumothoraces tend to occur randomly in the right hemithorax in most cases. Additionally, a higher incidence of grade 1 pneumothoraces in the left hemithorax resulted in a lower sensitivity range in our findings.
One important limitation of our study is the lack of specific measures to address bias in both patient recruitment and statistical analysis. While we aimed to minimize bias through careful patient selection criteria, the study was conducted at a single healthcare facility, which may introduce selection bias. The Emergency Clinic of Bakırköy Dr. Sadi Konuk Training and Research Hospital may serve as a tertiary referral center, leading to the inclusion of patients with more severe cases or specific characteristics. As a result, the generalizability of our findings to other healthcare settings or patient populations may be limited.
Conclusion
Our study aimed to investigate the diagnostic effectiveness of bedside ultrasonography performed by emergency unit physicians on patients over 18 years of age with thorax trauma. The results of our study have shown that Thorax ultrasonography is a useful technique that offers high specificity in diagnosing pneumothorax. Additionally, the study findings have demonstrated that ultrasonography is highly sensitive in detecting pneumothoraces with a width over 1 cm, as confirmed by Thorax computed tomography. The sensitivity for grade 2 pneumothoraces in Thorax computed tomography is 70%, and it is 100% for grade 3 pneumothoraces. Thorax ultrasonography successfully detected all grade 3 pneumothoraces. Notably, Thorax ultrasonography is a valuable technique that poses no risk of exposure to ionizing radiation, enabling emergency unit physicians to accurately assess unstable patients at the bedside. However, the sensitivity dramatically decreases when the size of the pneumothorax is below 1 cm.
References
Crawford WO Jr (1973) Pulmonary injury in thoracic and non-thoracic trauma. RaioClin North Am 11:527
Clark GC, Schecter WP, Trunkey DD (1988) Variables affecting outcome in blunt chest trauma: flail chest vs. pulmonary contusion. J Trauma 28(3):298–304
Cameron P, Dziukas L, Hadj A et al (1996) Rib fractures in major trauma. Aust N Z J Surg 66:530–534
LoCicero J 3rd, Mattox KL (1989) Epidemiology of chest trauma. Surg Clin North Am 69.1:15–19
Altunkaya A, Aktunc E, Kutluk AC et al (2007) Analysis of 282 patients with thoracic trauma. Turk J Thorac Cardiovasc Surg 15:127–132
Graeber GM, Prabhakar G, Shields T (2005) Blunt and penetrating injuries of the chest wall, pleura and lungs. In: Shields TW, LoCicero J 3rd, Ponn RB, Rusch VW (eds) General thoracic surgery, 6th edn. Lippincott Williams & Wilkins, Philadelphia, pp 951–972
Magu S, Yadav A, Agarwal S (2009) Computed tomography in blunt chest trauma. Indian J Chest DisAlliedSci Apr-Jun 51(2):75–81
Kaewlai R, Avery LL, Asnari AV et al (2008) Multi detector CT of blunt thoracic trauma. Radiographics 28:1555–1570
Kelly AM, Weldon D, Tsang AY et al (2006) Comparison between two methods for estimating pneumothorax size from chest X-rays. RespirMed 100(8):1356–1359
Rowan KR, Kirkpatrick AW, Liu D et al (2002) Traumatic pneumothorax detection with thoracic US: correlation with chest radiography and CT-initial experience. Radiology 225:210–214
Lichtenstein DA, Mezière G, Lascols N et al (2005) Ultrasound diagnosis of occult pneumothorax. CritCareMed 33(6):1231–1238
Çevik AA, Ergün N, Sivrikoz C et al (2006) Diagnosis of pneumothorax by ultrasonography. Turk J EmergMed 6(4):176–180
Kirkpatrick AW, Sirois M, Laupland KB, Liu D, Rowan K, Ball CG et al (2004) Hand-held thoracic sonography for detecting post-traumatic pneumothoraces: the Extended Focused Assessment with Sonography for Trauma (EFAST). J Trauma 57:288–295
Dente CJ, Ustin J, Feliciano DV, Rozycki GS, Wyrzykowski AD, Nicholas JM et al (2007) The accuracy of thoracic ultrasound for detection of pneumothorax is not sustained over time: a preliminary study. J Trauma 5(62):1384–1389
Lichtenstein D, Van Hooland S, Elbers P, Malbrain MLNG (2014) Ten good reasons to practice ultrasound in critical care. AnaesthesiolIntensiveTher 46:323–335. https://doi.org/10.5603/AIT.2014.0056
Uz I, Yürüktümen A, Boydak B, Bayraktaroğlu S, Ozçete E, Cevrim O et al (2013) Impact of the practice of “Extended Focused Assessment with Sonography for Trauma” (e-FAST) on clinical decision in the emergency department. Ulus Travma Acil Cerrahi Derg 19(4):327–332
Wolfman NT, Myers WS, Glauser SJ, Meredith JW, Chen MYM (1998) Validity of CT classification on management of occult pneumothorax: a prospective study. AJR Am J Roentgenol 171:1317–20
Soldati G, Testa A, Sher S et al (2008) Occult traumatic pneumothorax: Diagnostic accuracy of lung ultrasonography in the emergency department. Chest 133:204–211
Trupka A, Waydhas C, Hallfeldt KK, Nast-Kolb D, PfeiferKJ Schweiberer L (1997) Value of thoracic computed tomography in the first assessment of severely injured patients with blunt chest trauma: results of a prospective study. J Trauma 43:405–11
Ding W, Shen Y, Yang J et al (2011) Diagnosis of pneumothorax by radiography and ultrasonography: a meta-analysis. Chest 140:859–866
Mackenzie DC, Azad AM, Noble VE, Liteplo AS (2019) Test performance of point-of-care ultrasound for gastric content. Am J Emerg Med 37(1):123–126
Blaivas M, Lyon M, Duggal S (2005) A prospective comparison of supine chest radiography and bedside ultrasound for the diagnosis of traumatic pneumothorax. Acad Emerg Med 12:844–849
Zhang M, Liu ZH, Yang JX, Gan JX, Xu SW, You XD et al (2006) Rapid detection of pneumothorax by ultrasonography in patients with multiple trauma. Crit Care 10:R112
Funding
Open Access funding provided by the Qatar National Library.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
A.T, H.D., M.A.E and Y.Y reports no conflict of interest.
A.T, H.D., M.A.E and Y.Y no financial disclosure was declared by the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Temel, A., Doğan, H., Erduhan, M.A. et al. Does Ultrasound Really Good Enough to Evaluate the Pneumothorax in the Emergency Department. Indian J Surg (2023). https://doi.org/10.1007/s12262-023-03895-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12262-023-03895-w