Abstract
Malignant melanoma is an aggressive neoplasm with a high tendency to metastasize.
Gastrointestinal metastases, although described in the literature, are infrequent. We present the case of a 51-year-old male patient with a surficial spreading melanoma stage IIIc with BRAF mutation who presented a gallbladder outgrowth lesion, compatible with a polyp. A significant growth of the lesion was observed in subsequent TC studies and a laparoscopic cholecystectomy was performed. The anatomopathological study of the specimen confirmed the diagnosis of gallbladder metastasis due to epithelioid and spindle cell malignant melanoma. The presence of a gallbladder lesion in the context of a patient diagnosed with melanoma should establish the diagnostic suspicion of metastasis, and an early extension study and laparoscopic cholecystectomy should be considered. The palliative surgical approach to avoid hepatobiliary symptomatology can be considered.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
A 51-year-old male patient with a melanocytic lesion in the left lumbar region was biopsied, confirming the histopathological diagnosis of superficial spreading melanoma pT4bM2b M0 (stage IIIc) with BRAF mutation. Further surgery was indicated to widen the margins and a selective biopsy of the sentinel lymph node was performed, which showed metastasis without extracapsular invasion. Left inguinal lymphadenectomy was proposed. Two months earlier, the patient had presented an episode of acute diverticulitis, for which reason an abdominal computed axial tomography was requested. The CT scan showed a normal-sized gallbladder with a 13-mm outgrowth lesion, compatible with a gallbladder polyp. The tomography was repeated prior to the lymphadenectomy, where a significant growth of the gallbladder lesion up to 30 mm was observed (Fig. 1). The patient had no digestive symptoms at any time, and the hepatobiliary and pancreatic profiles showed no analytical alterations.
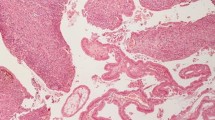
Given the findings, it was decided to perform a concomitant laparoscopic cholecystectomy at the same surgical time, which was carried out without incident. The anatomopathological study of the specimen confirmed the diagnosis of gallbladder metastasis due to epithelioid and spindle cell malignant melanoma (Fig. 2). The lymphadenectomy study showed 18 lymph nodes, all of them without tumor infiltration. Subsequently, an extension study was performed by PET-TAC, which showed involvement of a presacral ganglion and a single bone metastasis in the left iliac bone. It also showed hypermetabolic foci in the right prostatic lobe, of uncertain significance. The patient is alive and is undergoing oncological treatment with pembrolizumab.
Histological section of the gallbladder. Microphotography (H-E. × 10): biliary cylindrical epithelium is observed, infiltrated by melanocytic cells. The accompanying stroma is also infiltrated by this proliferation of large, atypical cells, with a large cytoplasm loaded with pigment and presence of a central and hyperchromatic nucleus of irregular contour
Malignant melanoma is an aggressive neoplasm with a high tendency to metastasize. Gastrointestinal metastases, although described in the literature, are infrequent [1]. Regarding gallbladder metastases, there are only a few isolated reports in the scientific literature, and there is no consensus on optimal management. A recent review showed that 60% of the metastases present in the gallbladder correspond to malignant melanoma. The most probable route of dissemination is hematogenous, although dissemination via the biliary route cannot be excluded [1]. In series of autopsies performed on patients with melanoma, up to 20% of metastases have been found in the gallbladder, but the proportion of these patients diagnosed during life is much lower. This is probably related to the fact that gallbladder metastases are in most cases asymptomatic [1]. Although there are reports of high survival rate at 1-year follow-up after surgery in single gallbladder malignant melanoma metastasis [2], these results are different from those reported in other series. This seems to be related to the fact that in most patients in whom gallbladder metastases are found, the disease is widespread. Given these findings, it seems reasonable to consider laparoscopic cholecystectomy in patients with localized and resectable disease [3].
In conclusion, melanoma metastases in the gallbladder are infrequent and constitute a diagnostic and therapeutic challenge. The presence of a gallbladder lesion in the context of a patient diagnosed with melanoma should establish the diagnostic suspicion of metastasis, and an early extension study and laparoscopic cholecystectomy should be considered. The palliative surgical approach to avoid hepatobiliary symptomatology can be considered (including biliary stenting and cholecystostomy), although the decision must be individualized.
References
Giannini I, Cutrignelli DA, Resta L, et al. (2016) Metastatic melanoma of the gallbladder: report of two cases and a review of the literature. Clinical and experimental medicine 16(3). Springer Milan: 295–300. https://doi.org/10.1007/s10238-015-0353-6.
Dong XD, DeMatos P, Prieto VG, Seigler HF (1999) Melanoma of the gallbladder: a review of cases seen at Duke University Medical Center. Cancer 85:32–39
Katz SC, Bowne WB, Wolchok JD, Busam KJ, Jaques DP, Coit DG (2007) Surgical management of melanoma of the gallbladder: a report of 13 cases and review of the literature. Am J Surg 193:493–497
Funding
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
After consultation, the institutional board review of our center does not require evaluation of individual clinical cases or retrospective studies based on isolated cases. All the information in this document has been anonymized in accordance with current legislation and does not allow patient recognition.
Consent to Participate
Prior to the submission of this article, verbal and written informed consent was obtained from the patient whose clinical photographs are included in this publication. The patients’ medical records were accessed in accordance with the specific hospital regulations applicable to this type of case.
Consent for Publication
All authors of the manuscript declare that it is an original contribution, not previously published, and that at the present time it has not been sent to any other journal to assess its publication.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Arredondo Montero, J., Recreo Baquedano, A., Bronte Anaut, M. et al. Metastasis of Spindle Cell Malignant Melanoma in Gallbladder. Indian J Surg 85, 433–435 (2023). https://doi.org/10.1007/s12262-022-03379-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-022-03379-3